* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download (HbA) and sickle hemoglobin
Survey
Document related concepts
Transcript
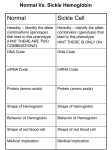
BIL 256 Cell and Molecular Biology Lab Spring, 2007 Sickle Cell Anemia Background Information Red blood cells, or erythrocytes, carry the protein hemoglobin in the circulation. This protein serves to transport oxygen from the lungs to the tissue. Hemoglobin is a globular protein made up of 4 subunits. Each subunit contains a polypeptide chain attached to an iron-containing component called heme. Each heme group contains one iron atom and each iron atom can bind one O2 molecule. The polypeptide chains of hemoglobin are referred to as the globin portion of the molecule. Normal adult hemoglobin (hemoglobin A) has four sub-units made up of two alpha (α) and two beta (β) polypeptide chains. Each α-chain contains 141 amino acid residues and each β-chain contains 146 amino acid residues. Fetal hemoglobin (hemoglobin F) is found in the blood of the human fetus. Hemoglobin F is similar to hemoglobin A except that γ-chains replace the β-chains. Although adult hemoglobin normally replaces fetal hemoglobin shortly after birth, fetal hemoglobin fails to disappear in certain individuals and persists throughout life. Many changes in the structure of hemoglobin have arisen by mutations in the human population. About one person in 100 contains a mutant hemoglobin gene and these individuals have an abnormal hemoglobin molecule in their blood. The mutations often involve substitution of one amino acid for another and usually they are harmless. However, in a few cases, mutations in hemoglobin can cause serious diseases. One of the most common and serious abnormal hemoglobins is hemoglobin S, which is present in individuals suffering from sickle cell anemia. In hemoglobin S, a single glutamic acid residue on the β-chains is replaced by valine. This single change in the primary sequence causes a marked change in the net charge and conformation of the protein. When hemoglobin S is deoxygenated, it crystallizes in the red blood cells and this leads to a distortion of the red cells into a sickle shape. These abnormal cells are then destroyed rapidly in the body which leads to a reduced number of erythrocytes; hence the term, sickle cell anemia. Sickle cell disease is inherited as an autosomal recessive gene. When the gene for hemoglobin S is inherited from only one parent the individual is heterozygous for the condition and has sickle cell trait. Although these individuals rarely have severe anemia, half of their circulating hemoglobin is hemoglobin S and half is normal hemoglobin A. When the gene for hemoglobin S is inherited from both parents, the individual is homozygous. In this case, all of the hemoglobin is hemoglobin S and the individual suffers from severe anemia. The gene for hemoglobin S is thought to have originated in the population in Eastern Africa. Hemoglobin S has an important benefit in the African population because it confers resistance to one form of malaria. In some parts of Africa, 40% of the population has the sickle cell trait. The incidence of sickle cell trait in the American Black population is about 10%, and about 1-2% of this population has sickle cell anemia. Abnormal hemoglobins are often detected in the clinical lab by electrophoresis. Hemoglobin molecules at pH 9.2 move toward the anode in an electrophoretic system at a speed proportional to the strength of their charge. The isoelectric point of normal hemoglobin A is 6.9 but the isoelectric point of certain hemoglobin variants differ depending on the hemoglobin type. As discussed above, valine residues replace the glutamic acid residues in the β-chains of hemoglobin S. Thus, hemoglobin S hemoglobin has two fewer negative charges per hemoglobin molecule than hemoglobin A and its isoelectric point and electrophoretic properties are correspondingly affected. Hemoglobin variants including sickle cell, sickle trait, persistence of fetal hemoglobin in the adult and many others can be detected by electrophoresis. The Figure shown below illustrates the electrophoretic separation of the normal hemoglobin variants. Objectives: In this experiment you will examine the electrophoretic behavior of hemoglobin from a normal person and from a person with sickle cell trait. In addition, an optional part of this experiment is for the student to examine his or her own hemoglobin. Procedure I. Preparation of the Hemoglobin Sample 1. Disinfect your finger with 70% alcohol, allow it to dry and puncture it with a sterile finger lancet. 2. Allow 1 drop of blood to fall into a microcentrifuge tube. 3. Add 10 drops of the erythrocyte lysis buffer and mix the contents of the tube thoroughly. The erythrocyte lysis buffer contains the detergent Nonidet P40 which serves to lyse (break open) the erythrocytes which in turn liberate their hemoglobin. Although the final solution contains plasma proteins as well as hemoglobin, the latter is a major component of the mixture and can readily be detected after electrophoresis. II. Electrophoresis 1. Prepare 1.2% agarose gels and load 15 μl of the following hemoglobin solution into the sample wells. Sample* Sample Well # Protein Normal Hemoglobin 1,5 HbAA Sickle Trait Hemoglobin 2,6 HbAS Sickle Hemoglobin 3,7 HbSS Student Hemoglobin 4,8 If student hemoglobin samples are not available, electrophorese standard normal and sickle trait hemoglobin on lanes 4 and 8. 2. Electrophorese until the bromophenol blue in the samples has migrated to within 0.25 cm of the positive electrode end of the gel. 3. Since hemoglobin has its own inherent color, it can sometimes be visualized on the gels without staining. Inspect the gels carefully to see if you can identify the hemoglobin bands. 4. Stain and destain the gels and record your results noting the migration of hemoglobin A, hemoglobin S and the student hemoglobin.