* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 89. When other options have failed... There is a therapy that can H
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
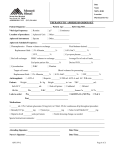
0911.LDL.Patient.ReleaseLR 12/1/04 3:44 AM Page 1 When other options have failed... There is a therapy that can HELP A Patient Guide to LDL Apheresis Therapy The HELP System (Heparin-induced Extracorporeal Lipoprotein Precipitation) 0911.LDL.Patient.ReleaseLR 12/1/04 3:44 AM Page 2 By now you’ve heard that high LDL-cholesterol – the “bad” cholesterol – is a serious threat to your health and longevity. Time Contents Lowering Blood Cholesterol: Some People Need Extra Help High LDL-Cholesterol: The Enemy Within What is LDL Apheresis – and How Does It Work? What Results Can I Expect From LDL Apheresis? How Safe is LDL Apheresis? Do I Qualify for LDL Apheresis Therapy? How Do I Get Started? The information in this guide is provided for general educational purposes only. You should confer with your physician about your particular medical condition, and to get his or her recommendation of the best treatment options for you. LDL apheresis therapy with the HELP System must be prescribed by a physician and supervised by a physician trained in its use. 2 4 6 9 10 11 12 You’ve faithfully eaten the right foods and taken the cholesterol-lowering medications your doctor prescribed. Yet your LDL-cholesterol (“LDL-C”) level is still much too high. doctors describe as “maximum tolerated drug and dietary therapy.” Without effective treatment, progressive damage to arteries can lead, by middle age or earlier, to severe angina, heart attack and strokes. You’re not alone. You are among the one in every 500 people with an inherited disorder in cholesterol metabolism called familial h y p e r c h o l e s t e r o l e m i a, or “FH.” To reduce your LDL-C to a safer range – and keep it down – your physician has recommended LDL apheresis therapy – a highly effective treatment that directly removes harmful amounts of “bad” LDL-C from your blood. For some people with FH, the LDL-C level remains stubbornly high, despite trying what 1 0911.LDL.Patient.ReleaseLR 12/1/04 3:44 AM Page 4 Lowering Blood Cholesterol: Some People Need Extra Help. You can consider yourself fortunate for two reasons. First, you are fully aware of your diagnosis and the health threat posed by your high LDL-C level. Many others remain undiagnosed, or don’t understand the damage their very high cholesterol is doing — day in and day out. to reduce their LDL-cholesterol levels, and thus reduce their risk of heart attack, stroke and premature death. This guide explains some of the health risks of high blood LDL-cholesterol, and how regular LDL apheresis treatments with the HELP System reduce and maintain a lower LDL-cholesterol level. Second — if you qualify — you have access toa proven LDL apheresis technology called the HELP System. This procedure has been used in Europe since 1986, and was approved by the FDA for patient use in the U.S. in 1997. More than 200,000 HELP treatments have enabled people with treatment-resistant FH Most importantly, this guide and consultation with your physician will help you determine if you’re a good candidate for LDL apheresis therapy. 2 HELP THERAPY ALLOWS YOU TO KEEP PURSUING YOUR GOALS 3 0911.LDL.Patient.ReleaseLR 12/1/04 3:44 AM Page 6 High LDL-Cholesterol: The Enemy Within Your heart quietly and efficiently pumps blood to every organ and cell in your body, including the hard-working muscle of the heart itself. That life-giving blood courses through a network of flexible, smooth-walled arteries and veins to deliver oxygen and nutrients to your brain, heart and other vital organs, as well as to your muscles and skin. white blood cells migrate through that cell layer and take up oxidized LDL particles, in a failing effort to repair the damage. The result is deposition of a fatty streak in the arterial wall. When the LDL level remains too high, this disease process progresses to produce a hard fibrous plaque. Over a period of years, painful angina can develop, as the coronary arteries narrow and less and less blood reaches the heart muscle. But these thick arterial plaques also set up the conditions for sudden, life-threatening thrombosis (blood clotting). When a fibrous plaque becomes unstable and breaks or tears, a thrombus may almost instantly form on the surface of the plaque, and block the artery. But when the LDL level in the blood is much higher than the optimal, healthy range, a disease process called atherosclerosis (athero = fatty and sclerosis = scarring or hardening) progressively damages the major arteries. Progression of atherosclerosis When a sudden thrombosis occurs in a coronary artery supplying blood, it can cause a myocardial i n f a r c t i o n, or heart attack. A similar event in the arteries supplying the brain causes a stroke. LDL (low-density lipoprotein) is a normal carrier of cholesterol. But when the blood LDL-C concentration is too high, more of it is oxidized. Some of that oxidized LDL-C appears to enter and injure the thin, single layer of cells that lines the inner walls of the arteries. Apparently, In 1992, a landmark study reported on the relationship between blood cholesterol levels and survival of over 360,000 American men for 12 years,1 and found that the rate of death from coronary heart disease climbed proportionally as the measured LDL-C level increased. 4 100 90 80 70 60 50 40 30 20 10w 0 80 w w w w w w w w w The newest National Cholesterol Educational Program (NCEP) guidelines define an LDL level of less than 100 milligrams per deciliter of blood as “optimal,” while 130 to 159 milligrams is “borderline high,” and 160 to 189 milligrams is “high.” 5 w w NCEP Classification of LDL-Cholesterol Levels Optimal 120 160 200 240 280 LDL-Cholesterol (mg/dL) Death rate from coronary heart disease in relating to LDL-C over a 12-year period (in 361,662 U.S. men) <100 Near Optimal 100-129 Borderline High 130-159 High 160-189 Very High >190 For patients with established heart disease, the NCEP guidelines now recommend lowering LDL-cholesterol to less than 100 mg/dL. On a “time-averaged” basis, that low level is probably not realistic for you even with LDL apheresis, but the more you can reduce your LDL-cholesterol level, the more you reduce your risk of heart attack and premature death. Several other studies have confirmed that, for a rise of each 20 milligrams per deciliter(mg/dL) in the total cholesterol level, one’s risk of death increases by more than 20%.2,3 In 1996, another major clinical study proved that long-term treatment to reduce LDL-cholesterol – in this case using an LDL-lowering drug – saves lives.4 5 0911.LDL.Patient.ReleaseLR 12/1/04 3:44 AM Page 8 What is LDL Apheresis — and How Does it Work? Blood withdrawn from the patient is continuously separated into plasma and cellular components by passage through a capillary plasma filter. Cellular components are returned directly to the patient. You are already taking one or more medications which work in different ways to reduce your LDL-C level. If you are a qualified candidate for LDL apheresis, you will continue on your drug and dietary regimen. Third Phase: The “cleaned” plasma then passes through other filters to remove excess heparin and fluids, and finally is returned (along with your blood cells) to your circulation through a vein in the other arm. LDL apheresis works differently than drug therapy, by physically removing the LDL-C from your blood. LDL apheresis involves three phases. B U F F E R / H E PA R I N 2 1 First Phase: A small portion of whole blood is drawn, usually from an arm vein, and passed through tubing into the HELP System device. Oxygen-carrying red cells and other blood cells are separated from the liquid plasma component of your blood. You leave your appointment with nearly all of the blood you came in with – minus about 60% of the harmful LDL- cholesterol that had accumulated in your circulation. Most people can be treated every two weeks, but people with very high LDL-C levels, including those with a rare “homozygous” form of FH, often require weekly treatments. Second Phase: A solution containing heparin is added to the plasma. The heparin adheres to many LDL-cholesterol molecules, causing them to “precipitate” as a sticky yellow material. A container containing small-pored filters captures that yellowish mass of excess LDL-C, which is later discarded. Your “cleaned” plasma passes through this filter. 3 P R E C I P I TAT E F I LT E R 1 Physiologic pH of LDL- and heparin-free plasma is corrected with bicarbonate dialysis, followed by ultrafiltration to correct volume. 5 THE PROCESS Basic HELP treatment process to physically remove LDL-C Your LDL apheresis staff will give you specific instructions, including a reminder to eat and drink well before each appointment. They will also make every effort to assure that your appointments are as comfortable and pleasant as possible. 6 When pH is adjusted to 5.12, lipoprotein complexes form a precipitate. PLASMA CAPILLARY PLASMA FILT E R U LT R A - F I LT E R This process is repeated a number of times during your treatment session, which usually takes one to two hours. A mixture of sodium acetate buffer (pH 4.85) and heparin (100 IU/ml) are added to the plasma in equivalent parts by volume. 7 H E PARIN ADSORBER 4 The precipitated lipoprotein complexes are captured in the precipitate filter, which is later discarded. Residual heparin is removed from the LDL-free plasma by a heparin adsorber. 0911.LDL.Patient.ReleaseLR 12/1/04 3:44 AM Page 10 What Results Can I Expect From LDL Apheresis? When you leave your treatment session, your LDL-C level will be reduced by roughly 60%, down to about 40% of the pre-treatment level. But because this blood-cleaning treatment doesn’t change the underlying metabolic problem, your LDL-C level will immediately begin to increase, or rebound. Again, reduction of this “bad cholesterol” has been shown in many clinical studies to reduce the risk of coronary heart disease and premature death. HELP therapy also reduces blood fibrinogen (a clotting protein) and triglycerides. The level of HDLcholesterol usually dips by 10-15%, but generally recovers within two days to pretreatment levels.6 Without regular LDL apheresis treatments, your LDL-C concentration will rise to close to its pretreatment level within less than two weeks. Thus, frequent, regularly scheduled treatments are required to keep your average LDL level in a lower, healthier range. Pre-treatment Post-treatment LDL-C -60 to 64%* Triglycerides H E LP therapy immediately reduces LDL-C levels and maintains a lower level over time. Fibrinogen -36 to 47%* -58 to 65%* *Extent of reduction varies by individual In a German study evaluating the HELP System in 39 patients with existing coronary heart disease, the share of patients who were free of angina increased from 18% prior to HELP therapy, to 38% over just two years of regular treatment.7 HELP THERAPY ALLOWS YOU TO KEEP DOING THE THINGS YOU LOVE. A number of other studies have also shown that LDL-lowering therapies may slow, halt and even reverse the progression of atherosclerotic plaques in the coronary arteries. Time As you can see, regular, ongoing LDL apheresis therapy will effectively reduce your average LDL-cholesterol level. 8 9 0911.LDL.Patient.ReleaseLR 12/1/04 3:44 AM Page 12 Do I Qualify for Apheresis Therapy? How Safe is LDL Apheresis? Over more than 20 years of use, LDL apheresis has proven itself to be a very safe method for treating excessive LDL-cholesterol levels. Other minor adverse events which occurred in at least 0.1% of procedures (1 in every 1,000) include: To date, there have been no reported patient deaths attributable to HELP LDL apheresis therapy. A German study of 51 patients who received 4,330 HELP treatments over a two-year period documented no serious adverse events.7 Adverse Event Number (%) Nevertheless, like any drug or medical intervention, adverse reactions or events do infrequently occur. Chills/Shivering 9 (0.3%) Fatigue 8 (0.3%) In most instances, these adverse reactions are easily managed, and don’t require discontinuation of the treatment. Prolonged PTT or ACT 7 (0.2%) Nausea/Vomiting 7 (0.2%) Chest Heavy/Pain 4 (0.1%) Adverse reactions associated with HELP therapy are those typically expected with any procedure involving circulation of blood outside the body. In the U.S. HELP trial involving more than 2,800 treatments, hypotension (low blood pressure) was the most common adverse reaction. This minor temporary reaction can usually be managed by giving the patient intravenous fluids, and the treatment completed. Dizziness/Syncope 4 (0.1%) Headache 4 (0.1%) Elevated Temperature 3 (0.1%) Others (single events) 14 (0.5%) Total = 2,826 treatments 10 At this point, your doctor has tried prescribing different combinations of lipid-lowering medications and you’ve adhered to a prescribed diet. But despite this, your LDL-C level is still much too high. • Heterozygous FH patients whose LDL-C level exceeds 300 mg/dL Your physician has recommended LDL apheresis therapy to help you manage your LDL-C level. But unfortunately not every patient with high LDL-cholesterol is a good candidate for this lifelong treatment. LDL apheresis is an ongoing therapy that requires commitment on your part for the long haul. Successful candidates are people who fully understand the importance of lowering their LDL-C levels, and commit to making their apheresis visit part of their routine. • Heterozygous FH patients whose LDL-C exceeds 500 mg/dL H E LP LDL apheresis therapy is indicated when at least six months of maximum tolerated drug and dietary therapy fails to achieve lowering of the LDL-C level below certain thresholds. The three subgroups include: Your doctor will be happy to answer any questions you have, and may also ask you a number of questions to make sure you are a motivated candidate, willing to commit to long-term LDL apheresis therapy. • Heterozygous FH patients whose LDL-C level exceeds 200 mg/dL and have angina, or a history of coronary heart disease (CHD)* 11 0911.LDL.Patient.ReleaseLR 12/1/04 3:44 AM Page 14 How do I Get Started? You and your doctor need to obtain some specific information to make sure that LDL apheresis is appropriate, practical and affordable for you. Venous Access. Before you can begin LDL apheresis therapy, your physician will examine your arm veins. For some people whose veins are “fragile” from years of cardiovascular disease, alternatives to simple arm vein access may be appropriate. “Baseline” Blood Test. Your doctor will order blood tests to establish your current “baseline” LDL-C level. This “lipid panel” of tests also includes total cholesterol, HDL-cholesterol, and triglycerides. Insurance Verification. As this is an FDA-approved therapy, most insurance policies cover LDL apheresis. Insurers will ask your doctor to provide specific information about your treatment history and laboratory results before they can authorize payment. You and your physician will review your blood test results together, to determine whether you’re an appropriate candidate for LDL apheresis therapy. Finally, you’re ready to start on your new path to a healthier future. REFERENCES Neaton JD, Wentworth D. Arch Int Med 1992; 152:56-64. 2 Verschuren WMM, Jacobs DR et al. JAMA 1995; 274(2):131-6. 3 Anderson KM, Castelli WP and Levy D. JAMA 1987; 257(16):2176-80. 4 Cholesterol and Recurrent Events (CARE) Trial Investigators. N Engl J Med 1996; 335:1001-1009. 5 Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001; 285(19);2486-2509. 6 Lane DM, Alaupovic P, Knight-Gibson C et al. Am J Cardiol 1995; 75:1124-29. 7 S c h u ff - Werner P, Gohlke H, Bartmann U et al. Eur J Clin Investig 1994; 24:724-32. 1 12 0911.LDL.Patient.ReleaseLR 12/1/04 3:44 AM Page 16 B. Braun Medical Inc. Rx only HELP is a trademark of B.Braun Medical Inc. Copyright 2004 B.Braun Medical Inc. HELP.002L 10/04 824 Twelfth Avenue Bethlehem, PA 18018 1-800-848-2066 email: [email protected] www.bbraunusa.com