* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Acute Renal Failure
Survey
Document related concepts
Transcript
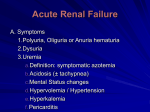
Acute Renal Failure Deb Goldstein Argy Resident September, 2005 Acute Renal Failure • Rapid decline in the GFR over days to weeks. • Cr increases by >0.5 mg/dL • GFR <10mL/min, or <25% of normal Acute Renal Insufficiency • Deterioration over days-wks • GFR 10-20 mL/min Definitions Anuria: No UOP Oliguria: UOP<400-500 mL/d Azotemia: Incr Cr, BUN • May be prerenal, renal, postrenal • Does not require any clinical findings Chronic Renal Insufficiency • Deterioration over mos-yrs • GFR 10-20 mL/min, or 20-50% of normal ESRD = GFR <5% of nl ARF: Signs and Symptoms • • • • • • • Hyperkalemia Nausea/Vomiting HTN Pulmonary edema Ascites Asterixis Encephalopathy Causes of ARF in hospitalized pts 45% ATN • Ischemia, Nephrotoxins 21% Prerenal • CHF, volume depletion, sepsis 10% Urinary obstruction 4% Glomerulonephritis or vasculitis 2% AIN 1% Atheroemboli ARF: Focused History • Nausea? Vomiting? Diarrhea? • Hx of heart disease, liver disease, previous renal disease, kidney stones, BPH? • Any recent illnesses? • Any edema, change in urination? • Any new medications? • Any recent radiology studies? • Rashes? Physical Exam • Volume Status – Mucus membranes, orthostatics • Cardiovascular – JVD, rubs • Pulmonary – Decreased breath sounds – Rales • Rash (Allergic interstitial nephritis) • Large prostate • Extremities (Skin turgor, Edema) W/U for ARF • Chem 7 • Urine – Urine electrolytes and Urine Cr to calculate FeNa – Urine eosinophils – Urine sediment: casts, cells, protein – Uosm • Kidney U/S - r/o hydronephrosis FeNa = (urine Na x plasma Cr) (plasma Na x urine Cr) FeNa <1% 1. PRERENAL • Urine Na < 20. Functioning tubules reabsorb lots of filtered Na 2. ATN (unusual) • Postischemic dz: most of UOP comes from few normal nephrons, which handle Na appropriately • ATN + chronic prerenal dz (cirrhosis, CHF) 3. Glomerular or vascular injury • Despite glomerular or vascular injury, pt may still have well-preserved tubular function and be able to concentrate Na More FeNa FeNa 1%-2% 1. Prerenal-sometimes 2. ATN-sometimes 3. AIN-higher FeNa due to tubular damage FeNa >2% 1. ATN • Damaged tubules can't reabsorb Na Calculating FeNa after pt has gotten Lasix... • Caution with calculating FeNa if pt has gotten Loop Diuretics in past 24-48 h • Loop diuretics cause natriuresis (incr urinary Na excretion) that raises U Na-even if pt is prerenal • So if FeNa>1%, you don’t know if this is because pt is euvolemic or because Lasix increased the U Na • So helpful if FeNa still <1%, but not if FeNa >1% 1. Fractional Excretion of Lithium (endogenous) 2. Fractional Excretion of Uric Acid 3. Fractional Excretion of Urea A 22yo male with sickle cell anemia and abdominal pain who has been vomiting nonstop for 2 days. BUN=45, Cr=2.2. A. ATN B. Glomerulonephritis C. Dehydration D. AIN from NSAIDs Prerenal ARF • Hyaline casts can be seen in normal pts – NOT an abnormal finding • • • • UA in prerenal ARF is normal Prerenal: causes 21% of ARF in hosp. pts Reversible Prevent ATN with volume replacement – Fluid boluses or continuous IVF – Monitor Uop Prerenal causes • Intravascular volume depletion – Hemorrhage – Vomiting, diarrhea – “Third spacing” – Diuretics • Reduced Cardiac output – Cardiogenic shock, CHF, tamponade, huge PE.... • Systemic vasodilation – Sepsis – Anaphylaxis, Antihypertensive drugs • Renal vasoconstriction – Hepatorenal syndrome Intrinsic ARF 1. 2. 3. 4. Tubular (ATN) Interstitial (AIN) Glomerular (Glomerulonephritis) Vascular You evaluate a 57yo man w/ oliguria and rapidly increasing BUN, Cr. A. B. C. D. ATN Acute glomerulonephritis Acute interstitial nephritis Nephrotic Syndrome ATN • Muddy brown granular casts (last slide) • Renal tubular epithelial cell casts (below) More ATN •Broad casts (form in dilated, damaged tubules) ATN Causes 1. Hypotension • Relative low BP • May occur immediately after low BP episode or up to 7 days later! 2. Post-op Ischemia • Post-aortic clamping, post-CABG 3. Crystal precipitation 4. Myoglobinuria (Rhabdo) 5. Contrast Dye – ARF usually 1-2 days after test 6. Aminoglycosides (10-26%) ATN—What to do • Remove any offending agent – IVF – Try Lasix if euvolemic pt is not peeing – Dialysis • Most pts return to baseline Cr in 7-21 days ATN Prerenal Cr increases at 0.3-0.5 /day U Na, FeNa increases slower than 0.3 /day UNa<20 FeNa<1% Normal UNa>40 FeNa >2% epi cells, granular casts Cr won’t Cr improves improve with IVF much 10-15:1 >20:1 UA Response to volume BUN/Cr Which UA is most compatible w/contrast-induced ATN? A. Spec grav 1.012, 20-30 RBC, 15-20 WBC, +Eos B. Spec grav 1.010, 1-3 WBC, 5-10 renal tubular cells, many granular casts, occasional renal tubular cell casts, no eos C. Spec grav 1.012, 5-10 RBC, 25-50 WBC, many bact, occasional fine granular casts, no eos D. Spec grav 1.020, 10-20 RBC, 2-4 WBC, 1-3 RBC casts, no eos ATN B. Spec grav 1.010, 1-3 WBC, 5-10 renal tubular cells, many granular casts, occasional renal tubular cell casts, no eos • Dilute urine: failure to concentrate urine • No RBC casts or WBC casts in ATN • Eos classically in AIN or renal atheroemboli, but nonspecific 56yo woman with previously normal renal function now has BUN=24, Cr 1.8. Which drug is responsible? A. B. C. D. Indinavir for her HIV Gentamicin for her SBE Motrin for her OA Cyclosporin for her SLE WBC Casts Cells in the cast have nuclei (unlike RBC casts) Pathognomonic for Acute Interstitial Nephritis Acute Interstitial Nephritis 70% Drug hypersensitivity • 30% Antibiotics: PCNs (Methicillin), Cephalosporins, Cipro • Sulfa drugs • NSAIDs • Allopurinol... 15% Infection • Strep, Legionella, CMV, other bact/viruses 8% Idiopathic 6% Autoimmune Dz (Sarcoid, Tubulointerstitial nephritis/Uveitis) AIN from Drugs Renal damage is NOT dose-dependent May take wks after initial exposure to drug • Up to 18 mos to get AIN from NSAIDS! But only 3-5 d to develop AIN after second exposure to drug • Fever (27%) • Serum Eosinophilia (23%) • Maculopapular rash (15%) • Bland sediment or WBCs, RBCs, non-nephrotic proteinuria • WBC Casts are pathognomonic! • Urine eosinophils on Wright’s or Hansel’s Stain – Also see urine eos in RPGN, renal atheroemboli... AIN Management • Remove offending agent • Most patients recover full kidney function in 1 year • Poor prognostic factors – ARF > 3 weeks – Advanced age at onset You evaluate a 32yo woman with HTN, oliguria, and rapidly increasing Cr, BUN. You spin her urine: A. ATN B. Acute glomerulonephritis C. Acute interstitial nephritis D. Nephrotic Syndrome Acute Glomerulonephritis • • • • RBC casts: cells have no nuclei Casts in urine: think INTRINSIC renal dz If she has Lupus w/recent viral prodrome, think Rapidly Progressive Glomerulonephritis If she had a sore throat 10 days ago, think Postinfectious Proliferative Glomerulonephritis What are these? Glomerular Dz • • • • • • Hematuria (dysmorphic RBCs) RBC casts Lipiduria (increased glomerular permeability) Proteinuria (may be in nephrotic range) Fever, rash, arthralgias, pulmonary sx Elevated ESR, low complement levels Rapidly Progressive Glomerulonephritis Type 1: Anti-GBM dz Type 2: Immune complex • IgA nephropathy • Postinfectious glomerulonephritis • Lupus nephritis • Mixed cryoglobulinemia Type 3: Pauci-immune • Necrotizing glomerulonephritis (often ANCA-positive, assoc. w/vasculitis) Can present with viral-like prodrome • Myalgias, arthralgias, back pain, fever, malaise Kidney bx : Extensive cellular crescents with or w/o immune complexes Can develop ESRD in days to weeks. Treat w/glucocorticoids & cyclophosphamide. Postinfectious Proliferative Glomerulonephritis • Usually after strep infxn of upper respiratory tract or skin – 8-14 day latent period – Can also occur in subacute bacterial endocarditis, visceral abscesses, osteomyelitis, bacterial sepsis • Hematuria, HTN, edema, proteinuria • Positive antistreptolysin O titer (90% upper respiratory and 50% skin) • Treatment is supportive – Screen family members with throat culture and treat with antibiotics if necessary A 19yo woman with Breast Cancer s/p chemo in the ER has weakness, fever, rash. WBC=15.4, Hct 24, Cr 2.9, LDH 600, CK=600. UA=3+ prot, 3+blood, 20 RBC. What next test do you order? What’s her likely dx? A. Nephrotic Syn B. Systemic Vasculitis C. Acute Glomerulonephritis D. Hemolytic-Uremic Syn E. Rhabdomyolysis TTP • Order blood smear to r/o TTP • TTP associated with malignancy, chemo • TTP may mimic Glomerulonephritis on UA (RBCs, WBCs) • Thrombocytopenia, anemia not consistent with nephrotic or nephritic syndrome • Need CK in the thousands to cause ARF Microvascular ARF • TTP/HUS • HELLP syndrome • Platelets form thrombi and deposit in kidneysGlomerular capillary occlusion or thrombosis • Plasma exchange, steroids, Vincristine, IVIG, splenectomy.... Macrovascular ARF • • • • Aortic Aneurysm Renal artery dissection or thrombosis Renal vein thrombus Atheroembolic disease – – – – New onset or accelerated HTN? Abdominal bruits, reduced femoral pulses? Vascular disease? Embolic source? Your 68yo male inpatient with baseline Cr=1.2 had negative cardiac cath 4 days ago, now Cr=1.8 and blanching rash. A. Renal Artery Stenosis B. ContrastInduced Nephropathy C. Abdominal Aortic Aneurysm D. Cholesterol Atheroemboli Why do his toes look like this? Renal Atheroembolic Dz 1% of Cardiac caths: atheromatous debris scraped from the aortic wall will embolize – Retinal – Cerebral – Skin (Livedo Reticularis, Purple toes) – Renal (ARF) – Gut (Mesenteric ischemia) • Unlike in Contrast-Induced Nephropathy, Cr will NOT improve with IVF • Diagnosis of exclusion: will NOT show up on MRI or Renal U/S; WILL show up on renal bx • Tx: supportive Post-Renal ARF • Urethral obstruction: prostate, urethral stricture. • Bladder calculi or neoplasms. • Pelvic or retroperitoneal neoplams. • Bilateral ureteral obstruction (neoplasm, calculi). • Retroperitoneal fibrosis. “Doc, your pt hasn’t peed in 5 hrs....what do you want to do?” • • • • Examine pt: Dry? Septic (vasodilated)? Flush foley (sediment can obstruct outflow) Check I/Os (has she been drinking?) Give IV BOLUS (250-500cc IVF), see if pt pees in next 30-60 min – If she pees, then she was dry – If she doesn’t pee, then she’s either REALLY dry or in renal failure • Check UA, UCx, urine lytes • Consider Renal U/S if reasonable You’re called to the ER to see... • A 35yo woman with previously normal renal function now with BUN=60, Cr=3.5. Do you call the Renal fellow to dialyze this pt? • What if her K=5.9? • What if her K=7.8? Indications for acute dialysis AEIOU • • • • • Acidosis (metabolic) Electrolytes (hyperkalemia) Ingestion of drugs/Ischemia Overload (fluid) Uremia • You admit this pt to telemetry and aggressively hydrate her. • You recheck labs 6h later and BUN=85, Cr=4.2. Suddenly the pt starts to seize. • Now what? Uremia—So what? • General – – • Mental status change – – – • Uremic encephalopathy Seizures Asterixis GI disturbance – • • Fatigue, weakness Pruritis Anorexia, early satiety, N/V, Uremic Pericarditis Plt dysfunction/bleeding A pt with chronic lung disease has acute pleuritic pain and desats to 92%RA. You want to r/o PE but her Cr=1.4. Can you get a CT with IV contrast? A. B. C. D. E. F. Send her for Stat CT with IV contrast Send her for Stat CT without IV contrast Just give her heparin Begin IV hydration Begin pre-procedure Mannitol Get a VQ scan instead Contrast-Induced Nephrotoxicity • Cr increases by 25% or >0.05 postprocedure • Contrast causes renal vasoconstriction renal hypoxia • Iodine itself may be renally toxic • If Cr>1.4, use pre-procedure prophylaxis Pre-Procedure Prophylaxis 1. IVF ( 0.9NS) 1-1.5 mg/kg/hour x12 hours prior to procedure and 6-12 hours after 2. Mucomyst (N-acetylcysteine) Free radical scavenger; prevents oxidative tissue damage 600mg po BID x 4 doses (2 before procedure, 2 after) 3. Bicarbonate (JAMA 2004) Alkalinizing urine should reduce renal medullary damage D5W with 3 amps HCO3; bolus 3.5 mL/kg 1 hour preprocedure, then 1mL/kg/hour for 6 hours postprocedure 4. Possibly helpful? Fenoldopam, Dopamine 5. Not helpful! Diuretics, Mannitol