* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download schematic view - Autumn Symposium
Dental implant wikipedia , lookup
Dental hygienist wikipedia , lookup
Special needs dentistry wikipedia , lookup
Dental degree wikipedia , lookup
Remineralisation of teeth wikipedia , lookup
Tooth whitening wikipedia , lookup
Focal infection theory wikipedia , lookup
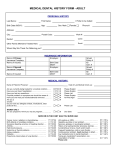
11th Annual Queensland Emergency Medicine Autumn Symposium – Dental Trauma Workshop 29th May 2015 Brisbane Convention Centre 1 Contents Chapters Tooth Numbering………………………………………………………………………………………..3 Dental Pain…………………………………………………………………………………………………4 Dental Infections…………………………………………………………………………………….......5 Dental and Maxillofacial Trauma………………………………………………………………....7 Post Dental Treatment Related Complications…………………………………………......9 Material Guidelines…………………………………………………………………………………...11 Dental Local Anaesthetic Techniques………………………………………………..………..12 References and acknowledgements……………………………………………………………17 2 A. TOOTH NUMBERING FDI – Federation Dentare International Two Digit System – Each digit pronounced separately 1. First Digit refers to Quadrant (Half a Mandible or Maxilla) Starts at top right maxillary quadrant and goes clockwise as you look at the patient SCHEMATIC VIEW 1 (5) 2 (6) 4 (8) 3 (7) 1 – Maxillary Right Quadrant (Permanent Dentition) 2 – Maxillary Left Quadrant (Permanent Dentition) 3 – Mandibular Left Quadrant (Permanent Dentition) 4 – Mandibular Right Quadrant (Permanent Dentition) 5 to 8 are for Deciduous Teeth. Repeats Quadrants in same order as permanent teeth. 5 – Maxillary Right Quadrant (Deciduous Dentition) 6 – Maxillary Left Quadrant (Deciduous Dentition) 7 – Mandibular Left Quadrant (Deciduous Dentition) 8 – Mandibular Right Quadrant (Deciduous Dentition) 2. Second Digit refers to tooth type and its closeness to the mid sagittal plane. 1 – Central Incisor (Permanent/Deciduous) 2 – Lateral Incisor (Permanent/Deciduous) 3 – Canine (Cuspid) (Permanent/Deciduous) 4 – 1st Premolar (Permanent) or 1st Molar (Deciduous) 3 5 – 2nd Premolar (Permanent) or 2nd Molar (Deciduous) 6 – 1st Permanent Molar 7 – 2nd Permanent Molar 8 – 3rd Permanent Molar Some examples: a. “13” – Right Maxillary Permanent Canine (pronounced as ‘ONE’ ‘THREE’) b. “25” – Left Maxillary Permanent 2nd Premolar c. “38” – Left Mandibular 3rd Permanent Molar B. DENTAL PAIN REVERSIBLE PULPITIS Short and sharp pain, disappears on removal of the stimulus, sensitivity to hot/cold/sweet stimuli Management: 1. 2. 3. 4. 5. 6. Advise patients to avoid foods that provoke pain Analgesics are not indicated Antibiotics are not indicated Cover any obvious cavity with an inert material (Eg Chewing Gum) Advise patient to see a dentist as soon as possible A simple restoration (filling) is usually sufficient IRREVERSIBLE PULPITIS Sharp and severe pain, becoming a dull throbbing ache that persists after removal of the stimulus, sensitive to hot/cold/sweet stimuli Management: 1. 2. 3. 4. 5. Advise patient to avoid foods that provoke pain Analgesics are indicated, especially NSAIDs if the patient can use them Antibiotics are not indicated Cover any obvious cavity with an inert material (Eg Chewing Gum) Infiltrate a local anaesthetic into the soft tissue adjacent to the root apex of the affected tooth for temporary relief if symptoms are severe 6. Advise patients to see a dentist as soon as possible 7. Either endodontic (root canal) treatment or extraction is usually needed 4 C. DENTAL INFECTIONS INFECTED ROOT CANAL SYSTEM WITH ACUTE APICAL PERIODONTITIS Dull ache, throbbing, may be sore to bite on, but not sensitive to hot/cold/sweet stimuli Management: 1. 2. 3. 4. Analgesics are indicated, especially NSAIDs if the patient can use them Antibiotics are not indicated Advise patient to see a dentist urgently Either endodontic (root canal) treatment or extraction is needed DENTAL ABSCESS (vestibular – localised in the buccal sulcus) Tender/ painful swelling in the region of recent toothache Management: 1. 2. 3. 4. Analgesics are indicated, especially NSAIDs if the patient can used them Antibiotics may be indicated Consider local anaesthetic away from the abscess site and lancing of the abscess. If swelling causing dysphagia or dyspnoea is present, IV antibiotic therapy and appropriate surgical management indicated 5. Advise patient to see a dentist urgently 6. Either endodontic (root canal) treatment or extraction is needed 7. Close monitoring of the airway is needed – if cellulitis develops, it can be life threatening SEVERE PERIODONTAL INFECTIONS – ACUTE ULCERATIVE GINGIVITIS Extremely painful infection of the periodontal tissues. Characterised by punched out interdental papillae, ulcers often covered with a greyish membrane and usually a fetid odour. Can be associated with systemic signs and symptoms. Commonly seen in young adult smokers. Management: 1. Local irrigation with chlorhexidine 2% mouthwash or hydrogen peroxide 3% solution 2. Smoking cessation 3. Antibiotic therapy with metronidazole 4. Analgesics 5. Advise patient to see their dentist as soon as possible 5 SPREADING ODONTOGENIC INFECTIONS Consequence of untreated localised odontogenic infection is that it may spread to surrounding tissues. Spreading odontogenic infections can be: 1. Superficial (Involving canine/buccal spaces) a. Can be treated with local surgical or dental treatment alone. b. In patients with severe superficial infections with swelling and systemic signs and symptoms, use antibiotic therapy in addition to local surgical or dental treatment. c. Advise patient to contact their dentist for prompt review if their condition deteriorates. d. All patients with infection should be reviewed within 48-72 hours of commencing treatment. e. If infection not resolved in 5 days, do not just repeat the antibiotic, check that pus has been drained, the cause removed and appropriate antibiotic is being used. f. Usually admission not required. 2. Deep (Involving the upper neck) a. Spreading to submandibular and pharyngeal spaces in upper neck are potentially life threatening, as there is a risk of airway obstruction. b. Any patient who has trismus, and cannot open their mouth more than 2cm (interincisal) must be assessed for signs of airway compromise. c. Look out for signs of stridor, dyspnoea, dysphagia and elevation and firmness of the tongue. d. Patients with deep infections and compromised airway must be assessed urgently by an oral and maxillofacial surgeon. e. Prescription of antibiotics without active dental treatment referral is not appropriate. f. Patient with systemic symptoms of pain and dehydration usually need to be managed in hospital, particularly if the infection is extensive. g. Management involves drainage, removal of the tooth, culture and susceptibilities of causative organisms, and treatment with IV fluid therapy and antibiotics. 3. Infraorbital/canine fossae space infections or swellings a. Risk of Cavernous Sinus Thrombosis – ascending infection arising from the maxillary teeth that travels via valveless anterior and posterior facial veins toward the brain. b. Presentation: 6 i. Exophthalmous ii. Oedema of the eyelids iii. Ophthalmoplegia (paresis of CN III, IV and VI) iv. Pain and fever c. Treatment: i. Admission, IV antibiotics and urgent oral and maxillofacial surgeon review. ii. If untreated will eventually lead to meningitis and encephalitis (high mortality) D. DENTAL AND MAXILLOFACIAL TRAUMA Crown Fracture 1. Enamel only – No need for emergency dressing 2. Enamel and dentine a. If large, dressing can be of assistance. b. Be aware tooth fragments could be embedded in lip laceration or inhaled. c. Treatment: i. Isolate teeth with gauze rolls in sulcus. ii. Apply Fuji IX Glass Ionomer Cement with a flat plastic or ball burnisher iii. Cover dentine just up to the fractured enamel iv. Ensure opposing tooth does not contact the dressing placed v. Once set the material can remain in the oral environment vi. Advise non chew diet 3. Enamel Dentine and Pulp a. Identify by bright red bleeding pulp in center of fracture b. Treatment: i. Isolate teeth with gauze rolls in sulcus ii. Dry blood and saliva off tooth using sterile water soaked gauze follow by dabbing with dry gauze iii. Apply DYCAL (Calcium Hydroxide liner) to cover pulp exposure with a DYCAL applicator iv. If DYCAL won’t stick, can apply pin head amount of topical EMLA cream on pulp to decrease pain and bleeding v. Seal the DYCAL with Fuji IX Glass Ionomer Cement with a flat plastic or ball burnisher/ Blu Tack Reinforced with Aluminium Foil vi. Ensure opposing tooth does not contact the dressing placed 7 vii. Advise non chew diet Root fractures 1. 2. 3. 4. Apical 1/3 fracture – no mobility/looseness of crown Mid Root 1/3 fracture – moderate mobility of crown Coronal 1/3 fracture – Just below the gum line, very poor prognosis Emergency treatment: a. Splinting techniques can be applied to stablise Luxations – Intrusion 1. 2. 3. 4. Teeth are usually pushed deeper into their sockets/bone. They are firm and don’t usually require splinting. Dental assessment is needed to decide correct treatment. Treatment options: a. Disimpaction and splinting b. Natural re-eruption and orthodontic extrusion c. As for emergency treatment: i. If there is concurrent crown fracture, treat as outlined above in the Crown Fracture section of this guideline. Luxations – Extrusion and Lateral luxations 1. 2. 3. 4. 5. Local anaesthetic will help with pain reduction. Two separate injections required. (Labial/Buccal and Palatal/Lingual) Use digital pressure to reposition tooth/teeth and alveolar bone. Check the biting with teeth in opposing jaw. Apply Splint Material. Avulsions 1. Deciduous teeth are best not reimplanted due to risk to infections and damage to permanent successors. 2. Best if tooth reimplanted in under 20 mins. 3. Storage mediums play and important role if tooth can’t be reimplanted quickly at the accident site. 4. Storage medium options a. Hanks Balanced Salt Solution Tissue Culture (HBSS) i. Excellent length of storage (24 hours) ii. Not easily obtainable in community settings b. Fresh Pasteurized Milk (Non Flavoured) i. Good practical alternative. 8 ii. Must be placed within 20 minutes of the accident. iii. Tooth can remain viable for 12-24 hours. iv. Best medium for public to use whether the patient is going to dentist immediately or afterhours to ED. c. Saliva expectorated into container i. Reasonable source, keeps periodontal ligament viable for 2 hours. d. Isotonic Saline i. Fair alternative viable for 1-2 hours. e. Tap water i. Poor Choice – viability only 20 minutes 5. Treatment: a. Handle tooth by crown and not handle root (prevent trauma to periodontal ligament) b. Wash tooth off dirt/milk/contaminants with running saline. c. Expand socket if necessary (remove blood clot with sterile instruments) and irrigate socket with saline. d. Reinsert tooth with care that the labial surface (convex surface) faces outwards. e. Apply Splinting material. f. Check bite with opposing jaw. (Biting relationship must not be excessive on reimplanted tooth) E. POST DENTAL TREATMENT RELATED COMPLICATIONS Management of Dental Haemorrhage 1. Causes: a. Anatomical – soft tissue or intrabony vessels bleeding b. Medications – Warfarin, Plavix (worse than Aspirin) c. Coagulopathies – Undiagnosed Von Willebrands Disease 2. Treatment: a. Local anaesthetic administered, retract cheek away, have good light source and assistance. b. Suture material – 3/0 Chromic Gut, 3/0 Slik, 3/0 Vicryl c. Pack socket with Surgicel/Gelfoam d. Suture Diagonally across socket x 2 (Buccal to lingual) e. Compress gauze over socket for 10 mins. Get patient to bite on this pack. f. Consider soaking gauze packs with 5% Tranexamic Acid Solution and compress socket for 10 mins. 9 g. Consider discharge with 5% Tranexamic Acid Mouthwash, 10-12ml rinse TDS for 2 days. h. Maxfacs referral if haemostasis not achieved. Dry Socket/Alveolar Osteitis 1. Incidence 3-5% for standard extractions, up to 30% for surgical extraction 2. Symptoms: a. Throbbing pain in extraction wound and adjacent teeth. b. Occuring 2-5 days after extraction. c. Pain referred to the TMJ. d. Not easily relieved by simple analgesics. e. Bad Taste 3. ‘Dry Socket’ is not a true infection of bone/fascial spaces but a failure of healing. Blood Clot disintegrates due to activation of plasminogen system, leaving painful exposed bony walls of socket. 4. Signs: a. Reddened gingiva around socket b. Partly or complete loss of blood clot from socket, food debris and necrotic tissue/clot lying in socket. c. Can be more difficult to visualize in lower 3rd Molars. d. Absence of true facial swelling or intra oral swelling 5. Treatment: a. Antibiotics of no real benefit. b. Irrigate socket with Curved Monojet (412) syringe with saline or dilute Chlorhexidine Mouthwash (0.12%) c. Placement of Alvogyl dressing (Septodent) with dental tweezers. d. This obtundant dressing has analgesic properties and stops further food entry into socket. e. It is slowly dissolved in the oral environment. Reassure patient. f. Push dressing lightly into the socket. No need to suture. g. May need changing by dental practitioner 2 days later. h. Most dry sockets resolve in 1-2 weeks. i. Alvogyl contents: i. Butamben (Benzocaine) ii. Iodoform iii. Eugenol iv. Penghawar v. CAUTION: Beware patients with hypersensitivity to IODINE. 10 F. MATERIAL GUIDELINES Splint options 1. 2. 3. 4. 5. 6. Elastoplast – on Labial/anterior surface of teeth Fibrin Glue Blu-tack covered with Aluminium Foil Zinc Phosphate Dental Cement with Aluminium Foil Fuji IX GIC with Aluminium foil Acid etch Composite Resin Dental filling material and Nylon Fishing Line/Paper Clip FUJI IX Mixing 1. Mixing time = 30 seconds, Working time = 2 minutes 2. Lightly tap powder bottle to unsettle powder, don’t evert 3. Dressing mix ratio = 1 drop of liquid: 1 scoop of powder (1gram liq: 3.6gram powder) 4. Use collar inside top of powder bottle to get level scoopful. 5. Divide powder into halves. Mix first half with plastic spatula in 10 seconds. The incorporate second half in 20 seconds. 6. For splinting: a. 8 drops: 4 scoops may be more appropriate for loading Aluminium mould (3 tooth mould) – more fluid like mix. Zinc Phosphate Cement Mixing (Havard or Hoffman’s Brand) 1. 2. 3. 4. Fast set type – working time = 90 seconds 7-8 drops of liquid dispense for average mix. Divide 2 dental spatula loads of powder into 4 equal parts on mixing pad/glass slab. Slowly incorporate first quarter into liquid. Then the next quarter a little faster. Last quarters is added as needed. 5. Consistency of mix is reached when on lifting the spatula, the point/drop formed slowly sinks back into the mixture. 6. After loading Aluminium Foil mould, assistant can scrap remaining cement into a small ball/mound to monitor the setting reaction. 7. Clean spatula and glass slab early with soapy water. Aluminium foil technique of splinting 1. 2. 3. 4. Use standard domestic cooking foil 5cm x 5cm squares enough for 3 teeth splint (For one avulsed tooth) 5cm x 8cm squares enough for 5 teeth splint ie, two avulsed teeth. Fold foil in half with matt side preferably outwards. 11 5. Fold in half two more times (8 layers for strength) 6. Remove excessive blood clots from crowns and neighbouring teeth with damp gauze. 7. Adapt foil to labial/anterior surface, incisal edge and palatal surface leaving 2-3mm clear of gingival margin. 8. Crimp foil in between teeth with fingernail to form a mould of the teeth crown. 9. Remove foil and fill bottom half with Dental material (Zinc Phosphate/FUJI IX) 10. Place foil on teeth – compress lightly and get patient to close teeth together. 11. Allow 2-3 mins to set (Looking at mixing pad to gauge speed of set) 12. Soft non chew diet G. DENTAL LOCAL ANAESTHETIC TECHNIQUES Armamentarium In a dental setting: 1. 27 Gauge (0.4mm) dental needle – long 38mm 2. Reusable dental syringe side loading or bridge loading (Stainless steel) 3. Dental Local Anaesthetic carpules (2.2ml or 1.8ml) a. 2.0% Lignocaine with 1:80,000 Adrenaline (Toxic dose 4.4mg/kg) b. 3.0% Prilocaine with 0.03IU/ml of Felypressin (Toxic dose 6.0mg/kg) In a medical setting: 1. 2. 3. 4. 5ml plastic syringe (narrower than 10ml syringe, easier for mouth) 23 Gauge (0.63mm) x 32mm needle 26 Gauge (0.45mm) x 13mm needle (infiltrations only, too short for IANB) 0.5% Bupivicaine with 1:200,000 Adrenaline (Toxic dose 1.5mg/kg) Maxillary Anaesthesia Names of common infiltration/field blocks are: a. b. c. d. e. f. Anterior Superior Alveolar Nerve Block (ASA) – Labial Sulcus Middle Superior Alveolar Nerve Block (MSA) Posterior Superior Alveolar Nerve Block (PSA) – Buccal Sulcus Infraorbital Nerve Block (IOB) – Labial Sulcus Greater Palatine Nerve Block (GP) – Palatal Hard Palate Nasopalatine Nerve Block (NP) – Incisive papilla on anterior palate 12 ASA, PSA, MSA Nerve blocks 1. Area anaesthetised: a. Pulp, Periodontal ligament, buccal bone, buccal/labial gum and periostium and sulcus mucosa of the following teeth: i. PSA - 1st, 2nd and 3rd molars ii. MSA – 1st , 2nd Premolars iii. ASA – Central and Lateral Incisor/Canine b. Success rate – 95% 2. Technique: a. Supra periosteal injection with bevel towards bone b. Aim at apical region (Root Tip) of the teeth being operated upon (Molars to Incisors) c. Puncture point – depth of sulcus (mucobuccal fold) d. Depth of penetration - 3-5mm, touch bone lightly and then withdraw slightly 0.5mm. Needle should be 30 degress to long axes of teeth. e. Deposit 1-1.5ml of solution over 30 seconds. Tissue ballooning is indicative of too shallow an injection and subsequent poor depth of anaesthesia. f. For PSA Block, target is apices of just superior to apices of 2nd and 3rd Maxillary Molar. Infraorbital Nerve Block (IOB) 1. Area anaesthetised: a. Area supplied by the ASA and MSA nerves as well as lower eyelid, upper lip and lateral aspect of nose. 2. Technique: (assume right hand operator giving right IOB) a. The infraorbital foramen is palpated externally with left index finger below the infraorbital rim. Felt as a distinct depression. Foramen lies on a line between pupil of eye and upper 2nd premolar. b. Retract lip with left thumb, keeping the left index finger over the infraorbital foramen. c. Puncture point is slightly lateral depth of sulcus adjacent to 1st or 2nd premolar. d. Index finger acts as a guide. e. Depth of penetration – 15-20mm to contact upper rim of foramen. f. After aspiration 1.0-1.5ml of solution deposited. Solution is massaged extraorally with finger to assist spread. 13 Palatal maxillary injections - Greater Palatine (GP) and Nasopalatine (NP) nerve block 1. Area anaesthesised: a. Palatal gum and mucosa, palatal bone and periostium – not pulps of teeth b. GP nerve block i. Anaesthetises broad area from GP foramen forward to 1st premolar/canine up to the midline on the roof of the palate. c. NP nerve block i. Anaesthetises anterior palate from incisive foramen back to canine area. d. Infiltration technique i. Anaesthetises palatal tissues just adjacent to needle puncture point. Smaller area compared to GP/NP nerve blocks. 2. Technique: (Infiltration) a. Puncture palatal mucosa adjacent to tooth being worked on, halfway between gingival margin and mid sagittal plane (midline of palatal roof) b. Needel perpendicular to palatal mucosa. c. 0.2-0.3ml slowly injected over 30-60 seconds. Can be painful. d. For GP Nerve Blocks, 0.5-0.6ml needed. Mandibular Injections Inferior Alveolar Nerve (IAN) Block 1. Area anaesthetised: a. Body of mandible, inferior portion of ramus b. Mandibular teeth to midline (pulp and periodontal ligament included) c. Buccal gum/soft tissue anterior to Mandibular 1st molar. d. Lingual soft tissue/Gum, Lingual(Medial) Periostium. e. Anterior 2/3 of tongue if lingual nerve included 2. Success rate – 85% a. Lower success rate compared to infiltrations in maxilla due to: i. Anatomical variation of height of Mandibular Foramen ii. Depth of Needle Penetration – 25mm iii. Intra Oral Landmarks not consistently reliable iv. Intravascular Injection possible 3. Technique: (assume right hand operator) a. Puncture point identification: i. Palpate external oblique ridge (Coronoid Notch) with left index finger, finger nail facing medially. ii. Identify pterygo-mandibular raphe (PMR) 14 b. c. d. e. f. g. h. i. j. k. l. iii. Identify Apex of buccal fat pad (Triangular shape) Puncture point is just lateral of the PMR at the apex of the buccal fat pad about the midpoint of left finger nail. Syringe body held over left premolar region with bevel of needle facing toward right mandible. Stretching tissues at puncture point with index finger prior to injection helps decrease pain. Insert needle 2-3mm, inject a few drops for pain control. Aim is to slowly advance needle to contact bone at 20-30mm depth (3/4 of long dental needle) Aspiration should be done to avoid intravascular injection, if +ve move needle tips 1-2mm and check again. If bone struck too early (ie 5mm) usually due to contacting the internal oblique ridge, withdraw needle 2-3mm, swing barrel of syringe over to a line parallel to Lower Right molars. Then insert deeper by 5-10mm, then swing syringe back to original position and advance to touch mandible at correct needle depth. If bone not touched at all after 30mm, don’t inject (risk of anaesthesising Facial Nerve (VII) ) Withdraw needle almost completely. Swing barrel further back on left side over molars and advance to strike bone at correct depth. If this fails, needle can be withdrawn completely and re-inserted 1-2mm more laterally. On difficult cases with broad divergent RAMI, bent needle technique is of assistance: i. Bend needle preferably with gloved fingers as instrument bending can lead too sharp a bend and metal fatigue. ii. Bend needle 20-30 degrees toward the bevel side in the lower 1/3rd of needle but not at the hub. This will ensure no breakage at the hub and relatively safe operator needle-stick injury risk. iii. Multiple bending at the hub increases needle fracture risks. Insert bent needle at same puncture point. Deposit 1-1.5ml (2/3rd dental cartridge) of solution after aspiration, slowly over 30-60 seconds. Withdraw majority of needle leaving approximately 10mm in the tissues. At this point, 0.5ml of solution is deposited for Lingual Nerve Anaesthesia. The lingual nerve will need to be anaesthesised if suturing any lingual gum in the Mandible. If inadequate lingual anaesthesia achieved, a repeat injection of 1ml of solution about 10mm in penetration in a slightly more lateral and inferior position than original puncture point. 15 Long Buccal Nerve Block 1. Area Anaesthetised: a. Gum and soft tissue (Sulcus) adjacent to mandibular 1st, 2nd and 3rd molars (lateral/buccal side) 2. Will need to anaesthetise this nerve in addition to IANB for suturing gingiva and extractions in this area. 3. Technique: a. Inject 0.5mls in sulcus depth, just posterior to Molar being worked on with Bevel toward Bone Mental Nerve Block (MNB) 1. Area anaesthetised: a. Buccal mucous membrane, gingiva and periosteum from mental foramen forward to the midline. b. Skin of Ipsilateral lower lip. c. Does not give lingual tissue anaesthesia. 2. Success rate – approaching 100%, 6% aspiration rate 3. Technique: (assume right hand operator) a. Palpate mental foramen in depth of sulcus adjacent to apex of 2nd Premolar. b. Stretch lower lip and buccal tissue with left index finger to improve visibility and keep tissues taut. c. Advance needle with bevel toward bone aiming at Mental Foramen. d. Injection depth is 6-10mm. e. Deposit 1ml of solution after aspiration. f. No need to directly enter Mental Foramen with needle. 16 References: 1. Hawkesford J & Banks JG. Maxillofacial and dental emergencies. Oxford University Press; 1994. 2. Malamed SF. Handbook of local anesthesia. 6th ed. St. Louis : Elsevier/Mosby; 2013. 3. Malamed SF. Medical emergencies in the dental office. 5th ed. St Louis: Mosby; 2000. 4. Acute Odontogenic and Salivary Gland Infections. Therapeutic Guidelines – Oral and Dental Version 2 , 2012 – p61 -69. 5. Hupp JR, Tucker MR, Ellis, E III. Complex Odontogenic Infections. Contemporary oral and maxillofacial surgery. 5th ed. St. Louis, Missouri : Mosby, 2008: 317-336. Helpful internet links: 1. http://www.endodonticgroup.com.au/files/trauma_poster_updated_8.9.11.pdf 2. http://www.dentaltraumaguide.org/ Acknowledgements: 1. Dr Dwight Elvery, BDSc, FRACDS, Lecturer at University of Queensland School of Dentistry. 2. Endodontic Group (www.endodonticgroup.com.au) 17