* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PDF
Survey
Document related concepts
Transcript
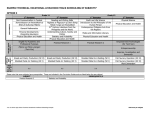
CASE REPORT Photoretinitis: an underestimated occupational injury? N. Magnavita Institute of Occupational Medicine, Catholic University School of Medicine, Largo Gemelli 8, 00168 Roma, Italy Non-ionizing radiation, which is produced in large amounts by welding arcs, may induce photophthalmia, keratoconjunctivitis and cataracts. Retinal injuries resulting from exposure to electric welding arcs have been reported, but such injuries are not commonly seen and may be misdiagnosed. A case is described of bilateral maculopathy in a millwright exposed to metal arc inert gas-shielded welding and oxygen lance light. Insurance adjudicators denied his claim, as they did not acknowledge the cause-and-effect relationship between welding and retinopathy. Welding emits a wide spectrum of radiation, ranging from IR to UV and beyond. UV and far-IR radiation are adsorbed by the cornea and the lens, whereas visible light and near-IR radiation penetrate to the retina. According to the intensity and time of exposure, they may cause thermal or photochemical retinal damage, which may be permanent and sight-threatening. Workers covered by compulsory collective insurance should be eligible for compensation in every case of welding light-induced retinal damage. Key words: IR light; occupational exposure; retinal injury; visible light; welding. Received 18 September 2001; revised 26 March 2002; accepted 30 April 2002 Introduction Traditionally, the ocular hazards of arc welding have been primarily considered to be photophthalmia (welder’s flash), keratoconjunctivitis and cataracts caused by UV radiation, which is produced in large amounts by welding arcs [1]. Retinal injuries resulting from exposure to electric welding arcs have been reported [1–7], but such injuries are not commonly seen. Here we report a case of welding arc maculopathy which failed to attain compensation from the Italian National Insurance Institute (INAIL), owing to supposed lack of a causative relationship. Subject The patient was a 45-year-old male who had been Correspondence to: N. Magnavita, Istituto di Medicina del Lavoro, Università Cattolica del Sacro Cuore, Largo Gemelli 8, 00168 Roma, Italy. Tel: +39 347 3300367; fax: +39 06 3054481; e-mail: nmagnavita@ rm.unicatt.it working for >25 years in industrial building framing, using electric arc welders, metal arc inert gas-shielded (MIG) and submerged arc welders, and oxygen lances. He was a skilled welder and had frequently suffered ocular pain from keratoconjunctivitis, or foreign bodies penetrating the eye. He never reported sick for such common eye problems. In September 1996, he complained of acute ocular pain while working at a welding arc. In the days that followed, when in the dark, he became aware of a persistent bright spot near the centre of his vision. He could not go on working, because he was unable to see the welding spots. He went to his general practitioner and was referred on to an ophthalmic hospital, still complaining of a positive scotoma affecting the lower part of his central field in both eyes, blurred vision (‘a tightly woven net, like a cobweb’) and photophobia. Ophthalmoscopic examination of the fundus revealed a circular bright-yellow foveal oedematous lesion in both eyes. The changes were most evident in the left eye. Computer-aided field examination showed scotoma in Occup. Med. Vol. 52 No. 4, pp. 223–225, 2002 Copyright © Society of Occupational Medicine. Printed in Great Britain. All rights reserved. 0962-7480/02 224 Occup. Med. Vol. 52, 2002 the nasal region of the left eye and remarkable sensitivity reduction in the corresponding area of the right eye. Anterior eye segments were normal. Visual evoked potentials (VEPs) were normal. The patient claimed worker compensation; INAIL declared that the worker was entitled to income lost through acute injury, but rejected the claim of permanent disability, asserting that there was no cause-and-effect relationship between the employment and the retinal lesion. Owing to visual impairment, the worker’s occupational performance significantly worsened and he was subsequently discharged from his job. Four years later, in February 2000, the patient came to our occupational health outpatient department, and underwent examination and further investigations at the university clinic. At the time, instead of the pain, a slight gritty feeling was present and visual acuity was reduced in both eyes. Pigmented foveal changes in locations corresponding to the retinal lesions and lack of foveal reflex were seen in the right eye, while chorioretinic paramacular atrophy was shown in the left eye. On automated static perimetry, visual field analysis showed enlargement of the blind spot in the left (22 absolute defects) and right eye (13 defects). VEPs were confirmed to be normal. Discussion Welding emits a wide spectrum of radiation, from IR to UV light and beyond. UV and far-IR radiation are adsorbed by the cornea and the lens, whereas visible light (VL) and near-IR radiation penetrate to the retina [1,4]. The cornea is sensitive to the effects of UV light and can suffer both acute and chronic toxicity. UV keratoconjunctivitis, or ‘arc-eye’, is a painful condition which is not considered a threat to sight in the long term [1]. It is associated with relatively short exposures to light sources, such as welding arcs or tanning lamps. The corneal effects are seen within a few hours following exposure and typically will resolve within 72 h. Chronic exposure to environmental UV light may lead to a variety of ocular surface abnormalities that rarely resolve in the absence of therapy [8–10]. Welding-arc-like injury may lead to secondary subretinal neovascularization [8]. There is a high prevalence and incidence of long-term changes in the outer part of the eye in welders [9,10]. Radiation in the visible and near-IR spectrum (400–1400 nm) penetrates the eye to be adsorbed by the retina and may cause thermal or photochemical damage, which may be permanent and sight-threatening, according to the intensity and duration of the exposure [4]. Retinal lesions induced by arc welding have been called ‘phototoxic maculopathy’ [3], ‘retinitis photoelectrica’ [4], ‘photic maculopathy’ [2] and ‘macular photoinjury’ [7]; all these definitions refer to identical pathology. Early diagnosis may be difficult, because maculopathy can be masked in the first few days by a phototoxic keratitis [7]. In most cases, retinal injuries heal spontaneously without loss of vision [1,4,6]. Severe burns of the macula, on the other hand, may lead to permanent complete or partial loss of central vision [1,4,7]. The prevalence and seriousness of the illness depend both on the intensity and characteristics of emitted radiation, and the availability of protective measures. Degenerative changes in the eye macula are very frequent among East European welders [11]. On the other hand, in Western countries, retinal lesions are infrequent and less well known by occupational health specialists. Occupational cases are scattered in the literature: two cases have been reported by Brittain [1] and three cases by Fich et al. [4]. A study of routine eye examinations of a general population showed that 0.14% of people who went to a primary eye care provider had photic maculopathy [12]; 15% of these were caused by looking at welding light without eye protection and the remaining by sungazing, substance abuse and psychiatric conditions [12]. MIG welding poses a greater threat to sight than other types of welding, because light emission is brighter and richer in VL and near-IR radiation than in a conventional rod arc [1]. Oxygen lances are even brighter than MIG welders. Protective lenses give no absolute protection [13]. In fact, radiation may be reflected into conventional welding helmets, thus causing undue exposure, even if work is performed at the welding desk [14]. There is anecdotal evidence that, in building yards, workers often have to lie on the floor or stretch in unnatural positions that do not allow the use of personal protective devices. They therefore cannot avoid looking momentarily at the intense light emitted from welders without any protection, especially when background light is insufficient. Moreover, in crowded workplaces, a worker may be exposed to the light emitted from another adjacent welder. Our patient sustained macular burns from MIG and/or oxygen lance welding. The seriousness of the lesion was not promptly recognized. The worker compensation system allocated benefits for days off work, but denied permanent disability, assuming that there was no causeand-effect relationship. The patient was recognized as disabled on the basis of a court’s verdict only in 2001, i.e. 5 years after the accident—when he had already lost his job. Causation is frequently a critical issue in worker compensation and liability cases. The question usually arises as to whether the condition was pre-existing or whether it was caused by an accident or occurrence that is not a subject of the claim in question. With an acute injury this determination should be simple. Before the injury, the worker had normal vision. He N. Magnavita: Photoretinitis had no other illnesses affecting the retina or other parts of the eye. This means that there was a high probability that retinal impairment arose as a result of the work in question. The available information suggests, with a reasonable degree of medical certainty, that exposure to MIG and/or oxygen lance welding caused the maculopathy. Better physicians’ knowledge of such an occupational injury would undoubtedly lead to early recognition of the problem, so decreasing workers’ impairment and reducing legal claims. A comprehensive approach to the management of retinal lesions should acknowledge both the individual and organizational levels of intervention. Preventive strategies should include good welding equipment, environmental background lighting, eye protection redesign and training of workers. Workers should be adequately informed about the danger of welding too close to the eyes and of looking round the side of the visor, even for a very short period. Workers should be advised to avoid ingestion of photosensitizing drugs, such as hydrochlorothiazide, furosemide, allopurinol, benzodiazepines [15] and fluphenazine [6], while welding. Early diagnosis of radiation retinopathy may be useful in reducing macular oedema by photocoagulation treatment [16], so improving vision in eyes with welders’ maculopathy. References 1. Brittain GP. Retinal burns caused by exposure to MIG-welding arcs: report of two cases. Br J Ophthalmol 1988; 72: 570–575. 2. Cellini M, Profazio V, Fantaguzzi P, et al. Photic maculopathy by arc welding. A case report. Int Ophthalmol 1987; 10: 157–159. 3. Denk PO, Kretschmann U, Gonzalez J, et al. Phototoxische Makulopathie nach Lichtbogenschweissen: Stellenwert des multifokalen ERG. Klin Monatsbl Augenheilkd 1997; 211: 207–210. 225 4. Fich M, Dahl H, Fledelius H, et al. Maculopathy caused by welding arcs. A report of 3 cases. Acta Ophthalmol Copenh 1993; 71: 402–404. 5. Garcia A, Wiegand W. Retinitis photoelectrica durch Elektroschweissen. Klin Monatsbl Augenheilkd 1989; 195: 187–189. 6. Power WJ, Travers SP, Mooney DJ. Welding arc maculopathy and fluphenazine. Br J Ophthalmol 1991; 75: 433–435. 7. Turut P, Isorni MC, Sicard C, et al. Phototraumatisme maculaire par ‘coup d’arc’ sur oeil implante. Bull Soc Ophtalmol Fr 1986; 86: 857–859. 8. Kozielec GF, Smith CW. Welding arc-like injury with secondary subretinal neovascularization. Retina 1997; 17: 558–559. 9. Narda R, Magnavita N, Sacco A, et al. Affezioni oculari nei saldatori: uno studio longitudinale. Med Lav 1990; 81: 399–406. 10. Norn M, Franck C. Long-term changes in the outer part of the eye in welders. Prevalence of spheroid degeneration, pinguecula, pterygium, and corneal cicatrices. Acta Ophthalmol Copenh 1991; 69: 382–386. 11. Gos R, Stepien J, Horowski P. State of the eyes in welders of Division M-5, Brown Coal Mine in Belchatow. Med Pr 1984; 35: 133–136. 12. Stokkermans TJ, Dunbar MT. Solar retinopathy in a hospital-based primary care clinic. J Am Optom Assoc 1998; 69: 625–636. 13. Arend O, Aral H, Reim M, et al. Welders maculopathy despite using protective lenses. Retina 1996; 16: 257–259. 14. Tenkate TS, Collins MJ. Angles of entry of ultraviolet radiation into welding helmets. Am Ind Hyg Assoc J 1997; 58: 54–56. 15. Mauget-Fa M, Quaranta M, Francoz N, BenEzra D. Incidental retinal phototoxicity associated with ingestion of photosensitizing drugs. Graefes Arch Clin Exp Ophthalmol 2001; 239: 501–508. 16. Kinyoun JL, Zamber RW, Lawrence BS, et al. Photocoagulation treatment for clinically significant radiation macular oedema. Br J Ophthalmol 1995, 79: 144–149.