* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download TB Management Guidelines
Survey
Document related concepts
Transcript
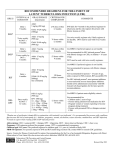
Guidelines for Management of Tuberculosis in Adults Section of Pulmonary Diseases, Critical Care and Environmental Medicine Department of Medicine - Tulane University School of Medicine New Orleans, Louisiana INTRODUCTION The initial decision to begin treatment for tuberculosis: The initial decision to treat is frequently empiric and founded on clinical judgment. The diagnosis of tuberculosis may be suggested by the clinical presentation, radiographic findings, and/or epidemiological information. In some cases, especially those with extrapulmonary disease, histopathologic findings may suggest the diagnosis. Supporting mycobacteriology data of positive AFB smears and cultures with identification and susceptibility data may not be available for days or weeks. The diagnosis of tuberculosis disease may be supported by evidence that indicates the presence of an underlying (latent) tuberculosis infection, i.e. positive tuberculin skin test (TST/ PPD) or positive interferon-gamma releasing assay (IGRA/ Quantiferon®-TB Gold). Remember that as many as 20-25% of active TB cases may have a negative TST at the time of diagnosis and that the sensitivity of the QFT-G in active TB has not been established. Positive AFB smears on sputum or tissue samples should be assumed to represent infection with Mycobacterium tuberculosis (M. tb) until culture with identification results are available. The ultimate defining data will be positive AFB cultures with identification of M. tb. The initial choice of anti-TB drugs is also empiric and assumes that the infecting TB bacillus will be susceptible to rifampin. Results of susceptibility testing is generally not available for 6-8 weeks or longer. The underlying principles for successful treatment of tuberculosis (TB) include: Multi-drug regimen containing two or more drugs to which the M. tuberculosis bacillus is susceptible, Drugs are given in adequate doses, Drugs are taken regularly, and Drugs are taken for a sufficient period of time. The most effective current regimens for the treatment of drug-susceptible M. tuberculosis (M. tb) contain a rifamycin which is the backbone of current antituberculous drug therapy. The addition of pyrazinamide during the first two months of treatment allows for effective 6 month, short course regimens. Treatment regimens for tuberculosis consist of an: Initial (Intensive) Phase (IP) of 8 weeks and a Continuation Phase (CP) of at least 4 months/18 weeks for a minimum total treatment period of 6 months/ 26 weeks. The preferred Initial Phase consists of the four first-line agents, Rifampin (RIF), Isoniazid (INH), Pyrazinamide (PZA), and Ethambutol (EMB) - “RIPE”. (The acronym “HRZE” is commonly used outside the U.S.) The preferred Continuation Phase for patients infected with pansusceptible M. tb consists of RIF and INH. An extended Continuation Phase (CP) of 7 months/ 31 weeks, for a total treatment period of 9 months/ 39 weeks, is recommended for patients with cavitary pulmonary tuberculosis (PTB), whose sputum AFB cultures remain positive after completion of the initial two months of therapy, and for patients whose Initial Phase of treatment did not include 8 weeks of PZA. 1 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 RECOMMENDED TREATMENT REGIMENS The American Thoracic Society, CDC, and the Infectious Diseases Society of America in their 2003 joint Statement on “Treatment of Tuberculosis” recommend four treatment regimens for drug susceptible M. tb.1 All four regimens are rifamycin based. Regimens 1+1a, 1+1b, and 2+2a are minimum six month/ 26 week, short-course treatment regimens that are in general use in the United States. Regimen 3, a regimen with three times weekly IP and CP, is not commonly used in the United States. This regimen is not currently used in Louisiana by the OPH TB Program. Regimens 1+1c and 2+2b, which have a Continuation Phase containing once weekly rifapentine, are rarely used in the U.S. and are not recommended for HIV-coinfected patients. Regimen 4, which does not include PZA, is for a period of minimum nine months. Ethambutol is included in the Initial Phase of all regimens when the local incidence of primary INH resistance exceeds the CDC threshold of 4%. INH resistance in Louisiana exceeds 4%. EMB is to be discontinued when susceptibility tests become available and indicate the M. tb bacillus is susceptible to both RIF and INH. All four regimens are based on the likelihood of drug susceptibility of M. tb to rifampin. SPECIFIC DETAILS FOR TREATMENT REGIMENS (See Attachment 1) Regimen 1 consists of an IP of daily RIPE for 8 weeks (40-56 doses) followed by Regimen 1a CP consisting of daily RIF and INH for 4 months/ 18 weeks (90-126 doses) for a total course of 6 months/ 26 weeks. or Regimen 1b CP consisting of twice weekly RIF and INH for 4 months/ 18 weeks (36 doses) for a total course of 6 months/ 26 weeks. Regimen 2 consists of an IP of daily RIPE for 2 weeks (10-14 doses) followed by twice weekly RIPE for 6 weeks (12 doses) and then followed by: Regimen 2a CP consisting of twice weekly RIF and INH for 4 months/ 18 weeks (36 doses) for a total course of 6 months/ 26 weeks. Regimen 3 consists of an IP of RIPE three times weekly for 8 weeks (24 doses) followed by RIF and INH three times weekly for 4 months/ 18 weeks (54 doses) for a total course of 6 months/ 26 weeks. Regimen 4 consists of an IP of daily RIF, INH, and EMB for 8 weeks (40-56 doses) followed by: Regimen 4a CP consisting of daily RIF and INH for 7 months/ 31 weeks (155-217 doses) for a total course of 9 months/ 39 weeks. or Regimen 4b CP consisting of twice weekly RIF and INH for 7 months/ 31 weeks (62 doses) for a total course of 9 months/ 39 weeks. Regimen 2+2a, with mostly twice weekly dosing, facilitates directly observed therapy programs and for this reason is utilized by many city/ county/ state public health department TB programs, including the Louisiana Office of Public Health (OPH). This is the default regimen for DOT in Louisiana. Regimens 1+1a, 1+1b and 2+2a all begin with daily RIPE for two weeks and all are for a total minimum duration of therapy of 6 months/ 26 weeks. You do not have to commit to the specific IP until 2 weeks of daily RIPE has been received. Patients receiving Regimens 1, 2 or 3 who have cavitary pulmonary tuberculosis with positive sputum AFB cultures after completing two months of therapy should receive an extended Continuation Phase of 7 months/ 31 weeks (155 5-day per week doses, 62 2 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 twice weekly doses, or 93 three times weekly doses) for a total treatment period of 9 months/ 39 weeks. An extended Continuation Phase of 7 months may also be considered for any patient whose response to treatment is considered suboptimal. Suboptimal response is indicated by delayed sputum culture conversion (>2 months), protracted fever and night sweats, and failure to gain weight. For individuals with very extensive/ “far advanced” pulmonary TB (bilateral, multilobar, cavitary disease), who are initially AFB-smear positive, the more intensive Regimen 1 consisting of an Initial Phase of daily RIPE for 8 weeks (40-56 doses) followed by one of two Continuation Phases, either Regimen 1a or 1b, may be preferable to the default Regimen 2+2a. Patients of especial concern are those with high bacterial burden as indicated by numerous (3-4+) AFB on smear and the presence of “large” and/or extensive cavities by imaging study. Regimen 1a CP consists of daily RIF and INH and Regimen 1b CP consists of twice weekly RIF and INH. For select patients Regimen 1+1b may represent a reasonable compromise between the all daily Regimen 1+1a and the largely twice weekly Regimen 2+2a. This would facilitate DOT. Another possible, non-standard, alternative would be 8 weeks of Regimen 1 IP with daily RIPE followed by Regimen 3a CP of three times weekly INH and RIF.* This decision re more intensive anti-TB therapy should be based on the clinical judgment of an expert in tuberculosis care. * A recent review of 20 trials of short-course treatment regimens, all containing rifampin, indicated relapse is directly related to the total dosage of drugs received. In the presence of cavitation, only all daily IP and CP or daily IP (8 weeks) plus three times weekly CP regimens had relapse rates <5%.2 Regimen 4, which does not include PZA, is not acceptable for 6 month, short course treatment. It is a minimum 9 month treatment regimen. Regimen 4 should only be utilized for those cases in which PZA cannot be utilized. For Regimen 4 an extended Continuation Phase of >7 months may be considered for patients with cavitary pulmonary tuberculosis whose sputum AFB cultures remain positive after two months of therapy. There are no established guidelines as to the duration of an extended continuation phase for Regimen 4. The total number of doses that a patient receives is more critical than the number of weeks or months that therapy is received. For DOT schedules CDC considers five-day-aweek dosing as equivalent to seven-day-a-week dosing. Five-day-a-week doses are given weekdays only; weekends are omitted. The total daily doses listed in the regimens above are given for both 5-day and 7-day per week dosing. Some TB experts prefer 7day per week daily dosing during the first two weeks of IP for patients with extensive, cavitary PTB or HIV-coinfection. Certain other clinical situations also may warrant 7-day a week dosing, e.g. TB meningitis in a child. Decisions regarding appropriate regimens and their duration for patients with very extensive pulmonary tuberculosis and/or suboptimal response should be based on clinical judgment by an expert in tuberculosis care. DRUGS AND DOSES Most anti-TB drug doses are modified based on lean body weight. INH and rifampin doses do not need to be weight adjusted for adult patients except those weighing <40 Kg. Doses for EMB and PZA are always weight based. Doses for all injectable agents (IA) and most other second-line drugs are weight based.1 For PZA and EMB the ATS/CDC/IDSA TB Statement (Table 4 and 5) provides a schedule of doses based on weight with three ranges of weight: 40-55 Kg, 56-75 Kg and 76-90 Kg.1 Anti-TB medications should only be dispensed with a 30 day supply at a time. 3 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 First Line Drugs: Rifampin (Rifadin®/ Rimactane®)† - The usual adult dose for daily, twice, and three-time a week schedules is 600 mg (approximately 10 mg/Kg with a maximum dose of 600 mg). For an adult with a lean body weight of less than 40 Kg (90 lb) consider a reduced dose of 450 mg. Available in 150 and 300 mg capsules and in parenteral formulation for IV use. Isoniazid / INH† - The usual adult dose for daily schedules is 300 mg (approximately 5 mg/Kg with a maximum dose of 300 mg). The usual dose for twice and three time a week schedules is 900 mg (approximately 15 mg/Kg with a maximum dose of 900 mg). For an adult with a lean body weight of less than 40 Kg (90 lb) consider a reduced dose of 200 mg for daily schedules and 600 mg for two and three times per week schedules. Available in 100 mg tablet and 300 mg scored tablet and in parenteral formulation for IM or IV use. Pyrazinamide† - PZA is required for effective short course (6 month) treatment regimens. The daily adult dose is 20-25 mg/Kg with doses of 1000, 1500, or 2000 mg for the three weight groups. 2000 mg is the maximum daily dose. The twice weekly dose is 35-50 mg/Kg with doses of 2000, 3000, or 4000 mg for the three weight groups. 4000 mg is the maximum twice weekly dose. For three time a week dosing see Table 4 in the ATS/CDC/IDSA TB Statement. The initial prescription should not exceed a 2 month supply (30 days plus one refill). PZA is relatively contraindicated in patients with symptomatic gout. For patients with renal insufficiency (CrCl <30ml/min) the dose schedule should be modified to 25-35 mg/Kg three times per week (not daily). Available in 500 mg scored tablets. Ethambutol (Myambutol®)† - The daily adult dose of EMB is 15-20 mg/Kg with doses of 800, 1200, or 1600 mg for the three weight groups. 1600 mg is the maximum daily dose. For older patients (>65 years) the daily dose should not exceed 15 mg/Kg. The twice weekly dose is 35-50 mg/Kg with doses of 2000, 2800, or 4000 mg for the three weight groups. 4000 mg is the maximum twice weekly dose. For three time a week dosing see Table 5 in the ATS/CDC/IDSA TB Statement. Exercise caution in older (>65 years) patients and patients with impaired (low) vision or renal function impairment. EMB has rarely been associated with optic neuritis; usually at doses >15 mg/Kg and for periods of >2 months. For patients with renal insufficiency (CrCl <30ml/min) the dose schedule should be modified to 15-25 mg/Kg three times per week (not daily). Available in 100 mg film-coated tablets and 400 mg scored tablets. Rifabutin (Mycobutin®) – Is frequently used as an alternative for rifampin in HIVcoinfected patients receiving HAART. The usual adult dose for daily, twice, or three times per week schedules is 300 mg (approximately 5 mg/Kg with a maximum dose of 300 mg). Rifabutin is generally only used for HIV-coinfected patients receiving HAART. See TB Treatment in HIV-coinfection below. Available in 150 mg capsules. Rifapentine – Rifapentine is used only in the CP. The usual adult dose for once weekly continuation phase with concomitant INH is 600 mg (approximately 10 mg/kg with a maximum dose of 600 mg). The relapse rate with this dose of rifapentine, especially in HIV-coinfected patients, is unacceptable. Currently this cannot be a recommended agent at this dose. There are studies in progress evaluating CP with rifapentine at doses of 900 and 1200 mg/ week. Available in 150 mg film-coated tablets. Rifamate® - This is a combination product containing 150 mg isoniazid and 300 mg rifampin per capsule. This combination capsule simplifies daily RIF and INH dosing. Some TB programs utilize Rifamate in combination with additional 300 mg INH tablets for twice-weekly DOT. Rifamate is available from the Louisiana OPH Pharmacy. Rifater® - This is a combination product containing 120 mg rifampin, 50 mg isoniazid, and 300 mg pyrazinamide per tablet. It is not acceptable for twice or three-time a week dosing. Rifater is not currently available from the Louisiana OPH Pharmacy. 4 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 † See the TB Drug Dose Table (Attachment 2). This table uses the 3 standard weight groups as suggested in the ATS/CDC/IDSA TB Statement and lists whole tablet (capsule) doses. Whole tablet (capsule) doses facilitate DOT. Second Line Drugs: Moxifloxacin (Avelox®) - The daily adult dose is 400 mg. There is no data to support intermittent dosing. There is limited experience with long-term dosing. Moxifloxacin has very promising activity in the treatment of tuberculosis. Two recent CDC trials have compared moxifloxacin with INH and EMB. Study 27 compared moxifloxacin with EMB (HRZM vs. HRZE). Study 28 compared moxifloxacin with INH (MRZE vs. HRZE). Analysis of results of these studies is incomplete, but is encouraging. Results of a recent Johns Hopkins study in Brazil were presented in abstract form at the September 2007 ICAAC meeting. They reported significantly better culture conversion at 2 months with a regimen containing moxifloxacin instead of EMB (85% vs. 68%). Available in 400 mg film-coated tablets and parenteral formulation for IV use. Cycloserine (Seromycin®) – The daily adult dose is 10-15 mg/Kg in divided doses (maximum of 1000 mg). May have significant, even severe, CNS adverse effects. Most patients cannot tolerate >750 mg/day. There is no data to support intermittent dosing. Available in 250 mg capsules. Ethionamide (Trecator®) – The daily adult dose is 15-20 mg/Kg in divided doses (maximum of 1000 mg). May have significant GI adverse effects and possible hepatotoxicity. Most patients cannot tolerate >750 mg/day. There is no data to support intermittent dosing. Available in 250 mg film-coated tablets. Amikacin (Amikin®) – The daily adult dose is 15 mg/kg per day (maximum of 1000 mg) and 10 mg/kg in persons >59 years of age (maximum of 750 mg) given IM or IV. The usual dose is 750-1000 mg as a single dose 3-7 days per week. After the first 2-4 months of therapy the frequency should be reduced to two to three times weekly. Available in parenteral formulation for IM or IV use. Capreomycin – The daily adult dose is 15 mg/kg per day (maximum of 1000 mg) and 10 mg/kg in persons >59 years of age (maximum of 750 mg) given IM or IV. The usual dose is 750-1000 mg as a single dose 3-7 days per week. After the first 2-4 months of therapy the frequency should be reduced to two to three times weekly. Available in parenteral formulation for IM use. Streptomycin – SM is of limited usefulness due to increasing drug resistance. The daily adult dose is 15 mg/kg per day (maximum of 1000 mg) and 10 mg/kg in persons >59 years of age (maximum of 750 mg) given IM or IV. The usual dose is 750-1000 mg as a single dose 3-7 days per week. After the first 2-4 months of therapy the frequency should be reduced to two to three times weekly. Exercise caution in older (>65 years) patients, due to vestibular toxicity. Available in parenteral formulation for IM use. Streptomycin is not FDA approved for intravenous administration. Vitamin Supplementation: Pyridoxine (B6) is given to selected patients receiving INH. It may be effective in the prevention of peripheral neurotoxic adverse effects of INH. Patients who should receive supplemental pyridoxine include those with diabetes mellitus, HIV-coinfection, malnutrition, chronic alcohol use, pregnancy or first 3 months postpartum, renal failure, or symptoms of peripheral neuropathy before or during INH therapy. The usual dose is 2550 mg daily. Louisiana OPH Pharmacy provides 50 mg tablets. DIRECTLY OBSERVED THERAPY Directly observed therapy (DOT) is the Standard of Care for patients with pulmonary tuberculosis (PTB) in the United States. 5 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 DOT programs in the metropolitan New Orleans area are the responsibility of the TB Disease Intervention Specialists (DIS) for OPH Metro Region 1 (Jefferson, Orleans, St. Bernard and Plaquemines Parish). Patients who reside in other Parishes are referred to DIS in their OPH Region. In Louisiana DOT is administered either daily or twice weekly and may be accomplished by several different schemes - field DOT, clinic DOT, or DOT by proxy. The TB Control Program gives priority for DOT to AFB-smear positive PTB patients and to HIV-coinfected TB patients. An individual treating physician may opt for self-administered daily therapy for a specific, responsible patient. Intermittent (twice or three times weekly) schedules and 5-day a week daily schedules are only to be used with DOT. Self-administered therapy is always daily, 7-days a week. Patients with “culture negative” or inactive PTB may be candidates for daily selfadministered therapy after the Initial Phase of 8 weeks DOT. DIS will make a recommendation, if appropriate. DOT generally is not utilized for adults with only extrapulmonary TB (EPTB). BASELINE EVALUATION AND MONITORING Sputum AFB studies: Identification of the AFB isolate as M. tuberculosis is essential. NAA (nucleic acid amplification) tests or PCR on sputum samples can provide early identification of M. tb and may be performed on both smear-positive and smear-negative initial sputum samples. A positive NAA or PCR test for M. tb is relatively specific. Culture identification of M. tb will generally require a minimum of 2-3 weeks and may take as long as 6-8 weeks. Drug susceptibility tests for RIF, INH, and EMB are routinely performed on the initial M. tb isolate. Isolates that are resistant to any of the first-line agents should have susceptibility testing done for the second-line agents. During the first 8 weeks of treatment, sputum for AFB smear and culture should be obtained at weekly intervals. If AFB smears remain positive at 8 weeks, continue to obtain weekly sputum samples until smear-negative status is achieved. After smearnegative status is achieved obtain sputum for AFB studies at least monthly until a minimum of two consecutive specimens are AFB culture-negative or until completion of therapy. Many patients will have difficulty in producing spontaneous sputum samples after several months of effective therapy. In those cases sputum induction with nebulized hypertonic (3-5%) saline may be necessary to obtain additional sputum samples. If sputum AFB cultures remain positive for M. tb after 3-4 months of treatment, repeat susceptibility tests, including second-line agents, should be requested. Radiographic studies: In addition to the baseline plain chest radiographs a chest CT scan at the time of initial diagnosis is very useful in determining the true extent of disease and cavitation. CT scans are especially useful in identifying apical disease and the presence of cavities. At a minimum repeat plain chest radiographs are obtained after 1 and 2 months of therapy and at the completion of therapy. Typically, radiographs are obtained after 1, 2, 4, and 6 or 9 months of therapy or at the completion of therapy. These follow-up films should be compared with prior studies including the “index” film. More frequent imaging should be obtained as clinically indicated. Patients with extensive disease may be considered for repeat CT imaging during or at the completion of therapy. It should be noted that patients with extensive disease at the time of diagnosis will typically have significant residual radiographic abnormalities after therapy is completed. This may include volume loss, fibrotic stranding, nodular densities, and residual cavities. The presence of residual radiographic disease does not increase the risk of relapse. Many pulmonary physicians would obtain repeat chest radiographs at 6 and 12 months after completion of treatment. Chemistries and CBC: Baseline blood tests with CBC (including differential and platelet count), CMP (comprehensive chemistry panel - including glucose, BUN, creatinine, ALT, AST, total bilirubin, and alkaline phosphatase), and uric acid should be obtained prior to initiating therapy. ALT is more specific than AST for hepatocellular injury due to drugs. 6 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 Repeat monthly ALT and AST should be obtained when: Baseline LFTs are abnormal Patient has preexisting liver disease (cirrhosis, viral hepatitis, etc.) Patient chronically and regularly consumes alcohol Patient takes concomitant hepatotoxic drugs (Rx or OTC) HIV-coinfection Pregnant or first 3 months postpartum Receiving the combination of PZA and RIF for >2 months Patients >35 years old should be considered for periodic testing. (If AST and ALT remain normal after 2 - 3 months of therapy may discontinue monthly testing.) Obtain complete hepatic panel if significant elevation of ALT and/or AST occurs. Obtain a repeat CBC with platelet count if a patient on RIF develops petechiae, easy bruising or bleeding tendencies. Periodic determination of uric acid should be performed for patients receiving PZA who have gout, baseline hyperuricemia, or are receiving PZA for >2 months. HIV test: All older adolescent and adult patients with suspected TB or confirmed TB infection or disease should have an HIV test. If there is no documentation of the patient’s HIV status at the initial encounter an HIV test is to be requested. If a patient is assessed to be “low risk” for HIV-coinfection, the physician may opt to omit HIV testing. In general, patients who decline HIV testing should be managed using the guidelines for HIV coinfected individuals. Hepatitis serology: Obtain serology for Hepatitis B and C if there is a history of undocumented hepatitis or if there are abnormal baseline AST/ ALT with possible risk factors for hepatitis, e.g. intravenous drug use, country of origin, etc. Review of systems: Cough and sputum production are usually the first symptoms to improve within weeks. Fever and night sweats also usually resolve within a matter of weeks, but can persist for 2 months. For patients who lost weight during their illness or who were underweight at the onset of their illness, weight gain is an important prognostic indicator. Weight and BMI should be closely monitored. Failure to gain weight is indicative of an increased risk for treatment failure or relapse. Vision assessment: Patients older than 65 years of age or expected to receive EMB for longer than 2 months should have a baseline vision exam. At each monthly visit patients taking EMB should be questioned regarding possible visual disturbances including decreased visual acuity, blurred vision or scotomata. Monthly testing of visual acuity and color discrimination is advised for patients taking doses exceeding 15-25 mg/Kg per day, for patients receiving EMB for longer than 2 months, and for patients >65 years old. Monthly face-to-face assessment: All patients receiving anti-TB therapy must be seen in person monthly by a healthcare professional, nurse or physician, for assessment of any symptoms of active TB, possible drug adverse effects and for compliance with therapy. In the New Orleans OPH Metro Region monthly nurse conferences are routinely done by the nurses at the Wetmore Clinic or the TB nurse at the local Parish Health Unit, either at clinic visits or by home visits. A nurse conference must occur to continue receiving medications each month. Patients on self-administered therapy are not to receive more than a one month supply of anti-TB medications at a time. Physician followup visits should be scheduled as appropriate, generally every 1-2 months. If adverse effects are an issue more frequent visits may be necessary. Some physicians will refer all physician follow-up TB care to OPH Regional TB Clinics such as the Wetmore TB Clinic. INFECTIVITY AND SPUTUM CONVERSION All patients with clinically suspected PTB should initially be considered to be infectious. 7 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 PTB patients with positive AFB smears, who are not on therapy or who have just started therapy, are infectious. Individuals with PTB, who have 3 consecutive negative AFB smears, are clinically improving, and have received a minimum of 2-3 weeks of anti-TB therapy may be considered “relatively” noninfectious. Patients with susceptible M. tb who are clinically improving, but who remain smear positive after 2-3 months of effective therapy, are potentially infectious and should be evaluated on a case-by-case basis. Patients with drug resistant strains of M. tb should be considered infectious until they have become AFB-culture negative. Patients with EPTB, who do not have pulmonary involvement, are not infectious. 80% of cases of PTB due to susceptible M. tb will become culture negative within two months of therapy and 90-95% will become culture negative within 3 months.1 For cases of smear positive PTB due to susceptible M. tb the mean time for conversion to a negative smear has been reported to range from 33 days3 to 38 days4. The mean time for conversion to a negative culture has been reported as 32 days3 to 34 ± 26 days4 (mean ± SD). The median time for conversion to a negative culture has been reported as 26 days.3 Note that culture conversion may occur before smear conversion, indicating the presence of nonviable TB bacilli. High initial sputum bacillary burden (cavitary disease and numerous AFB on smear) may result in delayed smear and culture conversion. HIV-coinfection does not affect the time to sputum smear or culture conversion. COMMON ADVERSE EFFECTS OF ANTI-TB DRUGS Every drug has the potential for adverse effects (AE) or adverse drug reactions (ADR). The FDA defines an adverse drug reaction (ADR) as “any undesirable experience associated with the use of a medical product in a patient”. There are some adverse effects that are mild, not serious, and do not require any change in therapy. Other AEs or ADRs are aggravating to the patient or even serious and possibly life-threatening, e.g. drug-induced liver injury and Stevens-Johnson syndrome. EMB is the least likely drug to cause most common adverse effects. Adverse effects in HIV-coinfected patients are especially troublesome. GI “upsets”, nausea, vomiting and abdominal discomfort: Are common with many anti-TB drugs. This may be more common when taking the larger twice weekly doses. Taking the drugs with food or the different drugs at different times may ameliorate the problem. Non-specific GI “upsets” are more common in regular, especially daily, users of alcoholic beverages. If GI symptoms develop after being on medications for several weeks or longer, LFTs should be obtained. AST >3x the ULN in the presence of GI symptoms is suggestive of hepatotoxicity. Skin rashes and pruritus: Are also common. INH can rarely cause an acneiform eruption. Minor itching and “rash” may be managed with OTC anti-histamines. More intense pruritus and/or frank urticaria may necessitate discontinuing medications. Pruritus may occur in as many as 6% of those receiving RIF. Rarely a type of “Redman syndrome” may occur with RIF. Skin eruptions with diffuse erythema and/ or associated fever require discontinuation of all TB medications. Initially all drugs should be held until the “rash” and other symptoms are substantially improved. This usually occurs within a few days. The medications can then be restarted one by one, at intervals of 2-3 days. The ATS/CDC/IDSA TB Statement suggests that RIF should be restarted first (as it is the most important agent), followed by INH, and then EMB or PZA. If the “rash” recurs the last drug added should be stopped. If no “rash” appears after the first three drugs have been restarted, the fourth drug should not be restarted unless it is considered essential. 8 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 Drug fever: Usually develops after several weeks of therapy. Fever due to tuberculosis itself can persist for as long as 2 months. Drug fever is frequently high and spiking. It typically resolves within 24-48 hours of stopping the offending medication. Once fever has resolved drugs can be restarted as outlined above. Medications causing drug fever generally can never be resumed. CNS complaints: Complaints of dysphoria (ill feeling), “off-balance”, memory problems, inability to concentrate, irritability, and sleep disturbances occur with some frequency due to INH. These symptoms can sometimes be controlled by taking INH at bedtime. INH rarely can induce seizures or cause frank psychosis. Arthralgias: May occur in patients receiving PZA. In patients with clinical gout PZA can precipitate an acute attack. This is associated with elevation of uric acid. In patients with normal renal function and elevated uric acid, probenecid is a very effective uricosuric agent. PZA adversely affects the metabolism of allopurinol, reducing its efficacy. Paresthesias: May occur due to INH, but are usually limited to those patients with coexisting risk factors for peripheral neuropathy such as diabetes mellitus, HIVcoinfection, malnutrition, excessive alcohol use, pregnancy and renal failure. Patients with any of these risk factors should receive supplemental pyridoxine 25-50 mg daily while receiving INH. Red-orange discoloration of bodily fluids: This discoloration, which includes urine, sweat, stool, semen, and tears, is a universal occurrence with rifamycins. Soft contact lenses, bed linens and clothing may be permanently stained. You must warn patients of this! Visual disturbances: Ethambutol has been associated with retro-bulbar neuritis, usually at daily doses exceeding 15 mg/Kg and for durations >2 months. Patients older than 65 years may be more vulnerable to optic AE. Three time weekly dosing may be less likely to cause optic AE. Caution patients re any changes in their vision. DRUG-INDUCED LIVER INJURY DILI / hepatotoxicity can be caused by isoniazid, rifamycins, and pyrazinamide.12 Most DILI is caused by INH or PZA. Abnormal baseline transaminases are an independent risk factor for DILI. Increasing age (>35 years old) is associated with an increasing incidence of hepatotoxicity due to INH. Hepatotoxicity is defined as elevated ALT >3x ULN with symptoms or ALT >5x ULN without symptoms. ALT >3x and<5x ULN is mild toxicity; ALT between 5 and 10x ULN is moderate toxicity; and ALT >10x ULN (or >500 units/L) is severe toxicity. INH may cause hepatocellular injury with increases in ALT and AST, ALT > AST. Frank DILI will exhibit an increase in bilirubin. Severe DILI may also cause an increase in alkaline phosphatase and prothrombin time. Rifampin more typically causes a cholestatic picture with disproportionate increases in bilirubin and alkaline phosphatase. RIF is an uncommon cause of DILI. The combination of PZA with RIF for 2 months as treatment of latent TB infection (LTBI) has been associated with an unacceptably high incidence of severe DILI. This combination is no longer recommended for treatment of LTBI. A modest increase in ALT and AST levels may occur in 10-20% of patients receiving INH. This “transaminitis” typically occurs during the first two to three months and generally resolves by the 3rd month of therapy. ALT and AST levels usually do not exceed 3x ULN. These patients are asymptomatic. An increase in ALT and AST with predominantly an increase in AST suggests that alcohol may be the culprit. When a diagnosis of DILI is made, ALL potentially hepatotoxic drugs must be stopped. Drugs are not restarted until the ALT has decreased to <2x ULN or to the pretreatment baseline values if there was preexisting liver disease. 9 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 As DILI may result in a protracted interruption of therapy, a new non-hepatotoxic regimen of 3-4 drugs should be instituted. A typical 3-drug regimen would consist of EMB, moxifloxacin and an injectable agent. Cycloserine can be added as a 4th drug. When LFTs have significantly improved, drugs are reintroduced, beginning with the least likely offender. As RIF is a less likely cause of DILI than INH or PZA, it is restarted first and LFTs are checked every 2-3 days. Generally the next drug can be restarted after 5-7 days. The ATS/CDC/IDSA TB Statement suggests restarting INH next. Again LFTs are checked every 2-3 days. If AST and ALT remain unchanged and DILI was not severe, PZA can be restarted for a trial. If PZA cannot be resumed and less that 6-7 weeks of PZA had been received prior to the development of DILI, treatment should adhere to the regimen outlined above for a non-PZA regimen (Regimen 4). DRUG - DRUG INTERACTIONS Every medication has the potential for drug-drug interactions, especially rifamycins. Less commonly, drug-drug interactions may occur with INH. Anti-retroviral therapy (ART): HAART (Highly Active Antiretroviral Therapy) may require the substitution of rifabutin for rifampin due to the numerous drug-drug interactions that can occur with rifampin, especially with protease inhibitors. Rifamycins‡: Rifampin is a potent inducer of the cytochrome P450 system. Problems related to drug-drug interaction with RIF include reduced efficacy of oral contraceptives and warfarin, methadone withdrawal, as well as effects on numerous other hepatic metabolized drugs. Alternative contraceptive measures are required while receiving RIF. Rifampin may necessitate a 50% increase in methadone dose and a 2-3 fold increase in warfarin dose. RIF also may decrease the effectiveness of most of the “statins” and of sulfonylureas, such as glyburide. Rifabutin is a less potent inducer of the cytochrome P450 system. Isoniazid: INH is an inhibitor of the cytochrome P450 system. Monotherapy with INH can lead to increased concentrations of some drugs including phenytoin, carbamazepine, and diazepam. INH inhibition effect on the cytochrome P450 system is usually offset by rifampin. Pyrazinamide: There is a drug-drug interaction with PZA and allopurinol which reduces the efficacy of allopurinol. ‡ For detailed information regarding rifamycin drug-drug interactions consult Table 12 in the ATS/CDC/IDSA TB Statement.1 DRUG RESISTANCE AND DRUG INTOLERANCE - Drug programs may have to be modified because of demonstrated in-vitro resistance or patient intolerance/ adverse effects. Intermittent dosing schedules of oral anti-TB drugs should not be used in treating tuberculosis caused by drug-resistant organisms.¹ A treatment regimen should always include a minimum of 2 drugs to which the TB organism is susceptible. Never add single agents at a time to a regimen. All patients with drug resistant TB should receive consultation from an expert in tuberculosis care. Isoniazid resistance (INHr) or intolerance: When INH cannot be used, RIF, PZA and EMB should be given for 6 months.1 The 2007 Up-To-Date® and the 2007 Treatment Guidelines from The Medical Letter® recommend a total treatment duration of 6 to 9 months8, 11, or 4 months after culture conversion.8 An alternative regimen for those patients who cannot tolerate PZA for more than the initial 2 months of treatment is RIF and EMB for a total of 12 months.1,11 Moxifloxacin or an IA may be added for INHr patients with extensive disease.1,11 Most TB experts would discontinue INH when the M. tb isolate is INH resistant. Patients with INHr M. tb who have positive AFB cultures at 2 months should receive 9 or more months of therapy. There are no established guidelines as to the duration of an extended continuation phase for INHr cases. 10 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 [A 2001 retrospective study of INHr TB cases from Texas suggested the duration of therapy should be ≥ 7 months. That study also supported daily or three times weekly administration of therapy as being preferable to twice weekly administration.9] Rifampin resistance (RIFr): For RIFr patients the accepted treatment regimen is INH, EMB, and moxifloxacin for 12-18 months supplemented with PZA for the first 2 months of therapy.1 An injectable agent (IA) may be included in the first 2 months for patients with more extensive disease or to shorten the duration of therapy to 12 months.1 The 2007 Up-To-Date® recommends a 12-18 month regimen of INH, EMB, and PZA with the possible addition of moxifloxacin throughout or an IA for 2-3 months.8 PTB patients with RIFr M. tb who have positive AFB cultures at 2 months should be treated for a total period of 18 months. In general patients with RIFr M. tb should receive 4 drug regimens. In actuality mono-resistance to RIF is vey uncommon; most cases are resistant to both INH and RIF, i.e. are MDR-TB. See below re Multi-drug resistance. Patients with RIFr TB require consultation from an expert in tuberculosis care. Rifampin intolerance: RIF intolerance is a more common problem than RIF resistance. For patients who are intolerant of rifamycins, but do not have RIF resistance, both the 2007 Up-To-Date® and the 2007 Treatment Guidelines from The Medical Letter® recommend 9-12 months of INH, EMB, and PZA with or without moxifloxacin or 18 months of INH and EMB.7,11 Pyrazinamide resistance, intolerance or contraindications: PZA resistance is rare. PZA is relatively contraindicated in patients with symptomatic, especially tophaceous, gout. Caution should be exercised with the use of PZA in patients with asymptomatic gout, base-line hyperuricemia or impaired renal function. When PZA cannot be used, Regimen 4+4 b is acceptable with an IP of daily RIF, INH, and EMB for 8 weeks followed by a Continuation Phase of either daily or twice weekly RIF and INH for 7 months (31 weeks). Those patients not receiving PZA during the Initial Phase of therapy and who remain sputum AFB culture positive at 2 months, should receive an extended duration of therapy. There are no established guidelines as to the duration of an extended continuation phase for patients not receiving PZA. Ethambutol resistance or intolerance: The inability to use EMB is generally not of clinical significance, unless there is resistance or intolerance to other first line agents. Moxifloxacin may be an acceptable alternative to EMB. (See notes re moxifloxacin above.) Multi-drug resistance and/or multi-drug intolerance: This presents a complex challenge in TB management. Multidrug-resistant (MDR) TB is defined as resistance to at least INH and RIF. True MDR-TB is uncommon in the U.S. Extensively drug-resistant TB (XDR-TB) is defined as resistance to RIF, INH, a fluoroquinolone, and either an aminoglycoside or capreomycin or both. XDR-TB is an increasing world-wide problem, but fortunately is rare in the U.S. Patient intolerance of several drugs, however, can occur. Intolerance may be the result of adverse effects or coexisting conditions which preclude the use of certain agents. Examples of coexisting conditions are severe liver disease (which precludes the use of hepatotoxic drugs), tophaceous gout (which precludes the use of PZA), and the elderly with impaired vision (which may preclude the use of EMB). For a patient with resistance or intolerance to both rifampin and INH an appropriate regimen would include EMB, PZA, moxifloxacin, and an IA for 18-24 months. Addition of a second line oral agent such as ethionamide or cycloserine may be considered for true MDR-TB, especially with extensive disease.1 The IA is usually given for 6 months. The regimen for MDR-TB should always include any first line agents to which the M. tb organism is susceptible plus moxifloxacin and an IA. Patients with multidrug intolerance, MDR-TB, or XDR-TB require consultation from an expert in tuberculosis care. 11 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 INTERRUPTIONS IN THERAPY Interruptions in therapy for TB are a common problem. (See Attachment 3) This may occur because of patient non-compliance or because of drug interruption(s) due to problems with adverse effects. Interruption during the Initial (Intensive) Phase: An interruption of therapy of ≥14 days during the IP requires that therapy be restarted from the beginning. If the interruption during the IP is <14 days, therapy should simply be continued to completion of the scheduled doses. If the IP is not completed within 3 months from the start of therapy it should be restarted from the beginning. Interruption during the Continuation Phase: If interruption of therapy occurs during the CP, appropriate management depends on the percentage of doses received. If the initial AFB smear was negative and ≥ 80% of the planned doses has been received, no additional therapy may be necessary. However, if the initial sputum AFB smears were positive, therapy should be continued to receive the total planned doses. For all cases of interrupted therapy repeat sputum for AFB smear and culture should be obtained. If these repeat cultures are positive, repeat susceptibility tests are necessary. If the repeat cultures are negative the patient could be treated as having culture-negative PTB and given an additional 4 months of anti-TB therapy. If the repeat AFB cultures are positive the treatment should be restarted from the beginning with a 4-drug regimen. When a patient has received ≤ 80% of the planned doses and the lapse has been < 3 months, treatment should be resumed to complete the planned full course of therapy within 6 months. If a patient has received ≤ 80% of the planned doses and the lapse has been ≥ 3 months the initial 4-drug regimen should be restarted from the beginning. This 4-drug regimen should be continued until results of the repeat susceptibility test are available. For patients with interrupted therapy who have positive repeat AFB cultures, consultation with an expert in tuberculosis care should be obtained. Strict DOT is essential in managing patients with a history of interrupted treatment. Patients who are noncompliant should be placed under quarantine by OPH. Close cooperation with the Regional TB Program Manager and DIS is necessary to assist in managing treatment interruptions. See also Management of the Noncompliant Patient below. RECURRENT TUBERCULOSIS (RELAPSE vs. REINFECTION) Recurrence of tuberculosis may represent relapse of treated disease or reinfection with a new strain of M. tb. Relapse after successful completion of an acceptable treatment regimen occurs in less than 5% of cases. Relapses usually occur as a result of poor patient noncompliance. Patients at greatest risk for relapse are those with cavitary disease and/or positive AFB cultures after 2 months of treatment. Most relapses occur within 12 months of completing therapy. Relapses in patients with initially drug susceptible M. tb typically occur with drug susceptible organisms. For HIV uninfected patients approximately 90% of relapses occur within 12 months and 70% within 6 months after completing therapy. HIV coinfected patients relapse slightly earlier with 78% occurring within 6 months. 13 Reinfection may occur, but is an uncommon event in HIV negative or HIV positive patients treated in the United States and Canada.13 In other countries, which have a 12 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 high incidence of tuberculosis, there is evidence of a much higher occurrence of exogenous reinfection. See also Treatment failure below. TB TREATMENT IN SPECIAL CIRCUMSTANCES HIV-coinfection: The six month treatment regimens are generally considered to be acceptable for HIV-coinfected patients with TB.1 Acceptable regimens include Regimens 1+1a, 1+1b, and 2+2a. For HIV-coinfected patients with profound immunosuppression, manifested by CD4+ cell counts <100 cells/μl, the recommended regimen is the all daily Regimen 1+1a, consisting of an IP of daily RIPE for 8 weeks (40-56 doses) and a CP of daily RIF and INH for a minimum of 4 months/18 weeks (90-126 doses).¶ Some experts have advised that therapy should be continued for a minimum of six months after sputum become AFB-culture negative. HIV-coinfected patients with positive AFB cultures at 2 months and/or other indication of a suboptimal response to anti-TB therapy should receive an extended 7 months/ 31 weeks CP of therapy for a total duration of 9 months. ¶ [A recent study from San Francisco suggests a decreased risk of relapse in HIV-coinfected patients who received all daily (5 or 7 days per week) therapy and were treated for longer than 6 months. This was not related to CD4+ cell counts or presence of cavitation.6] HIV-coinfected patients may experience a paradoxical reaction, manifest by a temporary exacerbation of symptoms, signs, or radiographic manifestations of tuberculosis, after beginning anti-TB treatment. These reactions presumably develop as a consequence of immune reconstitution brought on by antiretroviral therapy (Immune Reconstitution Inflammatory Syndrome [IRIS]) or, perhaps, by treatment of TB itself. The optimal timing of the initiation of HAART in antiretroviral-naive HIV patients with newly diagnosed TB remains controversial. Some studies have shown that HAART may shorten the time to sputum smear and culture conversion and lower mortality. Due to the risk of drug adverse effects and IRIS, many experts recommend delaying initiation of HAART for several months after starting anti-TB therapy. When HIV-coinfected patients are receiving HAART, rifabutin may have to be substituted for rifampin. Dose adjustments of rifabutin may be necessary when it is given with commonly used antiretroviral agents that are CYP3A inhibitors and inducers. See separate CDC guidelines for co-administration of rifampin and rifabutin with HAART.5 Anti-TB treatment for HIV-coinfected patients must be coordinated with the physician(s) managing their HIV disease. See the on-line CDC site “Managing Drug Interactions in the Treatment of HIV-Related Tuberculosis”.5 http://www.cdc.gov/tb/TB_HIV_Drugs/default.htm Culture-negative pulmonary tuberculosis: An individual diagnosed with clinical PTB and whose initial sputum AFB cultures have no growth after 6 to 8 weeks represents “culture-negative”, presumptive PTB. These individuals may be considered for an abbreviated 4 month version of Regimen 2+2a, consisting of an IP of RIPE for 8 weeks followed by a 2 month CP of RIF and INH. Therapy may be administered twice weekly after the initial 2 weeks of daily therapy. The abbreviated 4 month regimen is not recommended for HIV-coinfected patients. HIV-coinfected patients should receive a standard 6 month minimum regimen recommended for HIV-infected individuals. Inactive pulmonary tuberculosis: The above 4 month version of Regimen 2+2a may be utilized for an asymptomatic individual diagnosed as having inactive, culture-negative, radiographic PTB, who has not previously been adequately treated for TB. Extrapulmonary tuberculosis: The standard 6 month treatment regimens are utilized for treatment of extrapulmonary TB (EPTB) with several modifications. Bone and joint TB 13 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 should be treated for 6 to 9 months. CNS TB should be treated for 9 to 12 months. For other forms of EPTB, including lymph node, pleural, pericardial, genitourinary, abdominal, soft-tissue, and disseminated (miliary) disease, six month regimens are acceptable. Some experts recommend a 9 month course of therapy for severe disseminated disease. Approximately 20% of patients with pleural tuberculosis will have positive sputum AFB cultures. The abbreviated 4 month regimen is not intended for culture negative extrapulmonary TB (EPTB). These patients should receive the appropriate 6-12 month course of anti-TB treatment. It is common for EPTB cases to have negative AFB cultures from the site of infection. Liver disease: Patients with advanced liver disease may require a regimen with only one or no hepatotoxic drug. RIF should be included if possible. PZA and INH generally should not be used. An acceptable regimen that retains RIF would also include EMB, moxifloxacin, and cycloserine with or without an injectable agent (IA). An IA should be added for cases with extensive disease. The duration of treatment with such regimens should be 12-18 months, depending on the extent of the disease and response to treatment (sputum AFB culture status at 2 months). If severe liver disease necessitates a completely non-hepatotoxic regimen, a four drug program of EMB, moxifloxacin, cycloserine and an IA may be used. The duration of treatment with this regimen should be 18-24 months, depending on the extent of the disease and response to treatment (sputum AFB culture status at 2 months). Conventional treatment regimens generally can be used safely in patients with chronic liver disease, including hepatitis C, who have only modest ALT and AST elevations (< 23x ULN) and minimal bilirubin elevation. Some experts suggest weekly LFTs during the first 2 months of anti-TB therapy for patients with chronic liver disease. All patients with significant liver disease, including chronic active hepatitis B or C, require at least monthly LFTs (ALT, AST and total bilirubin) while receiving anti-TB therapy. Patients with advanced liver disease should receive consultation from an expert in tuberculosis care. Chronic use of alcohol and other potential hepatotoxins: Although chronic use of alcohol does increase the risk of DILI, it is more important that a person with TB take their antituberculous medications than that they stop drinking alcohol. If patients continue to regularly consume alcohol, especially daily, they will require close monitoring with periodic ALT and AST. Patients should be cautioned re the use of OTC drugs such as acetaminophen which are potential hepatotoxins. Regular use of prescription drugs which are potential hepatotoxins will also require close monitoring. Renal insufficiency and end-stage renal disease**: Many anti-TB agents are renally cleared. Dose adjustment is required for patients with significant renal insufficiency (CrCl <30 ml/min) or ESRD on dialysis. Dose adjustment is best accomplished by increasing the dose interval rather than decreasing the individual dose. Drugs that require renal dose adjustment include EMB, PZA, cycloserine, and all the injectable agents. RIF, INH and moxifloxacin do not require renal dose adjustment. Monitoring of drug serum concentration may be required, especially for injectable agents and EMB. ** For detailed information regarding renal dose adjustment consult Table 15 in the ATS/CDC/IDSA TB Statement.1 Diabetes mellitus: It has previously been recognized that type 1 diabetes mellitus increases the risk for development of TB. It is now apparent that type 2 diabetes mellitus also increases the risk for development of active TB. A random serum glucose should be obtained on all patients at the time of diagnosis of TB. Although there is some conflicting data, a recent (2007) study indicates that patients with PTB who have diabetes mellitus may initially have a higher bacillary load in sputum, delayed clearance of tubercle bacillus, and higher rates of multidrug-resistant infection.10 14 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 Pregnancy: The risk of morbidity and mortality from untreated TB during pregnancy is significantly greater than the risks of adverse maternal or fetal effects from first line TB drugs. None of the first line agents have been demonstrated to be teratogenic. INH, RIF and PZA are FDA Category C. EMB is FDA Category B. PZA is generally not recommended during pregnancy in the U.S., but is used by some TB experts. Injectable agents are not recommended during pregnancy. The safety of moxifloxacin has not been established in pregnancy. The standard regimen for a pregnant woman is the 9 month Regimen 4+4b with an IP of 8 weeks daily RIF, INH, and EMB followed by a CP of twice weekly RIF and INH for an additional 7 months/ 31 weeks. This regimen is also considered to be safe during breast-feeding. Treatment failure: Treatment failure is defined as persistently positive AFB cultures after 4 months of appropriate antituberculous therapy. This may be a result of drug resistance, patient noncompliance with the drug regimen, or drug malabsorption. It is a rare event with susceptible organisms and the use of DOT. New AFB culture and susceptibility data is essential for managing treatment failures. A fundamental principle in managing treatment failures is never to add a single drug to a failing regimen. Two and preferably three new drugs should be added to such a regimen. Patients with treatment failure require consultation from an expert in tuberculosis care and possible referral to a specialized treatment center. ¹ MANAGEMENT OF THE NONCOMPLIANT PATIENT Patients with active, infectious pulmonary tuberculosis represent a public health concern due to the potential for transmission of their infection to others. The Louisiana Public Health-Sanitary Code provides several mechanisms for dealing with patients with tuberculosis who may be uncooperative with their anti-TB treatment. Directly Observed Therapy (DOT) is the Standard of Care in Louisiana. Per CDC recommendation all patients receiving services from the OPH TB Program are enrolled in a voluntary program of compliance. They are asked to sign a Voluntary Patient Compliance Agreement. Patients may not attend school, go to their job site, or go shopping until it is determined they are non-infectious (smear negative). If the Regional DIS staff and TB Program Manager determine a patient is uncooperative after signing this agreement, OPH will then issue a Quarantine Order for Directly-observed Therapy. The patient’s place of residence (house, apartment, room, etc.) can be declared a Place of quarantine. For a patient who continues to be uncooperative, the State Health Officer may issue a Quarantine Order for Hospitalization. If the TB Program Manager and DIS anticipates that an individual will be uncooperative with this Quarantine order they may initiate a request for a Court order for Hospitalization. Patients who have been placed under a Quarantine Order for Hospitalization or a Court order for Hospitalization or who have problematic medical conditions, e.g. substance abuse, homelessness, complicating coexisting medical conditions, or an inadequate home support situation, may be referred to the Villa Feliciana Medical Complex (VFMC) Tuberculosis Unit for inpatient care. VFMC is a Louisiana Department of Health and Hospitals facility located in Jackson, Louisiana which provides long-term inpatient treatment for patients with tuberculosis. Referrals to VFMC are coordinated by the Regional TB Program Manager and the State TB Control Program staff. If a patient has not completed a full course of treatment at the time of their discharge from VFMC, the Regional TB Program Manager will initiate a new Voluntary Patient Compliance Agreement or issue a new Quarantine Order for Directly-observed Therapy effective until anti-TB treatment is successfully completed. 15 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 Attachment 1 ‡ When DOT is used, drugs may be given 5 days/week and the necessary number of doses adjusted accordingly. Although there are no studies that compare five with seven daily doses, extensive experience indicates this would be an effective practice. § Patients with cavitation on initial chest radiograph and positive cultures at completion of 2 months of therapy should receive a 7-month (31 week; either 217 doses [daily] or 62 doses [twice weekly]) continuation phase. ¶ Five-day-a-week administration is always given by DOT. Rating for 5 day/week regimens is AIII. # Not recommended for HIV-infected patients with CD4+ cell counts <100 cells/μl. ** Options 1c and 2b should be used only in HIV-negative patients who have negative sputum smears at the time of completion of 2 months of therapy and who do not have cavitation on initial chest radiograph (see text). For patients started on this regimen and found to have a positive culture from the 2-month specimen, treatment should be extended an extra 3 months From: Treatment of Tuberculosis, American Thoracic Society, CDC, and Infectious ‡ When DOT is used, drugs may be given 5 days/week and the necessary number of doses adjusted accordingly. Although there are no studies that compare five with seven daily doses, extensive experience indicates this would be an effective practice. § Patients with cavitation on initial chest radiograph and positive cultures at completion of 2 months of therapy should receive a 7-month (31 week; either 217 doses [daily] or 62 doses [twice weekly]) continuation phase. ¶ Five-day-a-week administration is always given by DOT. Rating for 5 day/week regimens is AIII. # Regimen 1b and 2a are not recommended for HIV-infected patients with CD4+ cell counts <100 cells/μl. ** Options 1c and 2b should be used only in HIV-negative patients who have negative sputum smears at the time of completion of 2 months of therapy and who do not have cavitation on initial chest radiograph (see text). For patients started on this regimen and found to have a positive culture from the 2-month specimen, treatment should be extended an extra 3 months Adapted from Table 2 in Treatment of Tuberculosis, American Thoracic Society, CDC, and Infectious Diseases Society of America. MMWR 2003; 52(No. RR-11): [3]¹ (See original source document for complete Table 2.) 16 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 Attachment 2 Drug Dosing Schedule for Treatment of Adults with Active Tuberculosis Suggested Isoniazid (INH) doses - 300 mg (& 100mg) tablets: Weight (Lean) Daily dose 40-55 Kg/ 90-121 lbs* 300 mg (1 tablet) 56–75 Kg/ 122-165 lbs 300 mg (1 tablet) 76–90 Kg/ 166-198 lbs 300 mg (1 tablet) † Twice weekly dose 900 mg (3 tablets) 900 mg (3 tablets) 900 mg (3 tablets) † (Approx 5 mg/Kg) (Approx 15 mg/Kg) †Maximum dose regardless of weight. *Lean body weight <40 Kg/ 90 lbs consider reduced dose of 200 mg/d and 600 mg twice weekly. Suggested Rifampin (RIF) doses - 300 mg (& 150 mg) capsules: Weight (Lean) Daily dose 40-55 Kg/ 90-121 lbs* 600 mg (2 capsules) 56–75 Kg/ 122-165 lbs 600 mg (2 capsules) 76–90 Kg/ 166-198 lbs 600 mg (2 capsules) † Twice weekly dose 600 mg (2 capsules) 600 mg (2 capsules) 600 mg (2 capsules) † (Approx 10 mg/Kg) (Approx 10 mg/Kg) †Maximum dose regardless of weight. *Lean body weight <40 Kg/ 90 lbs consider reduced dose of 450 mg/d and 450 mg twice weekly. Suggested Pyrazinamide (PZA) doses – 500 mg tablets: Weight (Lean) Daily dose 40-55 Kg/ 90-121 lbs 1,000 mg (2 tablets) 56–75 Kg/ 122-165 lbs 1,500 mg (3 tablets) 76–90 Kg/ 166-198 lbs 2,000 mg (4 tablets) † Twice weekly dose 2,000 mg (4 tablets) 3,000 mg (6 tablets) 4,000 mg (8 tablets) † (Approx 20-25 mg/Kg) (Approx 35 - 50 mg/ Kg) †Maximum dose regardless of weight. PZA is used during the 8 week Initial Phase. Prescription should be written with only one refill. Exercise caution in patients with gout, hyperuricemia or renal function impairment. Increase dose interval if CrCl <30 ml/min. Suggested Ethambutol (EMB) doses – 400 mg tablets: Weight (Leam) Daily dose 40-55 Kg/ 90-121 lbs 800 mg (2 tablets) 56–75 Kg/ 122-165 lbs 1,200 mg (3 tablets) 76–90 Kg/ 166-198 lbs 1,600 mg (4 tablets) † †† Twice weekly dose 2,000 mg (5 tablets) 2,800 mg (7 tablets) 4,000 mg (10 tablets)† (Approx 15-20 mg/Kg) (Approx 35-50 mg/Kg) †Maximum dose regardless of weight. ††Daily dose should not exceed 15 mg/Kg/day if >65 yo. Exercise caution in individuals with low vision or renal function impairment or >65 years old. Increase dose interval if CrCl <30 ml/min. EMB is to be discontinued if M. tb is susceptible to RIF and INH. Prepared by Dean B. Ellithorpe, M.D. Revised 10/01/2007 17 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 Attachment 3 From Treatment of Tuberculosis, American Thoracic Society, CDC, and Infectious Diseases Society of America. MMWR 2003; 52(No. RR-11): [41]¹ 18 TB MANAGEMENT GUIDELINES for ADULTS Revised 04/10/2008 REFERENCES: 1. Treatment of Tuberculosis, American Thoracic Society, CDC, and Infectious Diseases Society of America. MMWR 2003; 52 (No. RR-11). http://www.cdc.gov/mmwr/PDF/rr/rr5211.pdf 2. Chang KC, Leung CC, Yew WW, Chan SL, Tam CM. Dosing schedules of 6-month regimens and relapse for pulmonary tuberculosis. Am J Respir Crit Care Med 2006; 174:1153-1158. 3. Telzak EE, Fazal BA, Pollard CL, Turett GS, Justman JE, Blum S. Factors Influencing Time to Sputum Conversion Among Patients with Smear-Positive Pulmonary Tuberculosis. Clin Infec Dis 1997; 25:666–70. 4. Fortun J, Martın-Davila P, Molina A, Navas E, Hermida JM , Cobo J, et al. Sputum conversion among patients with pulmonary tuberculosis: are there implications for removal of respiratory isolation? Journal of Antimicrobial Chemotherapy 2007; 59: 794–798. 5. Managing Drug Interactions in the Treatment of HIV-Related Tuberculosis. CDC [online]. 2007. http://www.cdc.gov/tb/TB_HIV_Drugs/default.htm 6. Nahid P, Gonzalez LC, Rudoy I, de Jong BC, Unger A, Kawamura LM, Osmond DH, Hopewell PC, Daley CL. Treatment Outcomes of Patients with HIV and Tuberculosis. Am J Respir Crit Care Med 2007; 175:1199-1206. 7. Bass JB. General principles of the treatment of tuberculosis. 2007 UpToDate®. 8. Schluger NW. Diagnosis and treatment of drug-resistant tuberculosis. 2007 UpToDate®. 9. Escalante P, Graviss EA, Griffith DE, Musser JM, Awe RJ. Treatment of Isoniazid-Resistant Tuberculosis in Southwestern Texas. Chest 2001; 119:1730-1736. 10. Alisjahbana B, Sahiratmadja E, Nelwan EJ, Purwa AM, Ahmad Y, Ottenhoff THM, et al. The Effect of Type 2 Diabetes Mellitus on the Presentation and Treatment Response of PulmonaryTuberculosis, Clin Infec Dis 2007; 45:428–35. 11. Drugs for Tuberculosis. Treatment Guidelines from The Medical Letter® 2007; 5 (55): 15-22. 12. Saukkonen JJ, Cohn DL, Jasmer RM, Schenker S, Jereb JA, Nolan CM, et al. An Official ATS Statement: Hepatotoxicity of Antituberculosis Therapy. Am J Respir Crit Care Med 2006; 174:935–952. 13. Jasmer RM, Bozeman L, Schwartzman K, Cave MD, Saukkonen JJ, Metchock B, Khan A, Burman WJ and the Tuberculosis Trials Consortium. Recurrent Tuberculosis in the United States and Canada; Relapse or Reinfection? Am J Respir Crit Care Med 2004; 170:1360–1366. Guidelines prepared by Dean B. Ellithorpe, MD Clinical Professor of Medicine Tulane University School of Medicine New Orleans, LA Revised 04/10/2008 19