* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Male Infertility Explained - Queensland Fertility Group
Prenatal testing wikipedia , lookup
Embryo transfer wikipedia , lookup
Designer baby wikipedia , lookup
Egg donation wikipedia , lookup
Female infertility wikipedia , lookup
Donor Sibling Registry wikipedia , lookup
In vitro fertilisation wikipedia , lookup
Infertility wikipedia , lookup
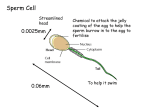
Male Infertility Explained Queensland Fertility Group’s guide to Andrology Public Information 1800 111 483 www.qfg.com.au Many couples are surprised to learn that approximately 50% of fertility issues are male-related. The male plays an equally important role in assisted conception, and a comprehensive fertility investigation will examine causative factors in both partners. Fortunately, the most common causes of male infertility are readily diagnosed and can be treated or overcome to help a couple conceive successfully. The information in this booklet outlines the fertility investigations and treatments available for males at Queensland Fertility Group. The Male Reproductive System Females are born with a limited number of eggs; however, sexuallymature males produce new sperm every day of their lives. Sperm take 72 days to be produced and a further 12 days to travel through the epididymis in preparation for ejaculation. Satisfactory sperm production requires four key components: • • • • normalhormonalstimulationfromthepituitarygland normalspermproductioninthetubulesofthetestes anunobstructedspermpathway effectivenaturalspermdelivery. Vas Deferens Penis Testicles Known Causes of Male Infertility Lifestyle • • • • • • • • • Age Smoking Recreationaldrugs Steroidabuse Weight Occupation Exposuretotoxins Radiationdamage Exposuretoexcessiveheat Sperm Problems • Productionofviablesperm –ChromosomeandDNAabnormalities – Undescended testes – Infections – Twisted testes – Varicocele – Illnesses and medications – Chemotherapy • Transportofthesperm – Obstructions –Absenceofvasdeferens – Problems relating to the prostate – Infections – Nerve damage due to surgery –Recreationaldrugsandsteroidhormones Sperm Antibodies • Injuryordamagetothebloodspermbarrier • Oftenfoundinpatientswhohavehad vasectomy reversals Erectile and Ejaculation Difficulties • • • • Spinalcordinjuries Retrogradeejaculation Prematureejaculation Somemedications Hormonal Problems • Pituitarytumours • Defectsatbirth • Steriodhormoneuse How do we test a male’s fertility? Following a consultation with your Queensland Fertility Group specialist,ourteamofdedicatedAndrologyscientistscanperforma number of tests in order to determine your ability to produce viable sperm. These tests include the following options: Semen Analysis Asemenanalysisisthefirst,andoftentheonlytest,requiredto diagnose whether or not a male is experiencing fertility problems. ThisinvolvesanAndrologistexaminingasemensampleundera microscope and searching for abnormalities. TheAndrologistwillcheckthesampleforthreekeyspermtraits: Sperm Count Low Sperm Count (Oligospermia) – Males with low sperm counts may be contributing to a couple’s infertility. Sperm Motility PoorSpermMotility(Asthenospermia)–Thespermdonot swim in a good forward-progressive manner and therefore lack the ability to make their way to the egg and then fertilise it. Sperm Morphology Poor Sperm Morphology (Teratospermia) – Most of the sperm in the semen sample are abnormally-shaped, which can result in their inability to penetrate and to fertilise an egg. You will be required to provide a semen sample for this test (refer to semen collection instructions). Sperm Antibody Test Althoughrelativelyuncommonasacauseofinfertility,thepresence ofspermantibodieshasbeenlinkedtomalefertilityissues.An estimated one in 16 males produce antibodies to their own sperm, and while they are most commonly found in males who have had vasectomy reversals or who have suffered injury or infection of the epididymis, in some cases there is no explanation for their presence. Spermcoatedwithantibodieshavedifficultypenetratingcervical mucusandeggs.YourspecialistmayorderaSpermAntibodyTest to be performed in conjunction with your semen analysis. Sperm Chromatin Structure Assay The genetic material contained in the head of the sperm is known as Chromatin.ASpermChromatinStructureAssay(SCSA)determinesthe percentageofsperminyoursemensamplecontainingdamagedDNA. AhighlevelofdamagedDNAcansignificantlyaffectacouple’sability to conceive, and can also result in early pregnancy loss. Andrologyscientistsexaminethousandsofspermwithinashorttimeperiod usingamachineknownasafluorescence-activatedcellsorter(FACS). Sperm Chromosome Studies Atthetimeoffertilisation,theheadofthespermshouldcontain23 chromosomes, which join with the 23 chromosomes contained in the egg.Anabnormalnumberofchromosomes(knownasaneuploidy)in the sperm reduces a couple’s chances of natural conception. ASpermChromosomeTestisusuallyonlyperformedwhenthereare indications that the sperm chromosome complement may be an issue. QueenslandFertilityGroup’sAndrologistsexaminethefivechromosomes commonly linked to various foetal abnormalities in order to determine the level of aneuploidy in a male’s ejaculate. The contents of the sperm head are stained using fluorescent probes, and the chromosomes are counted.Ahighlevelofaneuploidymayaffectthesperm’sabilityto fertilise an egg and to produce a chromosomally-normal embryo. Y Chromosome Abnormalities Men with very low sperm counts, or no sperm at all in their semen, may have small parts of their Y chromosome missing (deletions). Queensland Fertility Group’s Molecular Genetics laboratory has the capacity to detect thesedeletionswithabloodtestknownastheDAZDeletionTest. Therearetwobenefitsarisingfromperformingthistest.Inthecaseof there being no sperm in the semen (azospermia), the test can predict thelikelihoodofstillbeingabletofindsmallnumbersofspermin thetestes.Thesecouldbesurgicallyextracted(TESA)andusedin IVFandICSItofertiliseeggs.KnowledgeofDAZdeletionsalsoallows consideration of the likelihood of passing this genetic abnormality on to any sons arising from treatment of the infertility. How do we treat male infertility? Whiletherearenotmanytreatmentsinexistencethatwillimprovethe quality of the sperm themselves, there are a number of options available to help couples maximise the sperm’s ability to fertilise the egg. In the past, many couples have had to resort to donated sperm; however, today we can literally produce a pregnancy from a single sperm. Reversible Conditions There may be medical or environmental causes for damaged sperm DNA.Additionally,recentillnesses,recentdrugtreatments,regularheavy alcohol consumption, steroid hormone use, obesity, frequent hot baths or saunas and failure to follow correct specimen collection instructions can result in poor semen analysis results. You should tell your Queensland Fertility Group specialist if any of these factors are involved. Drug Treatment There are not many simple drug treatments that will increase sperm numbers or make the sperm swim or look better. Some males, however, produce low sperm numbers due to low reproductive hormone (gonadotrophin) levels. Gonadotrophin treatment can help these males to produce more sperm in each ejaculate. Intrauterine Insemination with Partner Semen (AI) This relatively simple procedure involving washing and concentrating the male partner’s sperm and inseminating them directly into the female uterusassistsspermthatexhibitonlyminimalabnormalitiestofindand tofertilisethefemaleegg.Aswecannevertotallyexcludetheabilityof sperm (regardless of their quality) to produce a pregnancy, this procedure isoftenthefirsttreatmentrecommendedwheremaleinfertilityisinvolved. In Vitro Fertilisation and Embryo Transfer (IVF-ET) Incasesofsubstandardspermquality,IVFcansignificantlyimprovea couple’s chances of conception. The strongest-swimming sperm are selected from the semen sample, and then placed with the eggs in a culture dish. IVF produces fertilisation in about 90% of male infertility cases, with the remaining 10% yielding no fertilisation. In addition to being performed as a treatment for male infertility, IVF provides a good diagnostictestofthesperm’sabilitytofertiliseeggs.Acrosstheboard, approximately 70% of eggs fertilise using IVF. Assisted Fertilisation by Microinjection (ICSI) The intra-cytoplasmic sperm injection (ICSI) of eggs has revolutionised the treatment of males with severe sperm abnormalities. In the past, the use of donor sperm or adoption were the only viable options for couples facing these circumstances; however, we can now inject a single sperm into each egg and achieve high fertilisation rates. The sperm injection isperformedasanadditionalpartoftheIVFprocedure.Aslongasthe sperm are alive, any motility or morphological abnormalities should not affect the procedure. Wheretherearenospermintheejaculate,spermsurgicallyretrieved fromtheepididymis(micro-epididymalspermaspirationorMESA)or thetestesthemselves(testicularspermaspirationorTESA)arequite usable in this procedure. Combined with frequent ejaculation protocol, ICSI is often the best treatmentforhighlevelsofdamagedspermDNA. Donor Insemination For many couples confronted with severe male infertility, the complexity or cost of the treatments listed above becomes prohibitive. In such cases, the couple may accept the simpler treatment option of the female being inseminated with donated semen. Semen donors are screened for prescribed genetic and infectious diseases. Acceptingdonorsemencanbeadifficultdecisionandcouplesare required to consult one of our specially-trained psychologists to discuss all aspects – both present and future – of this treatment before proceeding. Preimplantation Genetic Diagnosis (PGD) Sometimes there is a genetic basis for the male’s infertility. If there is a known or raised risk of a genetic disorder, or in cases of recurrent miscarriage, PGD can detect chromosome abnormalities and single gene disorders at the embryostage.PGDidentifiesembryosthatare free of suspected chromosomal abnormalities or genetically-linked diseases so that they may be transferred to the uterus to achieve a normal pregnancy. What will the male need to do? In order for Queensland Fertility Group to examine a male’s sperm, he mustfirstprovideasemensample.Masturbationisthemostobvious and the easiest method of sample collection; however, a number of specialist methods exist to extract sperm where necessary. Sperm Collection Methods Ejaculate The most common way to collect a semen sample is by masturbation (usually in the privacy of your own home) after two to three days of abstinence. It is very important for the whole of the ejaculate to be collected andexamined,asthesperm-richpartoftheejaculateisthefirstpart. This semen sample will need to be delivered to the Queensland Fertility Group Laboratory within one to two hours of its collection. The Laboratory will provide you with more detailed instructions on specimen collection so that maximum information can be derived from the tests. Other The condition where a male’s ejaculated semen does not contain any sperm is known as azoospermia. One of two approaches can be taken to attempt to retrieve sperm in this situation: TESA Surgical extraction of sperm from the testes, usually under general anaesthetic. MESA Surgical extraction of sperm from the epididymis under general anaesthetic. CAIRNS Queensland Fertility Group’s Network of Care 1800 111 483 www.qfg.com.au TOWNSVILLE MACKAY BRISBANE IPSWICH TOOWOOMBA GOLD COAST Brisbane Auchenflower (Wesley Hospital), Capalaba, City, Everton Park, South Bank, Spring Hill, Springfield Lakes Ipswich T [07] 4638 5243 T 1800 111 483 Mackay T [07] 4965 6500 Cairns T [07] 4041 2400 Toowoomba T [07] 4638 5243 Gold Coast T [07] 5564 8455 Townsville T [07] 4772 8900 QFG-COMM-PI-005 29-06-2013 For more information on clinic and specialist locations or Queensland Fertility Group’s regular public information events visit www.qfg.com.au