* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Guideline for the Management of Infections in Eyes, Ears, Nose and
Survey
Document related concepts
Transcript
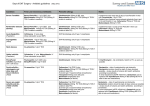
Management of Infections in Eyes, Ears, Nose and Throat in adults Full Title of Guideline: Division & Speciality: Guideline for the Management of Infections in Eyes, Ears, Nose and Throat in adults Sarah Partridge, Antimicrobial Pharmacist Mr Marshall Consultant ENT Mr John Sharp Opthalmology SpR Fiona Donald, Consultant Microbiologist Riya Savjani Senior Clinical Pharmacist: Antimicrobials (May 2017 update) Diagnostics and Clinical Support, Microbiology Scope (Target audience, state if Trust Prescribers, trained nurses and pharmacists Author (include email and role): wide): Review date (when this version goes out December 2018 of date): Explicit definition of patient group to which it applies (e.g. inclusion and Adult patients with named infections exclusion criteria, diagnosis): Changes from previous version (not Piperacillin/tazobactam removed from first line empirical treatment of malignant otitis externa due to national shortage Summary of evidence base this • Local microbiological sensitivity surveillance guideline has been created from: • Recommended best practice based on clinical experience of guideline developers • SIGN guideline (2010). Management of sore throat and indications for tonsillectomy. Available online from: http://www.sign.ac.uk (accessed 20.4.15) • Public Health England (2014) Management of infection guidance for primary care for consultation and adaption. Available online from: http://www.gov.uk (accessed 20.4.15) This guideline has been registered with the trust. However, clinical guidelines are guidelines only. The interpretation and application of clinical guidelines will remain the responsibility of the individual clinician. If in doubt contact a senior colleague or expert. Caution is advised when using guidelines after the review date or outside of the Trust. applicable if this is a new guideline, enter below if extensive): Nottingham Antimicrobial Guidelines Committee – December 2015 Page 1 of 15 Review: December 2018 GUIDELINE FOR THE MANAGEMENT OF INFECTIONS IN EYES, EARS, NOSE AND THROAT IN ADULTS Contents Page 1. Introduction 3 2. Eye Infections 3 2.1 Acute Bacterial Conjunctivitis 3 2.2 Chlamydial Conjunctivitis 4 2.3 Orbital Cellulitis 5 2.4 Herpes Zoster Ophthalmicus 5 2.5 Endophthalmitis 5 2.6 Corneal infection (keratitis) 6 6 3. Ear, Nose & Throat (ENT) Infections 3.1 Upper Respiratory Tract Infection 6 3.2 Acute Tonsillitis / Sore Throat 7 3.3 Quinsy or Peri-tonsillar Abscess 7 3.4 Acute Epiglottitis 8 3.5 Acute Otitis Media 8 3.5 Mastoiditis 9 3.7 Otitis Externa 9 3.8 Malignant / necrotising otitis externa 10 3.9 Acute Bacterial Sinusitis 11 3.10 Ludwig’s angina 11 3.11 Para-pharyngeal / Retro-pharyngeal abscess 11 3.12 Parotitis 12 Nottingham Antimicrobial Guidelines Committee – December 2015 Page 2 of 15 Review: December 2018 Guideline for the Management of Infections in Eyes, Ears, Nose and Throat 1. Introduction This guideline recommends empiric antimicrobial treatment options for adult patients with specified eye, ear, nose and throat infections. 2. Eye Infections 2.1 Acute Bacterial Conjunctivitis Common causative pathogens: Staphylococcus aureus, Haemophilus influenzae, Streptococcus pneumoniae Viral conjunctivitis may be associated with upper respiratory tract symptoms and is usually self-limiting. General approach: Infective conjunctivitis is a self-limiting illness and for most people settles without treatment. Watch and wait for 3 - 4 days. If treatment is required see below. If contact lenses are usually worn these should be removed until all symptoms and signs of infection have completely resolved and any treatment has been completed for 24 hours. The possibility of a serious corneal infection must be considered in any contact lens user with a red, painful eye (see below).Contact lens wearers and those patients who have had previous intraocular surgery e.g. glaucoma drainage, refer to opthamology/contact eye casualty. Symptomatic and empirical treatment is usually adequate. Treatment: • Chloramphenicol 0.5% eye drops 1 drop to affected eye(s) 2 hourly reducing to QDS as the infection improves. • Continue for 48 hours after resolution, usually 5 - 7 days. • If not responding to treatment, or if severe, refer to ophthalmology. 2.2 Chlamydial Conjunctivitis These should be considered in patients with risk factors for sexually transmitted diseases or in cases of chronic conjunctivitis. Investigation: Clean off any exudate and swab the conjunctiva with a chlamydia swab and a bacterial swab. Nottingham Antimicrobial Guidelines Committee – December 2015 Page 3 of 15 Review: December 2018 Treatment: 1st line: • Doxycycline PO 100mg BD for 7 days. • If patient is pregnant use Erythromycin PO 500mg QDS for 7 days. Alternative: • Azithromycin PO 1g single dose (see advice below regarding using Azithromycin in pregnancy). Where compliance with Erythromycin is likely to be a problem the patient can be offered Azithromycin PO 1g as a single dose following a discussion around the potential risks and benefits of its use with the patient. If gonococcus is suspected, seek advice on treatment from GUM and ophthalmology. Contact tracing and follow-up to be arranged through GUM when diagnosis confirmed. 2.3 Orbital Cellulitis Pre-septal cellulitis refers to infections localised to the lids. These are commonly caused by infected cysts, wounds or from sinuses. The septum provides some barrier to spread of infection into the orbit. In contrast, orbital cellulitis is infection in the orbit, often due to spread of infection from the sinuses through the thin lamina papyracea into the orbit. Symptoms of sinusitis or upper respiratory infection therefore often precede orbital cellulitis. It is a potentially sight and life-threatening infection due to spread to the cavernous sinus. Management is usually by ENT and ophthalmology. Care under a medical team may be required for patients who are unwell. Early discussion with ITU should be performed if there are signs of systemic deterioration. Diabetic or immunosuppressed patients may develop serious fungal infections, and necrotizing fasciitis should also always be considered. Common causative pathogens: Staphylococcus aureus, Streptococci (including the Streptococcus milleri group), Anaerobes, Haemophilus influenza. Investigation: • Blood cultures. • Swabs if any pus or exudate. Treatment: If intracranial extension suspected, please contact Microbiology for advice. 1st line: • Co-amoxiclav IV 1.2g TDS. • Converting to Co-amoxiclav PO 625mg TDS for a total of 10 days. Nottingham Antimicrobial Guidelines Committee – December 2015 Page 4 of 15 Review: December 2018 Mild penicillin allergy: • Cefuroxime IV 1.5g TDS plus Metronidazole IV 500mg TDS. • Converting to Cefalexin PO 500mg TDS plus Metronidazole PO 400mg TDS for a total of 10 days. Severe penicillin allergy (e.g. anaphylaxis, angioedema, urticarial rash in first 72 hours) or cephalosporin allergy: • Ciprofloxacin IV 400mg BD plus Metronidazole IV 500mg TDS plus Vancomycin IV (refer to antibiotic website for dosing, pre-dose level monitoring advice and the Vancomycin dosing calculator). • Converting to Levofloxacin PO 500mg OD plus Metronidazole PO 400mg TDS for a total of 10 days. 2.4 Herpes Zoster Ophthalmicus Potentially sight- threatening reactivation of the varicella zoster virus within the trigeminal ganglion affecting the ophthalmic division of the nerve. Ocular involvement occurs in more than fifty percent of cases with the potential for serious complications. Treatment: • Aciclovir PO 800mg 5 times a day for 7 days. • Refer patient to ophthalmology for ocular examination. 2.5 Endophthalmitis This usually presents with a history of intraocular surgery or intravitreal injection. Rapid replication of pathogens over hours, as in sepsis, causes potentially permanent loss of vision. Treatment: • Contact ophthalmology immediately. • Emergency administration of intravitreal Amikacin 0.4mg/0.1ml and intravitreal Vancomycin 1mg/0.1ml by ophthalmologist. • Vitreous tap performed at same procedure for microscopy, culture and sensitivity. • Oral antibiotics may be given according to preference of consultant ophthalmologist. Nottingham Antimicrobial Guidelines Committee – December 2015 Page 5 of 15 Review: December 2018 2.6 Corneal Infection (Keratitis) Commonly related to contact lens use, but also associated with numerous other causes. Always serious and sight threatening. Treatment: • Urgently refer cases to ophthalmology for corneal scrape for microscopy, culture and sensitivity and initiation of topical antibiotics STEROID-CONTAINING EYE DROPS SHOULD NEVER BE INITIATED UNLESS UNDER THE DIRECTION OF AN OPHTHALMOLOGIST. Ear, Nose and Throat (ENT) Infections 3.1 Upper Respiratory Tract Infection If clinical presentation suggests a viral infection, antibiotics are not indicated. Send a viral throat swab or naso-pharyngeal aspirate if influenza suspected or patient is immunocompromised (see current influenza guidelines and Microbiology A –Z guide.) 3.2 Acute Tonsillitis / Sore Throat • The majority of sore throats are viral but there is clinical overlap between viral and streptococcal infections. • The most common bacterial pathogen is Streptococcus pyogenes (Group A streptococcus). Group C and G streptococci may also be found in throat swabs but their role is less clear. • Consider Diphtheria in patients who have recent foreign travel eg to Russia, South Asia, Africa. Contact Duty Medical Microbiologist or Infectious Diseases (ID) consultant immediately if you suspect diphtheria. Antibiotics are more likely to be helpful in patients with: • a history of otitis media • general clinical condition of concern • Group A haemolytic streptococcus isolated in an inpatient • infection control reasons for example during an outbreak Using the Centor score, score 1 for each of the following. If scores more than 3 consider treatment. • Fever • Tonsillar exudate • Tender cervical lymphadenopathy • Absence of cough Investigation: Nottingham Antimicrobial Guidelines Committee – December 2015 Page 6 of 15 Review: December 2018 • Throat swab in bacterial transport medium. If treatment is required: 1st line: • • • Penicillin V PO 500mg QDS for 10 days. If unable to swallow use Benzylpenicillin IV 1.2g QDS converting to Penicillin V PO 500mg QDS. Total duration IV and PO is 10 days. If penicillin allergic: • Clarithromycin PO 500mg BD for 5 days (or IV if unable to swallow). 3.3 Quinsy or Peri-tonsillar Abscess Symptoms can include a worsening sore throat, usually on one side, pyrexia, difficulty opening the mouth, pain on or difficulty swallowing, swelling around face and neck, earache on the affected side, changes to voice or difficulty swallowing. Primarily caused by Streptococcus pyogenes. (Group A streptococcus). Investigation: Send swab or pus only if recurrent or complicated infection or the patient is immune compromised. Treatment: Appropriate surgical and airway management. 1st line: • • • Benzylpenicillin IV 1.2g QDS plus Metronidazole IV 500mg TDS. Converting to Penicillin V PO 500mg QDS and Metronidazole PO 400mg TDS Total course length (IV and PO) is 7-10 days. Mild penicillin allergy: • Cefuroxime IV 1.5g TDS and Metronidazole IV 500mg TDS. • Converting to Cefalexin PO 500mg TDS and Metronidazole PO 400mg TDS • Total course length (IV and PO) is 7-10 days. Penicillin anaphylaxis / severe allergy or allergy to cephalosporins: • Clindamycin IV 600mg QDS (until patient is able to swallow capsules). • Converting to Clindamycin PO 450mg QDS. • Total course length (IV and PO) 7-10 days. Note – if Group A streptococcus cultured then Metronidazole does not need to be continued. Nottingham Antimicrobial Guidelines Committee – December 2015 Page 7 of 15 Review: December 2018 3.4 Acute Epiglottitis Common causative pathogens Haemophilus influenzae type b, Diphtheria, Streptococcus pyogenes Respiratory obstruction due to diphtheria is rare but has a characteristic false membrane and swelling can extend from the pharynx to involve the uvula. Please contact duty Medical Microbiologist or Infectious Diseases if you suspect diphtheria. Investigations: • Take blood cultures. • Take a throat swab ONCE THE AIRWAY IS SECURE, otherwise respiratory obstruction may be precipitated. Ensure sample is labelled as being from the epiglottis. Treatment: Protect the airway. 1st line: • • Ceftriaxone IV 2g OD Note – treatment should be reviewed with culture and sensitivity results. If clinically well and able to swallow switch to: • Co-amoxiclav PO 625mg TDS • OR if penicillin allergy: Levofloxacin PO 500mg OD Total course length (PO and IV) should be 7 days. Severe penicillin allergy (e.g. anaphylaxis, angioedema, urticarial rash in first 72 hours) or cephalosporin allergy: • Vancomycin IV (refer to antibiotic website for dosing, pre-dose level monitoring advice and the Vancomycin dosing calculator) plus • Ciprofloxacin IV 400mg BD If clinically well and able to swallow switch to: • Levofloxacin PO 500mg OD Total course length (PO and IV) should be 7 days. 3.5 Acute Otitis Media Common causative pathogens Many are viral. Common bacterial causes: Streptococcus pneumoniae, Streptococcus pyogenes, Staphylococcus aureus, Haemophilus influenzae, Moraxella catarrhalis. Investigation: Nottingham Antimicrobial Guidelines Committee – December 2015 Page 8 of 15 Review: December 2018 • • Please refer patients who are not settling, who are immunocompromised or have complications to ENT for review. Bacterial swab may be useful if pus is present. Treatment (if antibiotics indicated): • Illness resolves over 4 days in 80% without antibiotics. • Antibiotics do not reduce pain in the first 24 hours, subsequent attacks or deafness. • If indicated use: Amoxicillin PO 500mg TDS for 5 days or if failure to respond to amoxicillin, Co-amoxiclav PO 625mg TDS for 5 days. Penicillin allergy: • Clarithromycin PO 500mg BD for 5 days. 3.6 Mastoiditis This is an infection of the mastoid bone and air cells, normally confirmed by CT or MRI scan. It can be a severe complication of otitis media. Rarely the infection can spread and cause meningitis or cerebral abscess. Investigation: • • • • • All patients with suspected mastoiditis should be referred to ENT for review. Discuss antibiotic treatment with microbiology. Where surgical drainage is required, pus samples should be sent for culture ideally from the post-auricular abscess or mastoid cavity. Assess for neurological signs including meningitis or altered conscious levels. Take blood cultures. 1st line: • Co-amoxiclav IV 1.2g TDS. • Converted to Co-amoxiclav PO 625mg TDS. • Prolonged antibiotic courses of 2-4 weeks may be required. Mild penicillin allergy: • Cefuroxime IV 1.5g TDS and Metronidazole IV 500mg TDS. • Converting to Cefalexin PO 500mg TDS and Metronidazole PO 400mg TDS. • Prolonged antibiotic courses of 2-4 weeks may be required. Severe penicillin allergy (e.g. anaphylaxis, angioedema, urticarial rash in first 72 hours) or cephalosporin allergy: • Ciprofloxacin IV 400mg BD plus Metronidazole IV 500mg TDS plus Vancomycin IV (refer to antibiotic website for dosing, pre-dose level monitoring advice and the Vancomycin dosing calculator). • Converting to Levofloxacin PO 500mg OD plus Metronidazole PO 400mg TDS. • Prolonged antibiotic courses of 2-4 weeks may be required. Note – treatment should be reviewed with culture and sensitivity results. Nottingham Antimicrobial Guidelines Committee – December 2015 Page 9 of 15 Review: December 2018 3.7 Otitis Externa It is important to exclude an underlying chronic otitis media. Common causative pathogens Staphylococcus aureus, Candida albicans, Pseudomonas aeruginosa, Aspergillus spp. Investigation: • In exceptional cases, swab for culture and sensitivity. Treatment: • Local aural toilet with or without topical antibiotic is the treatment of choice (for firstline options available see table 1). Table 1: First-line Topical Treatment Options for Otitis Externa Preparation Acetic Acid 2% (Earcalm Spray®) Dexamethasone with Antibacterial (Sofradex®) Hydrocortisone Acetate 1% with Gentamicin 0.3% (Gentisone® HC) Dexamethasone with Antibacterial (Otomize®) Flumetasone 0.02% with Clioquinol 1% (Locorten-Vioform®) Ciprofloxacin drops 0.3% (Ciloxin®) • • Normal Dose 1 spray at least TDS (maximum 2-3 hourly) 2-3 drops TDSQDS Recommended duration 7 days Comments Is as effective as topical antibiotics in mild otitis externa. 7 days 2-4 drops TDSQDS 7 days 1 spray TDS 7 days 2-3 drops BD 7 days 2-3 drops TDSQDS 7 days EAR drops not available, but EYE drops are acceptable to use in the ear Systemic antibiotics are only indicated when there is evidence of spreading cellulitis. Diabetic and immunocompromised patients are susceptible to malignant otitis externa, and aggressive destruction of cartilage. Refer urgently to an ENT specialist. Nottingham Antimicrobial Guidelines Committee – December 2015 Page 10 of 15 Review: December 2018 3.8 Malignant / necrotising otitis externa This requires admission, an ENT work up including imaging of the temporal bone, and prolonged IV antibiotics (usually at least 6 weeks) usually based on Microbiology advice. Treatment: • Ensure all patients are referred to ENT for review. • Send pus and deep tissue samples for culture. Initial empirical treatment 1st line: • Ceftazidime IV 2g TDS and Ciprofloxacin PO 750mg BD (Use IV route if oral route not available e.g. nil by mouth, swallowing difficulties, absorption issues). If allergic to penicillin: • Discuss with microbiology Treatment should be reviewed and discussed with microbiology. 3.9 Acute Bacterial Sinusitis Common causative pathogens Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus Diagnosis can be difficult please refer all patients to ENT for review. Many cases are viral and usually resolve within 2 – 3 weeks. Antibiotics are indicated in severe symptoms or those with symptoms for >10 days. Investigation: Nose swabs / swabs of mucous are not helpful. Endoscopy directed cultures may be helpful in complicated cases, refer to ENT. If antibiotics indicated: 1st line: • Amoxicillin PO 500mg TDS for 7 days. Penicillin allergy: • Doxycycline PO 100mg BD for 1 day, then 100mg OD for 6 days • or Clarithromycin PO 500mg BD for 7 days. 3.10 Ludwig’s angina Ludwig's Angina is a rapidly progressive cellulitis of the submandibular spaces, with potential for significant upper airway obstruction. Most reported cases follow an odontogenic infection. Common causative pathogens Usually polymicrobial involving mouth organisms such as streptococci, anaerobes, actinomyces. Investigation: • Blood cultures. • If drainage of abscess, send pus to microbiology. Nottingham Antimicrobial Guidelines Committee – December 2015 Page 11 of 15 Review: December 2018 Treatment: • Refer all patients to ENT. • Ensure safe airway management. • If abscesses are present they should be drained. • Discuss antibiotic treatment with microbiology / ENT. 3.11 Para-pharyngeal / Retro-pharyngeal abscess Parapharyngeal space infections are potentially life-threatening because of the possibility of involving the carotid sheath and its contents (e.g. common carotid artery, internal jugular vein, vagus nerve), propensity for airway impingement, and bacteraemic dissemination. Since the clinical presentation may be dominated by the symptoms and signs of the primary source of infection, the diagnosis of parapharyngeal space involvement is often delayed. Infection of the parapharyngeal space may arise from different sources throughout the neck. Dental infections are the most common underlying cause, followed by peritonsillar abscess, and rarely parotitis, otitis, or mastoiditis (Bezold's abscess). Refer urgently to specialist ENT. Common causative pathogens Usually polymicrobial involving mouth or upper respiratory tract bacteria including streptococci, anaerobes, actinomyces. Treatment (if antibiotics are indicated): • Appropriate surgical and airway management. • Discuss with Microbiology / ENT. Prolonged course of IV antibiotics may be required depending on progress. • Send PUS sample to microbiology and discuss treatment if not improving. 1st line: • Co-amoxiclav IV 1.2g TDS. • Converting to Co-amoxiclav PO 625mg TDS. Mild Penicillin allergy: • Cefuroxime IV 1.5g TDS plus Metronidazole IV 500mg TDS. • Converting to Cefalexin PO 500mg TDS plus Metronidazole PO 400mg TDS. Severe penicillin allergy (e.g. anaphylaxis, angioedema, urticarial rash in first 72 hours) or cephalosporin allergy: • Discuss with microbiology. 3.12 Parotitis Normally characterised by unilateral swelling of the parotid gland with potential abscess formation. Acute infection of the parotid gland can be caused by a variety of bacteria and viruses. Acute suppurative parotitis often occurs in the setting of debilitation, dehydration, and poor oral hygiene, particularly among elderly patients. Common causative organisms Nottingham Antimicrobial Guidelines Committee – December 2015 Page 12 of 15 Review: December 2018 Staphylococcus aureus (most common cause), Streptococcus pyogenes. Investigation: • Duct pus swab for culture if present. Blood cultures if systemically unwell. Treatment (if antibiotics are indicated): 1st line (if not at risk of MRSA – see below): • Flucloxacillin IV 2g QDS with Metronidazole IV 500 mg TDS if anaerobes suspected e.g. poor dentition. • Converting to Flucloxacillin PO 500 mg QDS +/- Metronidazole PO 400 mg TDS. • Total course length 7 – 10 days. Penicillin allergy: • Clindamycin IV 600mg QDS converting to oral 450 mg QDS when able to swallow. • Total course length 7 – 10 days. If patient known to be or previously MRSA positive, use: • Vancomycin IV (refer to antibiotic website for dosing, pre-dose level monitoring advice and the Vancomycin dosing calculator) plus Metronidazole IV 500mg TDS • For oral switch, consult with microbiology. Nottingham Antimicrobial Guidelines Committee – December 2015 Page 13 of 15 Review: December 2018 Equality Impact Assessment Report 1. Name of Policy or Service Response to external best practice policy 2. Responsible Manager Tim Hills Lead pharmacist antimicrobials and Infection control 3. Name of person Completing EIA Annette Clarkson 4. Date EIA Completed 10/12/2015 5. Description and Aims of Policy/Service Guideline for the Management of Infections in Eyes, Ears, Nose and Throat 6. Brief Summary of Research and Relevant Data There is no research or relevant data at the present time. 7. Methods and Outcome of Consultation Consultations have been carried out with the following: NUH Drugs and Therapeutics Committee NUH Antibiotic Guidelines Committee Comments from the above consultations have been received and incorporated where appropriate Nottingham Antimicrobial Guidelines Committee – December 2015 Page 14 of 15 Review: December 2018 8. 9. Results of Initial Screening or Full Equality Impact Assessment: Equality Group Assessment of Impact Age No Impact Identified Gender No Impact Identified Race No Impact Identified Sexual Orientation No Impact Identified Religion or belief No Impact Identified Disability No Impact Identified Dignity and Human Rights No Impact Identified Working Patterns No Impact Identified Social Deprivation No Impact Identified Decisions and/or Recommendations (including supporting rationale) From the information contained in the procedure, and following the initial screening, it is my decision that a full assessment is not required at the present time. 10. Equality Action Plan (if required) N/A 11. Monitoring and Review Arrangements Review: December 2018 Nottingham Antimicrobial Guidelines Committee – December 2015 Page 15 of 15 Review: December 2018