* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Progressive Caloric Restriction Induces Dose
Survey
Document related concepts
Transcript
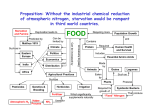
ORIGINAL ARTICLE E n d o c r i n e C a r e Progressive Caloric Restriction Induces DoseDependent Changes in Myocardial Triglyceride Content and Diastolic Function in Healthy Men Sebastiaan Hammer,* Rutger W. van der Meer,* Hildo J. Lamb, Michael Schär, Albert de Roos, Jan W. A. Smit, and Johannes A. Romijn Departments of Endocrinology and Metabolism (S.H., R.W.v.d.M., J.W.A.S., J.A.R.) and Radiology (S.H., R.W.v.d.M., H.J.L., A.d.R.), Leiden University Medical Center, 2300 RC Leiden, The Netherlands; Russell H. Morgan Department of Radiology and Radiological Science (M.S.), Johns Hopkins University School of Medicine, Baltimore, Maryland 21287; and Philips Medical Systems (M.S.), Cleveland, Ohio 44106 Context: In animal experiments, high plasma concentrations of free fatty acids (FFAs) are associated with increased triglyceride (TG) stores in liver and heart, and impaired cardiac function. In humans caloric restriction increases plasma FFA levels. Objective: Our objective was to assess the effects of progressive caloric restriction on myocardial and hepatic TG content and myocardial function. Design: This was a prospective intervention study. Participants: This study included 10 lean healthy men. Interventions: Three-day partial (471 kcal/d) and complete starvation was performed. Outcome Measures: Plasma levels of FFA, myocardial and hepatic TG content, and myocardial function were calculated. Results: Plasma FFA increased from 0.6 ⫾ 0.4 mmol/liter to 1.2 ⫾ 0.4 and to 1.9 ⫾ 0.7 mmol/liter, after partial and complete starvation, respectively (P ⬍ 0.001). Myocardial TG content increased from 0.35 ⫾ 0.14% to 0.59 ⫾ 0.27%, and 1.26 ⫾ 0.49%, respectively (P ⬍ 0.01). The ratio between the early diastole and atrial contraction decreased from 2.2 ⫾ 0.4 to 2.1 ⫾ 0.4 (P ⫽ 0.7) and 1.8 ⫾ 0.4, respectively (P ⬍ 0.01), and diastolic early deceleration from 3.4 ⫾ 0.7 ml/sec2 ⫻ 10⫺3 to 2.9 ⫾ 0.5 and 2.8 ⫾ 0.9 ml/sec2 ⫻ 10⫺3, respectively (P ⬍ 0.05). Hepatic TG content decreased after partial starvation (from 2.23 ⫾ 2.24% to 1.43 ⫾ 1.33%; P ⬍ 0.05) but did not change upon complete starvation. Conclusions: Progressive caloric restriction induces a dose-dependent increase in myocardial TG content and a dose-dependent decrease in diastolic function in lean healthy men. Hepatic TG content showed a differential response to progressive caloric restriction, indicating that redistribution of endogenous TG stores is tissue specific. (J Clin Endocrinol Metab 93: 497–503, 2008) lmost all endogenous triglycerides (TGs) are stored in adipose tissue to accommodate discrepancies between whole body fat uptake and fat oxidation. However, a very small A proportion is stored in nonadipose tissues like the heart (1), the liver (2), and skeletal muscle (3), especially in obesity and type 2 diabetes mellitus. There are indications that this storage of TG in 0021-972X/08/$15.00/0 Abbreviations: A, Atrial contraction; BMI, body mass index; E, early diastole; ECG, electrocardiogram; FA, fatty acid; FFA, free FA; LVEF, left ventricular ejection fraction; MRI, magnetic resonance imaging; MRS, magnetic resonance spectroscopy; ppm, parts per million; TC, total cholesterol; TE, echo time; TG, triglyceride; TR, repetition time; VLDL, very low density lipoprotein. Printed in U.S.A. Copyright © 2008 by The Endocrine Society doi: 10.1210/jc.2007-2015 Received September 7, 2007. Accepted November 13, 2007. First Published Online November 20, 2007 * S.H. and R.W.v.d.M. contributed equally. J Clin Endocrinol Metab, February 2008, 93(2):497–503 jcem.endojournals.org 497 498 Hammer et al. Myocardial TG Content and Diastolic Function nonadipose tissues is not merely an inert phenomenon but is associated with more or less subtle physiological changes in organ-specific functioning (4 – 8). In animal models there is an inverse relation between myocardial TG content and myocardial function. For example, myocardial lipid accumulation is associated with a decrease in left ventricular systolic function in obese Zucker rats, and treatment with thiazolidinediones reduces myocardial TG content and improves left ventricular function (8). The underlying mechanisms of the decrease in left ventricular function are complex and are related to effects of fatty acid (FA) derivatives, like fatty acyl-coenzyme A, ceramides, and diacylglycerol (4, 5, 7). High plasma concentrations of free fatty acids (FFAs) may result in excessive FA uptake in nonadipose tissues, such as the liver and heart, which may affect normal organ function (7, 8). However, in humans the relation between myocardial TG accumulation and myocardial function was difficult to study by noninvasive methods because measurement of myocardial TG content is challenging due to artifacts induced by cardiac and respiratory motion. Recently, proton magnetic resonance spectroscopy (MRS) of the heart was developed that enables the measurement of myocardial TG content in humans in vivo (1, 10 –13). Using this method, Reingold et al. (14) documented that fasting for 48 h increases plasma FFA levels and myocardial TG content in healthy subjects, whereas myocardial TG content did not change after a single high fat meal. In another, cross-sectional study, Kankaanpää et al. (12) showed that increased levels of plasma FFA in obese subjects correlate positively with myocardial TG content and inversely with cardiac function. However, both studies did not address the relation between myocardial function in relation to myocardial TG content within the same subjects. In a recent study, we documented that the use of a very low calorie diet increases plasma FFA and myocardial TG content, associated with a decrease in myocardial diastolic function (15). Therefore, it appears that myocardial TG content is not fixed but varies within the same subject according to physiological conditions. It is yet unknown whether our recent findings of myocardial flexibility can be extrapolated when caloric restriction is progressively increased. Therefore, the aim of the present study was to extend the conditions of partial caloric restriction to complete caloric restriction, i.e. complete starvation. For this purpose we compared baseline observations with those obtained after 3-d partial starvation (471 kcal/d) and after 3-d complete starvation with respect to plasma levels of FFA, myocardial TG content, myocardial function, and hepatic TG content. J Clin Endocrinol Metab, February 2008, 93(2):497–503 was performed. An electrocardiogram (ECG) was made during the first visit. Subjects with any aberrations on the ECG were excluded. In addition, a 2-h 75 g oral glucose tolerance test was performed in the fasted state, to exclude subjects suffering from diabetes mellitus (17). Other exclusion criteria were: obesity (BMI ⬎ 30 kg/m2); liver disease (increased plasma levels of alanine aminotransferase, aspartate aminotransferase, and/or ␥-glutamyl transferase ⬎ 2 SD above the reference value of our institution); renal disease (defined by plasma creatinine levels ⬎ 2 SD above the reference value of our institution); use of any medication; and a history of (congenital) heart disease. Specifically, subjects with prior or present coronary artery disease (based on medical history) or hypertension (defined as sitting systolic blood pressure ⬎ 130 mm Hg and/or diastolic blood pressure ⬎ 85 mm Hg) were excluded. Written informed consent was obtained from all participants before the study. The local ethics committee approved the study. Study design The study consisted of three conditions. Baseline measurements were made, while subjects followed a normal diet but abstained from alcohol for 3 d (mean intake 2065 kcal/d). Subjects were admitted 4 h after the last meal for measurement of plasma concentrations of glucose, insulin, and lipids, and for evaluation by magnetic resonance imaging (MRI) and MRS. The second measurement was performed after a 3-d period of partial caloric restriction (471 kcal/d; Modifast Intensive, Nutrition & Santé Benelux, Breda, The Netherlands). The third measurement was performed after a 3-d period of complete starvation (0 kcal/d, only water was allowed), after which subjects were again admitted for blood sampling and MRI/MRS evaluation. Plasma concentrations of FFA and insulin were used to assess study compliance (18). Between all study occasions, a washout period with a minimum of 14 d was acquired (19), and the sequence of the second and third occasions was determined by balanced assignment. 1 H-MRS of the liver and the heart All MRI/MRS measurements were performed on a 1.5-Tesla Gyroscan ACS-NT MRI scanner (Philips Medical Systems, Best, The Netherlands) in the supine position. Localized single voxel (2 ⫻ 2 ⫻ 2 cm for the liver and 2 ⫻ 4 ⫻ 1 cm for the heart) spectra were recorded using a body coil for radiofrequency transmission and a surface coil (Ø 17 cm) for signal receiving. For the heart, the spectral volume was placed in the interventricular septum on four-chamber and short axis images at end systole, avoiding contamination with epicardial fat (Fig. 1). Data collection was double triggered using ECG triggering and navigator echoes for compensation of respiratory motion as described earlier (13). For the liver, voxel sites were matched at both study occasions, carefully avoiding blood vessels and bile ducts. To detect weak lipid signals, watersuppressed spectra with 128 averages for the heart and 64 for the liver were collected. Spectral parameters were: a repetition time (TR) of 3000 msec, echo time (TE) of 26 msec, and 1024 data points over 1000 kHz spectral width. In the same voxel, using the same parameters except for a TR of 10,000 msec, unsuppressed spectra with four averages were collected. Spectra were analyzed in the time domain, using Java-based MR user interface software and prior knowledge files [version 2.2 (20)], as described earlier (13). Peak estimates of lipid resonances of myocardial TG at 1.3 parts per million (ppm) and 0.9 ppm were summed and calculated as a percentage of the unsuppressed water signal (TG content, TG/water ⫻100). Subjects and Methods MRI of the heart Subjects There were 10 nonsmoking, healthy men included in this study [age; mean ⫾ SD: 23.7 ⫾ 4.7 yr, range 20.8 –36.0 yr; body mass index (BMI): 23.6 ⫾ 0.9 kg/m2]. Women were excluded because the hormonal status or contraceptive use may affect lipid metabolism (16). The study population was partly based on a previous cohort (15). In each subject, medical history was obtained, and physical examination Imaging of the heart was performed using a body coil for radiofrequency transmission and a five-element synergy coil for signal receiving. To assess systolic function, the heart was imaged from apex to base with 12–14 imaging levels (dependent on the heart size) in short axis view using an ECG triggered, sensitivity encoding balanced steady-state free procession sequence. Imaging parameters were a field-of-view of 400 mm, a matrix size of 256 ⫻ 256, a slice thickness J Clin Endocrinol Metab, February 2008, 93(2):497–503 jcem.endojournals.org 499 Left ventricular ejection fraction (LVEF) was calculated for the assessment of systolic function. Furthermore, an ECG-gated gradientecho sequence with velocity encoding was performed to measure blood flow across the mitral valve for the determination of left ventricular diastolic function (22, 23). Imaging parameters included the following: a TE of 5 msec, a TR of 14 msec, a flip angle of 20°, a slice thickness of 8 mm, a field-of-view of 350 mm, a matrix size of 256 ⫻ 256, a velocity encoding of 100 cm/sec, and a scan percentage of 80%. Flow velocities in early diastole (E) and at atrial contraction (A) were measured, and their peak flow ratio was calculated (E/A ratio) using the FLOW analytical software package (Medis) by defining a region of interest on the modulus images in all cardiac phases. Furthermore, the mean deceleration of the E wave and an estimation of left ventricular filling pressures (E/Ea) (24) were measured. All spectroscopic and functional analyses were performed by an experienced observer, blinded to the interventions. During MRI, blood pressure and heart rate were measured twice with an automatic device (Dinamap DPC100X; Freiburg, Germany) and averaged for analysis. Assays Glucose, total cholesterol (TC), and TG were measured on a fully automated P800 analyzer (Roche, Almere, The Netherlands) and insulin on a Immulite 2500 random access analyzer with a chemoluminescence immunoassay (Diagnostic Products Corp., Los Angeles, CA). Coefficients of variation were less than 2% for glucose, TC, and TG, and less than 5% for insulin. Plasma FFAs were measured using a commercial kit (FFA-C; Wako Chemicals, Neuss, Germany). Statistical analysis All statistical analyses were performed using SPSS, version 12.01 (SPSS, Inc., Chicago, FIG. 1. Myocardial spectroscopic volume. Localization of the myocardial spectral voxel in the fourIL). Statistical comparisons among the three chamber (A) and short axis views (B). physiological conditions were made by repeated measures ANOVA. Pearson r values were used for correlation analysis. Data are of 10 mm, a slice gap of 0 mm, a flip angle of 35°, a TE of 1.67 msec, shown as mean ⫾ SD. P ⬍ 0.05 (two tailed) was considered significant. and a TR of 3.34 msec. Temporal resolution was 25–39 msec. End Based on a previous report, we expected a decrease in diastolic early diastolic and end systolic images were identified on all slices, and deceleration. Therefore, P ⬍ 0.05 (one tailed) was considered signifendocardial contours were drawn using MASS post processing softicant for this parameter (15). ware (Medis, Leiden, The Netherlands) as described previously (21). TABLE 1. Metabolic response to progressive caloric restriction Plasma concentrations Glucose (mmol/liter) Insulin (mU/liter) FFAs (mmol/liter) TGs (mmol/liter) TC (mmol/liter) Baseline Partial starvation Complete starvation 5.0 ⫾ 0.3 10.1 ⫾ 5.3 0.6 ⫾ 0.4 1.3 ⫾ 0.4 5.0 ⫾ 1.3 4.3 ⫾ 0.4a 8.0 ⫾ 3.7 1.2 ⫾ 0.4b 0.9 ⫾ 0.3a 5.1 ⫾ 1.4 3.9 ⫾ 0.5a 3.0 ⫾ 1.8a 1.9 ⫾ 0.7b 1.3 ⫾ 0.6 5.9 ⫾ 1.8a Data are mean ⫾ SD. Blood samples were collected 4 h after the last meal. a P ⬍ 0.01 vs. baseline. b P ⬍ 0.001 vs. baseline. 500 Hammer et al. Myocardial %TG (relative to baseline) A Myocardial TG Content and Diastolic Function J Clin Endocrinol Metab, February 2008, 93(2):497–503 associated with a dose-dependent decrease in plasma insulin levels. Simultaneously, plasma concentrations of FFA increased dose dependently from 0.6 ⫾ 0.4 mmol/liter to 1.2 ⫾ 0.4 mmol/liter after partial (P ⬍ 0.001) and to 1.9 ⫾ 0.7 mmol/liter after complete starvation (P ⬍ 0.001). Plasma TG levels decreased after partial starvation (from 1.3 ⫾ 0.4 mmol/liter to 0.9 ⫾ 0.3 mmol/liter (P ⫽ 0.009) but did not change upon complete starvation (P ⫽ 0.677). TC increased from 5.0 ⫾ 1.3 mmol/liter at baseline to 5.1 ⫾ 1.4 mmol/liter after partial (P ⫽ 0.810) and to 5.9 ⫾ 1.8 mmol/liter after complete starvation (P ⫽ 0.005). 4 3 2 Triglycerides 1 Creatine 0 1.3 baseline 1.3 partial starvation 1.3 complete starvation B 2.5 Myocardial TG (%) 2.0 1.5 * ppm Effects of progressive caloric restriction on myocardial and hepatic TG content Myocardial TG content increased dose dependently from 0.35 ⫾ 0.14% at baseline to 0.59 ⫾ 0.27% after partial (P ⫽ 0.006) and to 1.26 ⫾ 0.49% after complete starvation (P ⬍ 0.001; Fig. 2). Hepatic TG content correlated with BMI at baseline (r ⫽ 0.67; P ⫽ 0.033). Hepatic TG content significantly decreased after partial starvation (from 2.24 ⫾ 2.24% to 1.43 ⫾ 1.33%; P ⫽ 0.031), whereas it did not change after complete starvation (2.54 ⫾ 2.53%; P ⫽ 0.378; Fig. 3). Effects of progressive caloric restriction on myocardial function (Table 2) 1.0 Systolic and diastolic blood pressure, heart rate, and myocardial LVEF did not * change significantly during/after partial and complete starvation, compared with 0.5 baseline. Furthermore, estimated left ventricular filling pressures were unchanged after partial (8.8 ⫾ 3.8; P ⫽ 0.742) and complete starvation (8.2 ⫾ 2.5; P ⫽ 0.299) 0 baseline partial complete compared with baseline (9.3 ⫾ 2.6). Diastarvation starvation stolic E/A ratio decreased dose dependently FIG. 2. Myocardial TG content at baseline, and after partial and complete starvation. Typical from 2.2 ⫾ 0.4 at baseline to 2.1 ⫾ 0.4 after proton spectra of myocardial TG content of one subject at baseline, and after partial and complete partial starvation (P ⫽ 0.687) and to 1.8 ⫾ starvation scaled relative to baseline (A) and individual changes in myocardial TG content upon complete starvation (n ⫽ 10) (B). Vertical lines represent mean ⫾ SD. *, P ⬍ 0.01 vs. baseline. 0.4 after complete starvation (P ⫽ 0.005). E deceleration decreased dose dependently from 3.4 ⫾ 0.7 ml/sec2 ⫻ 10⫺3 at baseline Results ⫺3 to 2.9 ⫾ 0.5 ⫻ 10 ml/sec2 after partial (P ⫽ 0.036) and to 2.8 ⫾ 0.9 after complete starvation (P ⫽ 0.032). Metabolic effects of progressive caloric restriction (Table 1) Subject characteristics at baseline, after partial starvation, and after complete starvation are shown in Table 1. Postabsorptive Discussion plasma glucose levels decreased from 5.0 ⫾ 0.3 mmol/liter at baseline to 4.3 ⫾ 0.4 mmol/liter after partial (P ⫽ 0.001) and to 3.9 ⫾ This study demonstrates that progressive caloric restriction in0.5 mmol/liter after complete starvation (P ⬍ 0.001). This was creases myocardial TG content in lean healthy men. This increase J Clin Endocrinol Metab, February 2008, 93(2):497–503 jcem.endojournals.org 501 Reingold et al. (14) documented that shortterm fasting leads to myocardial TG accumulation, although they did not document 8 effects on myocardial function. The current results, documenting dose-dependent 7 effects of caloric restriction on levels of plasma FFA, myocardial TG content, and 6 diastolic function, extend these findings and support the general concept that in5 creased myocardial TG content is associated with decreased myocardial function 4 (33). Alternatively, starvation profoundly alters endogenous metabolic regulation 3 and other, yet undefined, metabolic effects than merely increased levels of plasma FFA * 2 and myocardial TG content, which may be involved in explaining the reduction in 1 myocardial diastolic function. For example, caloric restriction might change cal0 cium homeostasis in the myocardium (34), baseline partial complete which affects myocardial diastolic function starvation starvation (35). FIG. 3. Hepatic TG content at baseline, and after partial and complete starvation. Individual Transmitral flow velocities are load dechanges in hepatic TG content upon complete starvation (n ⫽ 10). Vertical lines represent mean ⫾ SD. *, P ⬍ 0.05 vs. baseline. pendent and can be affected by changes in intravascular volume. However, estimated left ventricular filling pressures were unchanged upon progresis paralleled by decreased diastolic myocardial function. In adsive caloric restriction. Therefore, we believe that the observed dition, the results document a dose-dependent effect between the change in transmitral flow patterns results from a change in the degree of caloric restriction and the myocardial effects. These relaxation of the left ventricle. Caloric restriction enhances adobservations point to physiological variations in myocardial TG ipose tissue lipolysis, reflected in increased levels of plasma FFA, content and diastolic function. The effect of caloric restriction on due to reduced insulin levels. Similar to our results in the heart, redistribution of endogenous TG stores is tissue specific because others found corresponding results of increased TG content of we demonstrated differential effects of partial and complete starskeletal muscle after fasting (19, 25, 26). Starvation affects more vation on liver TG content. parameters of lipid metabolism because plasma FFAs stimulate Different degrees of starvation were associated with a conthe hepatic production of very low density lipoprotein (VLDL), siderable increase in plasma FFA levels, in accordance with prewhich is an important supplier for TG to the heart (36, 37). vious observations (25, 26). These increased FFA levels reflect Plasma FFA levels also increase during starvation and most likely increased lipolysis of TG content in adipose tissue. Apparently, will contribute to increased myocardial TG levels. However, the during starvation myocardial FA uptake exceeds the requirerelative contribution of albumin-bound FAs vs. FAs derived from ments of myocardial FA oxidation, resulting in increased TG VLDL-TG to myocardial TG stores during caloric restriction stores. Moreover, progressive caloric restriction has dose-depencannot be derived from the present data. dent effects on myocardial TG accumulation and myocardial We found a correlation between hepatic fat content and BMI, function. However, a causal relationship between myocardial in accordance with previous observations (2, 38). However, deTG content and myocardial function cannot be derived from the spite the increase in the flux of plasma FFA to the liver, considpresent data. ering the increased plasma FFA levels, hepatic TG content was Our data are supported by animal experiments. In those studdecreased after partial starvation but was unchanged after comies excessive exposure of the myocardium to plasma FA is acplete starvation. In line with our results, Westerbacka et al. (9) companied by increased storage of myocardial TGs, resulting in previously documented that a low fat diet in moderately obese the production of FA intermediates, and ultimately deteriorawomen decreases hepatic TG content. Because hepatic TG contions in myocardial function (8, 27, 28). Accordingly, it has been tent is tightly regulated by the balance of hepatic FA uptake, suggested that in obese subjects, subclinical diastolic dysfunction hepatic FA oxidation, and output of VLDL-TG particles, it is is due to changes in myocardial metabolism (29 –32). Kankaanpossible that this hepatic balance between FA uptake and TG pää et al. (12) reported that alterations in left ventricular function output is differentially affected by partial and complete starvain moderate obese subjects are associated with increased myotion. Nonetheless, our data indicate that progressive caloric recardial TG content, compared with lean subjects. Moreover, striction differentially affects tissue-specific stores of TG in heart Szczepaniak et al. (1) showed increased myocardial TG content and liver, and prove that myocardial TG content and myocardial in overweight and obese subjects, which was accompanied by function vary depending on nutritional conditions, at least with increased left ventricular mass. In accordance with our study, Hepatic TG (%) 9 502 Hammer et al. Myocardial TG Content and Diastolic Function J Clin Endocrinol Metab, February 2008, 93(2):497–503 TABLE 2. Effects of progressive caloric restriction on myocardial function Systolic blood pressure (mm Hg) Diastolic blood pressure (mm Hg) Heart rate (bpm) LVEF (%) E/A ratio E deceleration (ml/sec2 ⫻ 10⫺3) Baseline Partial starvation Complete starvation 120 ⫾ 10 64 ⫾ 7 62 ⫾ 13 60 ⫾ 4 2.2 ⫾ 0.4 3.4 ⫾ 0.7 118 ⫾ 9 62 ⫾ 7 59 ⫾ 10 59 ⫾ 4 2.1 ⫾ 0.4 2.9 ⫾ 0.5b 122 ⫾ 12 61 ⫾ 5 65 ⫾ 10 60 ⫾ 6 1.8 ⫾ 0.4a 2.8 ⫾ 0.9b Data are mean ⫾ SD. bpm, Beats per minute. a P ⬍ 0.01 vs. baseline. b P ⬍ 0.05 vs. baseline. respect to progressive degrees of starvation. Additional studies are required to elucidate to which extent these results can be extrapolated to clinically relevant conditions like type 2 diabetes mellitus and obesity. In conclusion, progressive caloric restriction induces a dosedependent increase in myocardial TG content and a dose-dependent decrease in diastolic function in lean healthy men. Hepatic TG content showed a differential response to progressive caloric restriction, indicating that redistribution of endogenous TG stores is tissue specific, at least in lean healthy men. Acknowledgments Address all correspondence and requests for reprints to: S. Hammer, Department of Endocrinology and Metabolism (C4-R), Leiden University Medical Center, P.O. Box 9600, 2300 RC Leiden, The Netherlands. E-mail: [email protected]. Disclosure Summary: S.H., R.W.v.d.M., H.J.L., A.d.R., J.W.A.S., and J.A.R. have nothing to declare. M.S. is employed by Philips Medical Systems. This author provided technical and intellectual input. The authors who were not employed by Philips Medical Systems had full control of the inclusion of the data and information that might have presented a conflict of interest for this author. References 1. Szczepaniak LS, Dobbins RL, Metzger GJ, Sartoni-D’Ambrosia G, Arbique D, Vongpatanasin W, Unger R, Victor RG 2003 Myocardial triglycerides and systolic function in humans: in vivo evaluation by localized proton spectroscopy and cardiac imaging. Magn Reson Med 49:417– 423 2. Ishii M, Yoshioka Y, Ishida W, Kaneko Y, Fujiwara F, Taneichi H, Miura M, Toshihiro M, Takebe N, Iwai M, Suzuki K, Satoh J 2005 Liver fat content measured by magnetic resonance spectroscopy at 3.0 tesla independently correlates with plasminogen activator inhibitor-1 and body mass index in type 2 diabetic subjects. Tohoku J Exp Med 206:23–30 3. Sinha R, Dufour S, Petersen KF, LeBon V, Enoksson S, Ma YZ, Savoye M, Rothman DL, Shulman GI, Caprio S 2002 Assessment of skeletal muscle triglyceride content by (1)H nuclear magnetic resonance spectroscopy in lean and obese adolescents: relationships to insulin sensitivity, total body fat, and central adiposity. Diabetes 51:1022–1027 4. Lee Y, Hirose H, Ohneda M, Johnson JH, McGarry JD, Unger RH 1994 -cell lipotoxicity in the pathogenesis of non-insulin-dependent diabetes mellitus of obese rats: impairment in adipocyte--cell relationships. Proc Natl Acad Sci USA 91:10878 –10882 5. Shimabukuro M, Zhou YT, Levi M, Unger RH 1998 Fatty acid-induced  cell apoptosis: a link between obesity and diabetes. Proc Natl Acad Sci USA 95: 2498 –2502 6. Shimabukuro M, Higa M, Zhou YT, Wang MY, Newgard CB, Unger RH 1998 Lipoapoptosis in -cells of obese prediabetic fa/fa rats. Role of serine palmitoyltransferase overexpression. J Biol Chem 273:32487–32490 7. Unger RH, Orci L 2001 Diseases of liporegulation: new perspective on obesity and related disorders. FASEB J 15:312–321 8. Zhou YT, Grayburn P, Karim A, Shimabukuro M, Higa M, Baetens D, Orci L, Unger RH 2000 Lipotoxic heart disease in obese rats: implications for human obesity. Proc Natl Acad Sci USA 97:1784 –1789 9. Westerbacka J, Lammi K, Hakkinen AM, Rissanen A, Salminen I, Aro A, Yki-Jarvinen H 2005 Dietary fat content modifies liver fat in overweight nondiabetic subjects. J Clin Endocrinol Metab 90:2804 –2809 10. den Hollander JA, Evanochko WT, Pohost GM 1994 Observation of cardiac lipids in humans by localized 1H magnetic resonance spectroscopic imaging. Magn Reson Med 32:175–180 11. Felblinger J, Jung B, Slotboom J, Boesch C, Kreis R 1999 Methods and reproducibility of cardiac/respiratory double-triggered (1)H-MR spectroscopy of the human heart. Magn Reson Med 42:903–910 12. Kankaanpää M, Lehto HR, Parkka JP, Komu M, Viljanen A, Ferrannini E, Knuuti J, Nuutila P, Parkkola R, Iozzo P 2006 Myocardial triglyceride content and epicardial fat mass in human obesity: relationship to left ventricular function and serum free fatty acid levels. J Clin Endocrinol Metab 91:4689 – 4695 13. van der Meer RW, Doornbos J, Kozerke S, Schar M, Bax JJ, Hammer S, Smit JW, Romijn JA, Diamant M, Rijzewijk LJ, de Roos A, Lamb HJ 2007 Metabolic imaging of myocardial triglyceride content: reproducibility of 1H MR spectroscopy with respiratory navigator gating in volunteers. Radiology 245: 251–257 14. Reingold JS, McGavock JM, Kaka S, Tillery T, Victor RG, Szczepaniak LS 2005 Determination of triglyceride in the human myocardium by magnetic resonance spectroscopy: reproducibility and sensitivity of the method. Am J Physiol Endocrinol Metab 289:E935–E939 15. van der Meer RW, Hammer S, Smit JW, Frolich M, Bax JJ, Diamant M, Rijzewijk LJ, de Roos A, Romijn JA, Lamb H 2007 Short term caloric restriction induces accumulation of myocardial triglycerides and decreases left ventricular diastolic function in healthy subjects. Diabetes 56:2849 –2853 16. ESHRE Capri Workshop Group 2006 Hormones and cardiovascular health in women. Hum Reprod Update 12:483– 497 17. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus 2003 Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 26(Suppl 1):S5–S20 18. Klein S, Sakurai Y, Romijn JA, Carroll RM 1993 Progressive alterations in lipid and glucose metabolism during short-term fasting in young adult men. Am J Physiol 265(5 Pt 1):E801–E806 19. Johnson NA, Stannard SR, Rowlands DS, Chapman PG, Thompson CH, O’Connor H, Sachinwalla T, Thompson MW 2006 Effect of short-term starvation versus high-fat diet on intramyocellular triglyceride accumulation and insulin resistance in physically fit men. Exp Physiol 91:693–703 20. Vanhamme L, van den BA, Van Huffel S 1997 Improved method for accurate and efficient quantification of MRS data with use of prior knowledge. J Magn Reson 129:35– 43 21. Pattynama PM, Lamb HJ, van der Velde EA, van der Wall EE, de Roos A 1993 Left ventricular measurements with cine and spin-echo MR imaging: a study of reproducibility with variance component analysis. Radiology 187:261–268 22. Hartiala JJ, Mostbeck GH, Foster E, Fujita N, Dulce MC, Chazouilleres AF, Higgins CB 1993 Velocity-encoded cine MRI in the evaluation of left ventricular diastolic function: measurement of mitral valve and pulmonary vein flow velocities and flow volume across the mitral valve. Am Heart J 125:1054 –1066 23. Lamb HJ, Beyerbacht HP, van der Laarse A, Stoel BC, Doornbos J, van der Wall EE, de Roos A 1999 Diastolic dysfunction in hypertensive heart disease is associated with altered myocardial metabolism. Circulation 99:2261–2267 24. Paelinck BP, de Roos A, Bax JJ, Bosmans JM, Der Geest RJ, Dhondt D, Parizel PM, Vrints CJ, Lamb HJ 2005 Feasibility of tissue magnetic resonance imag- J Clin Endocrinol Metab, February 2008, 93(2):497–503 25. 26. 27. 28. 29. 30. 31. ing: a pilot study in comparison with tissue Doppler imaging and invasive measurement. J Am Coll Cardiol 45:1109 –1116 Stannard SR, Thompson MW, Fairbairn K, Huard B, Sachinwalla T, Thompson CH 2002 Fasting for 72 h increases intramyocellular lipid content in nondiabetic, physically fit men. Am J Physiol Endocrinol Metab 283:E1185– E1191 Wietek BM, Machann J, Mader I, Thamer C, Haring HU, Claussen CD, Stumvoll M, Schick F 2004 Muscle type dependent increase in intramyocellular lipids during prolonged fasting of human subjects: a proton MRS study. Horm Metab Res 36:639 – 644 Christoffersen C, Bollano E, Lindegaard ML, Bartels ED, Goetze JP, Andersen CB, Nielsen LB 2003 Cardiac lipid accumulation associated with diastolic dysfunction in obese mice. Endocrinology 144:3483–3490 Ouwens DM, Boer C, Fodor M, de Galan P, Heine RJ, Maassen JA, Diamant M 2005 Cardiac dysfunction induced by high-fat diet is associated with altered myocardial insulin signalling in rats. Diabetologia 48:1229 –1237 Sharma S, Adrogue JV, Golfman L, Uray I, Lemm J, Youker K, Noon GP, Frazier OH, Taegtmeyer H 2004 Intramyocardial lipid accumulation in the failing human heart resembles the lipotoxic rat heart. FASEB J 18:1692–1700 de Las FL, Waggoner AD, Brown AL, Davila-Roman VG 2005 Plasma triglyceride level is an independent predictor of altered left ventricular relaxation. J Am Soc Echocardiogr 18:1285–1291 Diamant M, Lamb HJ, Groeneveld Y, Endert EL, Smit JW, Bax JJ, Romijn JA, de Roos A, Radder JK 2003 Diastolic dysfunction is associated with altered jcem.endojournals.org 32. 33. 34. 35. 36. 37. 38. 503 myocardial metabolism in asymptomatic normotensive patients with wellcontrolled type 2 diabetes mellitus. J Am Coll Cardiol 42:328 –335 Peterson LR, Herrero P, Schechtman KB, Racette SB, Waggoner AD, KisrievaWare Z, Dence C, Klein S, Marsala J, Meyer T, Gropler RJ 2004 Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation 109:2191–2196 McGavock JM, Victor RG, Unger RH, Szczepaniak LS 2006 Adiposity of the heart, revisited. Ann Intern Med 144:517–524 Han X, Cheng H, Mancuso DJ, Gross RW 2004 Caloric restriction results in phospholipid depletion, membrane remodeling, and triacylglycerol accumulation in murine myocardium. Biochemistry 43:15584 –15594 Zile MR, Brutsaert DL 2002 New concepts in diastolic dysfunction and diastolic heart failure. Part II: causal mechanisms and treatment. Circulation 105:1503–1508 Goudriaan JR, Tacken PJ, Dahlmans VE, Gijbels MJ, van Dijk KW, Havekes LM, Jong MC 2001 Protection from obesity in mice lacking the VLDL receptor. Arterioscler Thromb Vasc Biol 21:1488 –1493 Sakai J, Hoshino A, Takahashi S, Miura Y, Ishii H, Suzuki H, Kawarabayasi Y, Yamamoto T 1994 Structure, chromosome location, and expression of the human very low density lipoprotein receptor gene. J Biol Chem 269:2173–2182 Westerbacka J, Corner A, Tiikkainen M, Tamminen M, Vehkavaara S, Hakkinen AM, Fredriksson J, Yki-Jarvinen H 2004 Women and men have similar amounts of liver and intra-abdominal fat, despite more subcutaneous fat in women: implications for sex differences in markers of cardiovascular risk. Diabetologia 47:1360 –1369