* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Blood - BrownsBiology
Cell theory wikipedia , lookup
Developmental biology wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Hematopoietic stem cell wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Hematopoietic stem cell transplantation wikipedia , lookup
Homeostasis wikipedia , lookup
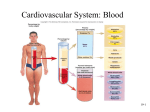
Unit 9 Blood is the only fluid tissue in the body Although it appears to be thick and uniform, it is actually composed of solid and liquid components Blood cells = formed elements Non-living fluid = plasma Red blood cells = erythrocytes White blood cells = leukocytes Erythrocytes make up ~45% of the volume of a blood sample this percentage is called the hematocrit Leukocytes make up less than 1% = buffy coat Plasma makes up the remaining ~55% Oxygenated blood looks bright red Deoxygenated blood looks dull red pH between 7.35 and 7.45 ~8% of body weight, 5-6 liters 90% water Contains over 100 different substances, including nutrients, metal ions, respiratory gases, hormones, proteins, and other cell metabolism products composition varies continuously Most abundant solutes are plasma proteins mainly made in liver, serve a variety of functions Albumin = helps maintain osmotic pressure of blood by keeping water in the bloodstream Clotting proteins stem blood loss Antibodies protect body from pathogens Plasma composition varies continuously, but is kept relatively constant through homeostatic mechanisms Acidosis = blood is too acidic Alkalosis = blood is too basic Liver, kidneys, respiratory organs, etc. work to keep plasma composition stable Plasma helps transport various substances and distribute body heat evenly throughout the body Red blood cells (RBCs) – carry oxygen to all cells in the body Don’t have a nucleus, very few organelles Mature RBCs are just sacs of hemoglobin molecules Hemoglobin (Hb) is a protein that contains iron and helps transport oxygen and carbon dioxide RBCs don’t have mitochondria make ATP using anaerobic respiration, so they don’t use the oxygen they are transporting Shaped like biconcave disks doughnuts Outnumber white blood cells 1000 to 1 1 RBC can carry 1 billion molecules of oxygen Increase in number of RBCs is called polycythemia A decrease in the oxygen carrying ability of the blood is called anemia Anemia can be caused by a decrease in the number of RBCs or by a lower hemoglobin content in the RBCs Sickle-cell anemia – abnormal hemoglobin causes RBCs to collapse and lose flexibility “sickle shape” These cells rupture easily and clog up small vessels Causes inhibited oxygen delivery, extreme pain, and advantage for surviving malaria parasite White blood cells – WBCs The only “complete” cells in the blood contain nuclei and organelles Defense against disease Able to slip in and out of blood vessels (diapedesis) Positive chemotaxis – WBCs can detect tissue damage, infection, etc. by “sniffing out” the chemicals these events release Leukocytosis – WBC count above average, indicates infection Leukopenia – low WBC count, usually caused by drugs Leukemia – “white blood,” bone marrow becomes cancerous and starts making huge numbers of WBCs Two major groups: ◦ Granulocytes = contain granules, have lobed nuclei Neutrophils = phagocytes, short-term or acute infections Eosinophils = kill parasitic worms, increase for allergies Basophils = contain histamine, cause inflammation and attract other WBCs ◦ Agranulocytes = lack visible granules, more spherical nuclei Lymphocytes = B lymphocytes make antibodies, T lymphocytes fight tumors and viruses (and reject grafts) and activate B lymphocytes Monocytes = long-term “clean-up team,” chronic infections Not exactly cells more like fragments of cells called megakaryocytes Needed for clotting process when blood vessels rupture or are broken Occurs in red bone marrow All blood cells start out as a hemocytoblast, a common type of stem cell Becomes either lymphoid or myeloid stem cell Lymphoid stem cell becomes lymphocyte Myeloid stem cell can become any other kind of blood cell RBCs are anucleate = they are unable to synthesize proteins, grow, or divide fall apart in 100 to 120 days Lost cells are constantly replaced by the division of hemocytoblasts in red bone marrow Erythropoietin = hormone that controls rate of RBC production, made by liver and kidneys Colony stimulating factors (CSFs) and interleukins = stimulate WBC production Thrombopoietin = stimulates platelet formation Hemostasis = stoppage of blood flow When a blood vessel wall breaks, a series of reactions is set in motion 1. Platelet plug forms – Platelets (which are normally repelled by healthy endothelium) stick to the now-exposed “sticky” collagen fibers. They release chemicals that attract more platelets until a platelet plug (white thrombus) is formed. 2. Vascular spasms occur – Platelet plug starts to release serotonin, which causes blood vessel to spasm. This narrows the blood vessel, which reduces blood flow. 3. Coagulation events occur – ◦ A. Injured tissues release thromboplastin, which plays important role in clotting. ◦ B. PF3 = phospholipid that coats surfaces of platelets. It interacts with thromboplastin, other clotting factors, and calcium ions to make an activator that triggers the clotting cascade. ◦ C. The prothrombin activator turns prothrombin to thrombin. ◦ D. Thrombin joins fibrinogen proteins into long, hairlike molecules called fibrin. The fibrin forms a “net” that traps RBCs and forms the clot. After an hour, the clot will start to retract, which squeezes out serum (plasma minus clotting proteins) and pulls the broken edges of the blood vessel closer together. Entire process normally takes 3-6 minutes Applying sterile gauze can speed up the process because the gauze provides a rough surface for platelets to stick to. Applying pressure will rupture nearby cells, which increases the release of thromboplastin. http://www.youtube.com/watch?v=9QVTHD M90io&feature=related Two major problems: too much clotting or not enough Too much clotting: ◦ Thrombus – a clot that develops and persists in an unbroken blood vessel ◦ Embolus – a thrombus that breaks away from the vessel and floats freely in the blood stream Not enough clotting: ◦ Thrombocytopenia – not enough platelets ◦ Hemophilia – hereditary disorder resulting in lack of any of the factors needed for clotting Plasma membranes of RBCs contain antigens. Antigens = substance the body can recognize as foreign stimulates release of antibodies to attack them Antibodies recognize “native” antigens and “foreign” antigens Antibodies will bind to foreign antigens and cause RBCs to clump together = agglutination This can cause blocked vessels, kidney blockage and failure, fever, chills, nausea, vomiting, etc. Over 30 RBC antigens, but the ABO and Rh antigens cause the most severe reactions Blood group RBC antigens Plasma antibodies Can receive from Can donate to AB A, B None A, B, AB, O (universal recipient) AB B B Anti-A B, O B, AB A A Anti-B A, O A, AB O None Anti-A, Anti-B O A, B, AB, O (universal donor) Rh factor – originally discovered in Rhesus monkeys Rh+ = RBCs carry Rh antigen Rh- = RBCs do not carry Rh antigen Anti-Rh antibodies are only formed after Rh antigens are detected in a Rh- person. If an Rh- woman is pregnant with a Rh+ baby, she must take RhoGAM right after delivery or she will develop anti-Rh+ antibodies that will attack her next pregnancy.