* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ischemic strokes
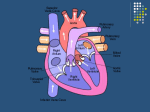
Management of acute coronary syndrome wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Jatene procedure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Stroke: Ischemic strokes: Stroke Risk Factors: What Patients and Families Should Know Evaluating the risk for stroke is based on heredity, natural process and lifestyle. Many risk factors for stroke can be changed or managed, while others that relate to hereditary or natural processes cannot be changed. Risk factors that you and your health care provider can change, treat or control: High blood pressure – The most important controllable risk factor for stroke is controlling high blood pressure. In an adult, high blood pressure is defined as a systolic pressure of 140mm Hg or higher and /or a diastolic pressure of 90 mm Hg or higher for an extended time. Goal blood pressure is 120/80mm Hg. High blood cholesterol and lipids – High blood cholesterol and lipids increase the risk for stroke. Diet: diets high in salt can increase blood pressure. Excess calories lead to obesity. Fruits and veggies can decrease risk of stroke. A poor diet has lots of saturated fats and/or trans fats. Diabetes mellitus – Diabetes is treatable, but having it increases the risk for stroke. Atrial fibrillation – This heart rhythm disorder raises the risk for stroke because the heart’s upper chambers quiver instead of beating effectively. This lets the blood pool and clot. If a clot breaks off, enters the blood stream and lodges in an artery leading to the brain, a stroke results. Carotid and other artery disease – The carotid arteries in the neck supply blood to the brain. When the carotid arteries are narrowed by atherosclerosis (plaque in artery walls), they may become blocked by a blood clot. People with peripheral artery disease (narrowed blood vessels in legs/arms) have a higher risk of carotid artery disease, which raises their risk of strokes. Other heart disease – People with coronary heart disease or heart failure have a higher risk of stroke as those with hearts that work normally. Dilated cardiomyopathy (an enlarged heart), heart valve disease and some types of congenital heart defects may also increase the chance of stroke. Certain blood disorders – A moderate increase in the number of red blood cells thickens the blood and makes clots more likely, thus increasing the risk of stroke. Sickle cell anemia increases risk of stroke because the “sickled” cells tend to stick to vessel walls, which can block arteries to the brain, causing a stroke. Physical inactivity and obesity – Being inactive and/or obese can increase your risk of high blood pressure, high blood cholesterol, diabetes, heart disease and stroke. Cigarette smoking – Smoking is the number one preventable risk factor for stroke. The nicotine and carbon monoxide in tobacco smoke reduce the amount of oxygen in your blood. They also damage the walls of blood vessels, making clots more likely to form. Using some kinds of birth control pills combined with smoking cigarettes greatly increases stroke risk. Excessive alcohol use – More than two drinks per day in men, or more than 1 drink/day in women is considered excessive. This can raise blood pressure, and binge drinking can lead to stroke. Illegal drug abuse – Intravenous drug abuse carries a high risk of stroke. Cocaine, amphetamine, and heroin use have been linked to strokes and heart attacks. Some have been fatal even in first-time users. IT IS VERY important that you follow up with your Primary Care Physician soon after your discharge from the hospital to continue addressing your controlable risk factors for stroke. Risk factors for stroke that cannot be changed: Age – Stroke happens to people of all ages, including children. But the older you are, the greater your risk for stroke. Sex (gender) – Stroke is more common in men than women. However, more women than men die of strokes. Use of birth control pills and pregnancy pose special risks for women. Heredity (family history) and race – The chance of stroke is greater for someone whose parent, grandparent, sister or brother has had a stroke. African Americans have a much higher risk of death and disability from a stroke than Caucasians do, in part because the African American population has a greater incidence of high blood pressure. Prior stroke, TIA, or MI increases risk of another stroke. A TIA is a “warning stroke” that does not cause long-term damage but is a strong predictor of future stroke. Recognizing and treating TIAs can reduce the risk of a major stroke. It is very important to recognize the warning signs of a TIA or stroke. Call 9-1-1 to get medical help immediately if they occur! Do not take these lightly! Virginians live in part of the “stroke belt”; strokes are more common in the Southeastern United States than in any other part of the country. STROKE TESTS: What patients and families should know Advances in technology now make it possible to examine how the brain looks, functions and get its blood supply. These tests can outline the affected part of the brain and help define the problem created by stroke. WHAT IMAGING TESTS MAY BE DONE? Computerized Tomography (CT or CAT scan) is a test that uses a combination of x-rays and computer technology to produce pictures of the brain and neck. For a CT Scan, the patient is placed flat on the x-ray table with their head placed inside the scanner. The patient is asked to remain very still. Sometimes, a CT Angiogram (CTA) is done to look at the blood vessels of the brain and neck. To do this an IV line will be placed and contrast dye will be injected as the pictures are taken. The time required to do the CT scan varies, but is usually about 15 minutes. Additional time is required for the patient to travel to and from the radiology department. Magnetic Resonance Imaging (MRI/MRA, DWI) is a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of the brain and other parts of the body. During a MRI the patient will be asked to lie flat and still on a narrow table inside the round opening of a large magnet. During the exam, humming and clicking sounds will be heard as the images are taken. Because the MRI uses a magnet to produce pictures, a worksheet is completed by the patient or family to screen for metal prior to the MRI. The opening to the MRI scanner is small and makes some people feel claustrophobic, so medications may be given to help the patient relax during the MRI. The length of time needed for the MRI varies a lot depending on the type of pictures needed. Carotid Doppler ultrasound test uses high-frequency sound waves to detect blockages in the carotid arteries that feed blood to the brain. A probe is placed on the patient’s neck and ultrasound images are taken. This test may be done at the patient’s bedside or in a special room in the radiology department. Cerebral Angiography (A-gram) is a test that injects dye into the cerebral arteries, providing information about the blood vessels of the brain. A thin tube (catheter) is placed in the large artery of the leg and fed up to the neck and head. Dye is injected to outline the blood vessels. Several injections are required. After each injection of dye, x-rays are taken to look at the circulation of the blood in the brain. After the test, the catheter is removed from the leg and pressure is applied to the insertion site. The patient must lie still for several hours after the test is completed. Echocardiogram (ECHO) is a test that uses ultrasound (high-frequency sound waves) to produce moving images of the heart beating on a video screen, evaluating the heart size and valves. One cause of stroke is a clot forming in the heart and then traveling to the brain, so an echo is often ordered on patients after a stroke. APHASIA: What Patients and Families Should Know What is aphasia? Aphasia is defined as a language disorder that usually results from damage to the left side or hemisphere of the brain. Depending on what area of the brain has been damaged, there may be differences in the type of aphasia. Aphasia usually occurs suddenly, with a stroke or brain injury, but can occur slowly, in the case of a brain tumor. Some people with aphasia have difficulty with expression of language (expressive aphasia), some have difficulties understanding language (receptive aphasia) and others have difficulties with both areas (global aphasia). Aphasia can also cause difficulties with reading and writing. It is estimated that about 1 million people in the United States have aphasia. Not all strokes cause aphasia, but about 20% of people who have strokes suffer a serious loss of speech and language. Some people recover quickly, while others will have permanent difficulties. A speech-language pathologist (SLP) works with patients to help rehabilitate speech and language function. How can I help communicate with an aphasic person? Remember that the patient’s intelligence has not decreased. Always keep in mind that the aphasia is probably very frustrating for the patient too, and s/he is trying to communicate effectively. General Guidelines: Try to communicate in a quiet environment with no distractions (turn off the TV, radio, and limit the number of people talking at one time). Do not use baby talk, talk to the person in a normal tone, loudness, and intonation. Use shorter, simple statements and questions, rephrase if the person does not understand. You can pause often when talking, giving the person time to understand and respond. Use other forms of communication to reinforce your words (i.e. gestures, facial expressions, pointing, written words, and pictures). Accept any form of communication from the person with aphasia. When asking a question to the person you can use YES and NO questions, give them choices, or use pictures to reinforce your words. If the person is having trouble speaking (expressive aphasia): phrase questions in such a way that s/he can answer yes or no avoid pressuring him/her; give additional time for responses encourage gesturing/pointing do not interrupt the patient when s/he is trying to speak; avoid the temptation to talk for him/her if s/he is trying to get his/her words out if you are not sure exactly what s/he said, ask if your interpretation is correct if you do not understand a message, begin by asking broad yes/no questions, and then narrow the topic with more specific yes/no questions (for example, “Does something hurt?” “Is it your leg?,” “Is it your stomach?,” “Is it your head?”) if the patient can write or draw what s/he can not say, provide him/her with a pad and pencil remember that s/he can probably understand what is being said; do not talk about the patient as if s/he is not present If the person is having trouble understanding (receptive aphasia): use short statements and questions; keep explanations short and simple speak slowly and give him/her additional time to process what you say look directly at the patient when speaking if the patient fails to understand you, try repeating or rewording what you have said only one person should speak to the patient at a time; turn off TV and radio accompany your words with gestures, objects or pictures if possible keep the topics you discuss with the patient relevant and familiar so that s/he can relate to what you say NEGLECT: What Patients and Families Should Know What is neglect? Neglect frequently occurs when someone has a stroke in the right side of their brain. Generally speaking, neglect is just that – inattention of their body, things or people on the left side. (Some people neglect their right side but this is less common; if this is the case with your family member, switch right with left in the information written below.) Problems that result from neglect can range from mild to severe. The more fortunate individuals are aware of it and can make conscious efforts to compensate for it. Some, however, are completely unaware they have this deficit. What are the symptoms of neglect? Paying less attention to their left side Difficulty finding things on the left Unable to look or turn to the left Unable to recognize one’s left arm or leg as their own Ignoring (though not on purpose) anything or anyone to their left Only eating things on the right side of their plate Difficulty or fear of moving about in crowded areas Startled by moving objects or people Forgetting to dress the left side of the body Bumping into doorways or objects on the left Missing words on the left side of a page when reading or frequently losing one’s place Below is a clock that was drawn by someone with left neglect How is neglect treated? Like other symptoms associated with a stroke, neglect can improve. Unfortunately, there is no medicine or simple cure for neglect. Symptoms can improve over time; to what extent depends on the amount of damage in the brain. Those who are aware that they have neglect do best. What can I do to help someone with neglect? The affected person should be encouraged to attend to the left side of their body and the environment. Approach them from the left whenever possible, and encourage them to look at you when you are speaking. Provide as much stimulation to the affected side as he or she can tolerate! Other tips: Constantly remind the person to turn their head and “look to the left” for lost objects, this is especially important when walking or eating Help them complete the exercises given to them by their physical therapist (PT) or occupational therapist (OT). Place items that the person finds motivating (pictures, TV, drinks/snacks) on the left. Encourage the person to attend to their neglected side by positioning their arm/leg when turning in bed, sitting in chair, and when performing self- care activities-ask nursing or OT/PT if you need guidance. People who have neglect should not drive! Please remember that neglect can have serious safety implications, especially if the person is unaware of their deficits. What’s the take-home message? If you need to have an important conversation with a person who has left neglect speak with them on their right side to ensure they are attending to you. They will be more likely to remember it. However, for general conversation with someone who has neglect, spend at least part of your time on their left side. Place items that are important to the person on the left to encourage them to look and reach to the left. Educating the individual with neglect is important! Stroke Websites and support groups: http://www.healthsystem.virginia.edu/docs/per/stroke-websites-and-supportgroups/at_download/perdocument