* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
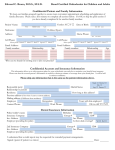
Download Cast-Analysis.09.Apr.2013
Survey
Document related concepts
Special needs dentistry wikipedia , lookup
Dentistry throughout the world wikipedia , lookup
Dental hygienist wikipedia , lookup
Focal infection theory wikipedia , lookup
Remineralisation of teeth wikipedia , lookup
Periodontal disease wikipedia , lookup
Crown (dentistry) wikipedia , lookup
Forensic dentistry wikipedia , lookup
Dental degree wikipedia , lookup
Impacted wisdom teeth wikipedia , lookup
Tooth whitening wikipedia , lookup
Dental avulsion wikipedia , lookup
Transcript
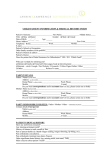
CAST ANALYSIS Experience has confirmed that describing a malocclusion in terms of the five major characteristics provides an economical and efficient way to detect all important points, without overlooking important aspects. There are five steps in cast ananlysis and each step is supplemented by revieving other diagnostic records ( orthopantomographs, lateral cephalometric radiographs, photographs ) Step 1 is to analyze the alignment and symmetry of the teeth in the dental arches. This is done by examining the dental casts, looking down on the occlusal surfaces of the teeth, casts not in occlusion. - alignment ( interproximal and contact relationship ): among the possibilities are ideal, crowded, spaced and mutilated - to ascertain which teeth are present or absent, it is obviously important to count them. In deciduous and mixed dentition we have to take orthopantomograph to ascertain whether all permanent teeth are present. The congenital absence of a tooth cannot be established accurately unless one knows the dental age of the individual and the approximate timing of the onset of calcification of the crowns under normal circumstances. For example, if a mandibular second premolar does not appear to be forming on the panoramic radiograph of a 6-year-old child, the tooth may be congenitally absent if the dental age of this child is 6 or 7 years. However, if the child´s dental age is approximately 4, it may be that the developing bud of the premolar has not yet begun to calcify - irregularities of individual teeth have to be described - it is important also to evaluate the symmetry of each dental arch, looking at both arch form and the position of the teeth within the arch. We have to evaluate the symmetry of corresponding teeth in A-P plane. If one tooth is placed more mesially than its corresponding tooth, it is wrong position due to mesial drift of the tooth. We also evaluate the symmetry of the corresponding teeth in transversal plane by comparing their distances from midline. During the clinical examination we should note the midline of the dentition in relation to the midline of the face. The skeletal midline is indicated by midpalatal raphe on the maxillary cast. If there are discrepancies, the true midline should be indicated on the lower cast. It is important to differentiate intra-arch midline shifts caused by displaced incisors from serious symmetry problem. Often simply correcting the alignment will correct the midline. This is less likely to be true if a skeletal deviation, as revealed by facial midlines that do not coincide, is noted or if there is an asymmetry in the buccal segments. Step 2 is to review the findings from the clinical examination of the face and confirm these from the casts and photographs. Of particular interest is the protrusion or retrusion of the incisors. We measure the overjet and compare it with ideal. This step should be supplemented by analysis of the photographs ( soft tissue profil ). Step 3 is to place the dental casts in occlusion and note the buccolingual relationship of the posterior teeth and the lateral ( transverse ) relationship of the jaws. A judgment is also made to determine whether a transverse problem - typically, posterior crossbite - is basically dentoalveolar, skeletal, or a combinationof the two. A continuous range of problems exist: those that are entirely skeletal to those that are entirely dental, with components of both in most instances. Because skeletal width dimensions can be seen on the dental casts, a PA cefalometric radiograph is not necessary unless skeletal asymmetry is suspected; however, if a PA ceph is available, it also is evaluated at this stage. If a bilateral palatal crossbite is entirely due to constriction of the maxilla, it is labeled as a skeletal problem. The palatal vault is narrow and high, the inclination of the long axises of posterior teeth are normal or may be slightly inclined buccaly. A similar crossbite caused by constriction of the maxillary dental arch alone, with normal width of the base of the palatal vault, would be dentoalveolar in nature. The long axises of posterior teeth are inclined palataly and result in crossbite. A problem may be also in mandibular width. As a general rule, maxillary or mandibular is used to indicate where the problem is located. Maxillary palatal crossbite implies a narrow maxillary arch; mandibular buccal crossbite, describing the same dental relationship, indicates excess mandibular width as the cause. Step 4 is to evaluate the dental arches in the AP dimension ( sagittal plane ), using both the dental casts in occlusion. In this dimension the orthodontist uses the Angle classification and merely supplements it by stating whether a deviation is skeletal, dentoalveolar, or both by cephalometric analysis. Step 5 is to evaluate the dentition from the standpoint of the vertical dimension, again using both the articulated dental casts and the lateral cephalometric film. Bite depth is used to describe the occlusal relationship. The possibilities are anterior open bite, anterior deep bite, posterior open bite and posterior collapsed bite. Again, the orthodontist must determine whether the problem is skeletal, dentoalveolar, or a combination of both by cephalometric analysis. At each step, as any problem is noted, it should be judged as mild, moderate, or severe. This method automatically produces a list of the patient´s orthodontic problems, in the sequence of the five steps. Space analysis: When crowding is present, an analysis of the space available for the teeth of both the maxillary and mandibular arches is needed. Space analysis means calculating the arch perimeter available for alignment of the teeth ( space available ) and comparing this dimension to the total mesiodistal diameter of the permanent teeth ( space required ). The underlying principle of this analysis is that only a certain amount of arch perimeter is available, whatever the mesiodistal dimension of the teeth may be. The orthodontist is limited by apical base or basal bone to the degree to which the line of occlusion can be changed. If there is less space available than required, the orthodontist must decide whether it will be necessary to extract teeth to produce the space required, whether the dental arch can be slightly expanded in the premolar region to gain additional space, or whether some reduction of tooth size can be accomplished by stripping enamel from the interproximal surfaces of teeth. Since one of the major treatment planning decisions in orthodontics is whether it is necessary to extract teeth, space analysis is a critical determination. When doing a space analysis procedure, the first step is to establish the amount of space required. This is the sum of the mesiodistal diameters of the teeth. In mixed dentition, the prediction tables and measuring the teeth on the bitewing radiograph have been advocated to obtain the size of unerupted teeth, and both are reasonably successful techniques. The best combination of precision and ease of measurement ( for appropriate population of northern European origin ) currently is obtained with the Tanaka-Johnston method, which uses the width of the lower incisors to predict the size of both the lower and upper canines and premolars. This method has good accuracy, and requires neither radiographs nor reference tables ( when the method is memorized ), which make it convenient. For a patient from a different racial background, measurements of unerupted teeth on radiographs, using a control for radiographic magnification, is recomended. Tanaka and Johnston Prediction Values: One half of the mesiodistal width of the four lower incisors +10. 5 mm = +11. 0 mm = Estimated width of mandibular canine and premolars in one quadrant Estimated width of maxillary canine and premolars in one quadrant The method of establishing the amount of space available, which is the arch perimeter, is a bit more difficult. A number of methods have been suggested. One method that has been used traditionally to measure the arch perimeter is a brass wire contoured over the cusps and incisal tips of the teeth from molar to molar and then straightened out. The wire should be contoured along the line of occlusion: the central fossa line of the upper and the buccal cusp line of the lower. The brass wire method requires considerable judgement regarding proper arch form. Another suggestion is to use a bow divider to measure segments along the arch at the alveolar crest and add the segments. Some orthodontists suggest using a hanging chain, which automatically establishes a catenary curve, as rapid and reliable method for establishing mandibular arch perimeter. The important point to remember is that we do not understand the factors responsible for determining dental arch form, and therefore it is not possible to establish the dental arch form for a specific individual. We know that there may be an inherent morphogenetic pattern for the dental arch that the orthodontist should maintain during treatment. If the dental arch is somewhat V-shaped it behooves the orthodontist not to change this into a U-shaped configuration. To do so would merely invite collapse. Because the mandibular arch clinically appears to be less adaptable to arch form changes, the mandibular arch perimeter is ussually the more critical to determine. Another aspect that must be considered in this analysis is the curve of Spee. If this curve is basically flat ( as can be determined merely by placing the occlusal surfaces of the teeth over the flat base of the other cast ), then there is no influence on the space analysis. If however, there is a deep curve that the orthodontist plans to flatten, additional arch perimeter will be required to accomlish this. Slightly less than 1 mm of additional arch perimeter is needed for each millimeter of leveling of the curve of Spee, if the arch is leveled through the second molars. A deep curve is frequently accompanied by mesially tipped mandibular posterior teeth. Many other factors are related to the decision ( to extract teeth or not ), such as the relative tooth size between the mandibular and maxillary teeth, particularly in the anterior region and the inclination of the incisor teeth. It is important to keep in mind that crowding and protrusion are different aspects of the same thing: the degree of crowding depends on whether the incisors are protrusive or retrusive, as well as on how much space exists within the arch. ( if the incisors are retrusive, they form smaller arch and crowding is more severe )