* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Information for Prescribers - PCSS-MAT
Survey
Document related concepts
Transcript
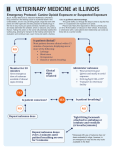
SAMHSA Opioid Overdose TOOLKIT: Information for Prescribers TABLE OF CONTENTS INFORMATION FOR PRESCRIBERS OPIOID OVERDOSE 3 TREATING OPIOID OVERDOSE 7 LEGAL AND LIABILITY CONSIDERATIONS 9 CLAIMS CODING AND BILLING 9 RESOURCES FOR PRESCRIBERS 9 ACKNOWLEDGMENTS, ETC. 11 n Acknowledgments n Disclaimer n PublicDomainNotice n ElectronicAccessandCopiesofPublication n RecommendedCitation n OriginatingOffice Also see the other components of this Toolkit: .FactsforCommunityMembers .FiveEssentialStepsforFirstResponders .SafetyAdviceforPatients&FamilyMembers .RecoveringfromOpioidOverdose: ResourcesforOverdoseSurvivors&FamilyMembers INFORMATION FOR PRESCRIBERS O pioidoverdoseisamajorpublichealthproblem,accountingfor almost17,000deathsayearintheUnitedStates[1].Overdose involvesbothmalesandfemalesofallages,ethnicities,and demographicandeconomiccharacteristics,andinvolvesbothillicit opioidssuchasheroinand,increasingly,prescriptionopioidanalgesics suchasoxycodone,hydrocodone,fentanylandmethadone[2]. Physiciansandotherhealthcareproviderscanmakeamajor contributiontowardreducingthetollofopioidoverdosethroughthe caretheytakeinprescribingopioidanalgesicsandmonitoringpatients’ response,aswellastheiracuityinidentifyingandeffectivelyaddressing opioidoverdose.FederallyfundedCMEcoursesareavailableatno chargeatwww.OpioidPrescribing.com(fivecoursesfundedbythe SubstanceAbuseandMentalHealthServicesAdministration)andon MedScape(twocoursesfundedbytheNationalInstituteonDrugAbuse). OPIOID OVERDOSE Theriskofopioidoverdosecanbeminimizedthroughadherencetothe followingclinicalpractices,whicharesupportedbyaconsiderablebody ofevidence[3-6]. ASSESS THE PATIENT. Obtainingahistoryofthepatient’spastuseof drugs(eitherillicitdrugsorprescribedmedicationswithabusepotential) isanessentialfirststepinappropriateprescribing.Suchahistoryshould includeveryspecificquestions.Forexample: n Inthepast6months,haveyoutakenanymedicationstohelpyou calmdown,keepfromgettingnervousorupset,raiseyourspirits, makeyoufeelbetter,andthelike? n Haveyoubeentakinganymedicationstohelpyousleep?Haveyou beenusingalcoholforthispurpose? n Haveyouevertakenamedicationtohelpyouwithadrugor alcoholproblem? n Haveyouevertakenamedicationforanervousstomach? n Haveyoutakenamedicationtogiveyoumoreenergyortocutdown onyourappetite? Thepatienthistoryalsoshouldincludequestionsaboutuseofalcohol andover-the-counter(OTC)preparations.Forexample,theingredients inmanycommoncoldpreparationsincludealcoholandothercentral nervoussystem(CNS)depressants,sotheseproductsshouldnotbe usedincombinationwithopioidanalgesics. Positiveanswerstoanyofthesequestionswarrantfurtherinvestigation. TAKE SPECIAL PRECAUTIONS WITH NEW PATIENTS. Manyexperts recommendthatadditionalprecautions betakeninprescribingfornewpatients [5,6].Thesemightinvolvethefollowing: 1. Assessment:Inadditiontothepatient historyandexamination,thephysicianshoulddeterminewhohasbeen caringforthepatientinthepast,what medicationshavebeenprescribed andforwhatindications,andwhat substances(includingalcohol,illicit drugsandOTCproducts)thepatient hasreportedusing.Medicalrecords shouldbeobtained(withthepatient’s consent). 2. Emergencies:Inemergencysituations, thephysicianshouldprescribethe smallestpossiblequantity,typicallynot exceedinga3days’supplyofanopioid analgesicandarrangeforareturn visitthenextday.Ataminimum,the patient’sidentityshouldbeverifiedby askingforproperidentification. 3. Limit quantities:Innon-emergency situations,onlyenoughofanopioid analgesicshouldbeprescribedto meetthepatient’sneedsuntilthe nextappointment.Thepatientshould bedirectedtoreturn to the officefor additionalprescriptions,astelephone ordersdonotallowthephysicianto reassessthepatient’scontinuedneed forthemedication. INFORMATION FOR PRESCRIBERS STATE PRESCRIPTION DRUG MONITORING PROGRAMS (PDMPs) have emergedas akeystrategyforaddressingthe misuseandabuse ofprescriptionopioids and thuspreventingopioid overdosesand deaths.Specifically, prescriberscan checktheirstate’sPDMPdatabase to determinewhetherapatientisfillingthe prescriptionsprovidedand/ orobtainingprescriptionsforthe sameorsimilar drug from multiple physicians. Whilem a n y statesnowhaveoperationalPDMPs,the programs differfrom stateto stateintermsofthe exactinformationcollected,how soon thatinformationisavailable to physicians,and whomay access the data.Therefore,informationaboutthe programinaparticularstate isbestobtaineddirectlyfrom the PDMPorfrom thestate boardof medicineorpharmacy. SELECT AN APPROPRIATE MEDICATION. Rationaldrugtherapy demandsthattheefficacyandsafetyofallpotentiallyuseful medicationsbereviewedfortheirrelevancetothepatient’sdiseaseor disorder[3,6]. Whenanappropriatemedicationhasbeenselected,thedose, schedule,andformulationshouldbedetermined.Thesechoicesoften arejustasimportantinoptimizingpharmacotherapyasthechoiceof medicationitself.Decisionsinvolve(1)dose(basednotonlyonage andweightofthepatient,butalsoonseverityofthedisorder,possible loading-doserequirement,andthepresenceofpotentiallyinteracting drugs);(2)timingofadministration(suchasabedtimedosetominimize problemsassociatedwithsedativeorrespiratorydepressanteffects);(3) routeofadministration(chosentoimprovecompliance/adherenceas wellastoattainpeakdrugconcentrationsrapidly);and(4)formulation (e.g.,selectingapatchinpreferencetoatablet,oranextended-release productratherthananimmediate-releaseformulation). Additionalsafeguardsarerecommendedbeforeprescribinganopioid analgesic.Forexample,evenwhensoundmedicalindicationshavebeen established,physicianstypicallyconsiderthreeadditionalfactorsbefore decidingtoprescribe[3,6]: 1. Theseverity of symptoms,intermsofthepatient’sabilityto accommodatethem.Reliefofsymptomsisalegitimategoalofmedicalpractice,butusingopioidanalgesicsrequirescaution. 2. Thepatient’sreliability in taking medications,notedthrough observationandcarefulhistory-taking.Thephysicianshouldassessa patient’shistoryofandriskfactorsfordrugabusebeforeprescribing anypsychoactivedrugandweighthebenefitsagainsttherisks.The likelydevelopmentofphysicaldependenceinpatientsonlong-term opioidtherapyshouldbemonitoredthroughperiodiccheck-ups. 3. Thedependence-producing potential of the medication.Thephysician shouldconsiderwhetheraproductwith lesspotentialforabuse,orevenanondrugtherapy,wouldprovideequivalent benefits.Patientsshouldbewarned aboutpossibleadverseeffectscaused byinteractionsbetweenopioidsand othermedicationsorillicitsubstances, includingalcohol. Atthetimeadrugisprescribed, patientsshouldbeinformedthatitis illegaltosell,giveaway,orotherwiseshare theirmedicationwithothers,including familymembers.Thepatient’sobligation extendstokeepingthemedicationina lockedcabinetorotherwiserestricting accesstoitandtosafelydisposingof anyunusedsupply(visithttp://www.fda. gov/ForConsumers/ConsumerUpdates/ ucm101653.htmforadvicefromthe FDAonhowtosafelydisposeofunused medications). EDUCATE THE PATIENT AND OBTAIN INFORMED CONSENT.Obtaining informedconsentinvolvesinformingthe patientabouttherisksandbenefitsofthe proposedtherapyandoftheethicaland legalobligationssuchtherapyimposes onboththephysicianandpatient[6]. Suchinformedconsentcanservemultiple purposes:(1)itprovidesthepatientwith informationabouttherisksandbenefits ofopioidtherapy;(2)itfostersadherence tothetreatmentplan;(3)itlimitsthe potentialforinadvertentdrugmisuse; and(4)itimprovestheefficacyofthe treatmentprogram. Patienteducationandinformedconsent shouldspecificallyaddressthepotential forphysicaldependenceandcognitive impairmentassideeffectsassociatedwith INFORMATION FOR PRESCRIBERS opioidanalgesics.Otherissuesthatshouldbeaddressedintheinformed consentortreatmentagreementincludethefollowing[6]: n Theagreementinstructsthepatienttostoptakingallotherpainmedications,unlessexplicitlytoldtocontinuebythephysician.Suchastatementreinforcestheneedtoadheretoasingletreatmentregimen. n Thepatientagreestoobtaintheprescribedmedicationfromonlyone physicianand,ifpossible,fromonedesignatedpharmacy. n Thepatientagreestotakethemedicationonlyasprescribed(forsome patients,itmaybepossibletoofferlatitudetoadjustthedoseas symptomsdictate). n Theagreementmakesitclearthatthepatientisresponsibleforsafeguardingthewrittenprescriptionandthesupplyofmedications,and arrangingrefillsduringregularofficehours.Thisresponsibilityincludes planningaheadsoasnottorunoutofmedicationduringweekendsor vacationperiods. n Theagreementspecifiestheconsequencesforfailingtoadheretothe treatmentplan,whichmayincludeweaninganddiscontinuationof opioidtherapyifthepatient'sactionscompromisehisorhersafety. Bothpatientandphysicianshouldsigntheinformedconsent agreement,andacopyshouldbeplacedinthepatient'smedicalrecord. Italsoishelpfultogivethepatientacopyoftheagreementtocarrywith himorher,todocumentthesourceandreasonforanycontrolleddrugs inhisorherpossession.Somephysiciansprovidealaminatedcardthat identifiestheindividualasapatientoftheirpractice.Thisishelpfulto otherphysicianswhomayseethepatientandintheeventthepatientis seeninanemergencydepartment. EXECUTE THE PRESCRIPTION ORDER. Carefulexecutionofthe prescriptionordercanpreventmanipulationbythepatientorothers intentonobtainingopioidsfornon-medicalpurposes.Forexample,federal lawrequiresthatprescriptionordersforcontrolledsubstancesbesigned anddatedonthedaytheyareissued.Alsounderfederallaw,every prescriptionordermustincludeatleastthefollowinginformation: Nameandaddressofthepatient Name,addressandDEAregistrationnumberofthephysician Signatureofthephysician Nameandquantityofthedrugprescribed Directionsforuse Refillinformation Effectivedateifotherthanthedateonwhichtheprescription waswritten Manystatesimposeadditional requirements,whichthephysician candeterminebyconsultingthestate medicallicensingboard.Inaddition, therearespecialfederalrequirements fordrugsindifferentschedulesofthe federalControlledSubstancesAct (CSA),particularlythoseinSchedule II,wheremanyopioidanalgesics areclassified. Blankprescriptionpads,aswell asinformationsuchasthenamesof physicianswhorecentlyretired,leftthe state,ordiedallcanbeusedtoforge prescriptions.Therefore,itisasound practicetostoreblankprescriptionsin asecureplaceratherthanleavingthem inexaminingrooms. NOTE:Thephysicianshouldimmediately reportthetheftorlossofprescriptionblanks tothenearestfieldofficeofthefederalDrug EnforcementAdministrationandtothestate boardofmedicineorpharmacy. MONITOR THE PATIENT’S RESPONSE TO TREATMENT. Properprescription practicesdonotendwhenthepatient receivesaprescription.Planstomonitor fordrugefficacyandsafety,compliance, andpotentialdevelopmentoftolerance mustbedocumentedandclearly communicatedtothepatient[3]. Subjectivesymptomsareimportant inmonitoring,asareobjectiveclinical signs(suchasbodyweight,pulserate, temperature,bloodpressure,andlevels ofdrugmetabolitesinthebloodstream). Thesecanserveasearlysignsof therapeuticfailureorunacceptable adversedrugreactionsthatrequire modificationofthetreatmentplan. Askingthepatienttokeepalogof signsandsymptomsgiveshimorhera senseofparticipationinthetreatment INFORMATION FOR PRESCRIBERS programandfacilitatesthephysician’sreview oftherapeuticprogressandadverseevents. Simplyrecognizingthepotentialfornonadherence,especiallyduringprolonged treatment,isasignificantsteptowardimproving medicationuse[7].Stepssuchassimplifying thedrugregimenandofferingpatienteducation alsoimproveadherence,asdophonecallsto patients,homevisitsbynursingpersonnel, convenientpackagingofmedication,and periodicurinetestingfortheprescribedopioid aswellasanyotherrespiratorydepressant. Finally,thephysicianshouldconveytothe patientthroughattitudeandmannerthatany medication,nomatterhowhelpful,isonlypart ofanoveralltreatmentplan. Whenthephysicianisconcernedabout thebehaviororclinicalprogress(orthelack thereof)ofapatientbeingtreatedwithan opioidanalgesic,itusuallyisadvisabletoseek aconsultationwithanexpertinthedisorderfor whichthepatientisbeingtreatedandanexpert inaddiction.Physiciansplacethemselvesat riskiftheycontinuetoprescribingopioidsin theabsenceofsuchconsultations[6]. CONSIDER PRESCRIBING NALOXONE ALONG WITH THE PATIENT’S INITIAL OPIOID PRESCRIPTION. Withproper education,patientsonlong-termopioidtherapy andothersatriskforoverdosemaybenefit fromhavinganaloxonekittouseintheevent ofoverdose[8]. Patientswhoarecandidatesforsuchkits includethosewhoare: n Takinghighdosesofopioidsforlong-term managementofchronicmalignantornonmalignantpain. n Dischargedfromemergencymedicalcarefollowingopioid intoxicationorpoisoning. n Athighriskforoverdosebecauseofalegitimatemedicalneed foranalgesia,coupledwithasuspectedorconfirmedhistoryof substanceabuse,dependence,ornon-medicaluseofprescriptionorillicitopioids. n Completingmandatoryopioiddetoxificationorabstinence programs. n Recentlyreleasedfromincarcerationandapastuserorabuser ofopioids(andpresumablywithreducedopioidtoleranceand highriskofrelapsetoopioiduse). Italsomaybeadvisabletosuggestthattheat-riskpatient createan“overdoseplan”tosharewithfriends,partnersand/or caregivers.Suchaplanwouldcontaininformationonthesigns ofoverdoseandhowtoadministernaloxoneorotherwiseprovide emergencycare(asbycalling911). DECIDE WHETHER AND WHEN TO END OPIOID THERAPY. Certainsituationsmaywarrantimmediatecessationofprescribing. Thesegenerallyoccurwhenout-of-controlbehaviorsindicatethat continuedprescribingisunsafeorcausingharmtothepatient[3]. Examplesincludealteringorsellingprescriptions,accidentalor intentionaloverdose,multipleepisodesofrunningoutearly(dueto excessiveuse),doctorshopping,orthreateningbehavior. Whensucheventsarise,itisimportanttoseparatethepatient asapersonfromthebehaviorscausedbythediseaseofaddiction, asbydemonstratingapositiveregardforthepersonbutno tolerancefortheaberrantbehaviors. Theessentialstepsareto(1)stopprescribing,(2)tellthe patientthatcontinuedprescribingisnotclinicallysupportable (andthusnotpossible),(3)urgethepatienttoacceptareferral forassessmentbyanaddictionspecialist,(4)educatethepatient aboutsignsandsymptomsofspontaneouswithdrawalandurge thepatienttogototheemergencydepartmentifsymptomsoccur, and(5)assurethepatientthatheorshewillcontinuetoreceive careforthepresentingsymptomsorcondition[6]. n Receivingrotatingopioidmedication regimens(andthusatriskforincomplete cross-tolerance). INFORMATION FOR PRESCRIBERS Identificationofapatientwhoisabusingaprescribedcontrolled drugpresentsamajortherapeuticopportunity.Thephysicianshould haveaplanformanagingsuchapatient,typicallyinvolvingworkwith thepatientandthepatient’sfamily,referraltoanaddictionexpertfor assessmentandplacementinaformaladdictiontreatmentprogram, long-termparticipationina12-Stepmutualhelpprogramsuchas NarcoticsAnonymous,andfollow-upofanyassociatedmedicalor psychiatriccomorbidities[3]. Inallcases,patientsshouldbegiventhebenefitofthephysician’s concernandattention.Itisimportanttorememberthatevendrugseekingpatientsoftenhaveveryrealmedicalproblemsthatdemand anddeservethesamehigh-qualitymedicalcareofferedtoany patient[3,6]. TREATING OPIOID OVERDOSE Inthetimeittakesforanoverdosetobecomefatal,itispossibleto reversetherespiratorydepressionandothereffectsofopioidsthrough respiratorysupportandadministrationoftheopioidantagonist naloxone(Narcan)[9].NaloxoneisapprovedbytheFDAandhasbeen usedfordecadestoreverseoverdoseandresuscitateindividualswho haveoverdosedonopioids. Thesafetyprofileofnaloxoneisremarkablyhigh,especiallywhen usedinlowdosesandtitratedtoeffect[8,9].Ifgiventoindividuals whoarenotopioid-intoxicatedoropioid-dependent,naloxone producesnoclinicaleffects,evenathighdoses.Moreover,whilerapid opioidwithdrawalintolerantpatientsmaybeunpleasant,itisnot typicallylife-threatening. Naloxoneshouldbepartofanoverallapproachtoopioidoverdose thatincorporatesthefollowingsteps. SignsofOVERMEDICATION,whichmay progresstooverdose,include[3]: n Unusualsleepinessordrowsiness n Mentalconfusion,slurredspeech, intoxicatedbehavior n Sloworshallowbreathing n Pinpointpupils n Slowheartbeat,lowbloodpressure n Difficultywakingtheindividual fromsleep Becauseopioidsdepressrespiratory functionandbreathing,onetelltalesignof anindividualinacriticalmedicalstateisthe “deathrattle.”Oftenmistakenforsnoring, the“deathrattle”isanexhaledbreathwith averydistinct,laboredsoundcomingfrom thethroat.Itindicatesthatemergency resuscitationisneededimmediately[8]. RECOGNIZE THE SIGNS OF OVERDOSE. Anopioidoverdose requiresrapiddiagnosis.Themostcommonsignsofoverdose include[3]: SUPPORT RESPIRATION. Supporting respirationisthesinglemostimportant interventionforopioidoverdoseand maybelife-savingonitsown.Ideally, individualswhoareexperiencingopioid overdoseshouldbeventilatedwith100% oxygenbeforenaloxoneisadministeredto reducetheriskofacutelunginjury[3,8]. Insituationswhere100%oxygenisnot available,rescuebreathingcanbevery effectiveinsupportingrespiration[8].Rescue breathinginvolvesthefollowingsteps: n Paleandclammyface n Verifythattheairwayisclear. n Limpbody n Withonehandonthepatient'schin,tilt theheadbackandpinchthenoseclosed. n Fingernailsorlipsturningblue/purple n Placeyourmouthoverthepatient's mouthtomakeasealandgive2slow breaths(thepatient'schestshouldrise, butnotthestomach). n Vomitingorgurglingnoises n Cannotbeawakenedfromsleeporisunabletospeak n Verylittleornobreathing n Veryslowornoheartbeat n Followupwithonebreathevery 5seconds. INFORMATION FOR PRESCRIBERS ADMINISTER NALOXONE.Naloxone(Narcan)shouldbe giventoanypatientwhopresentswithsignsofopioidoverdose, orwhenoverdoseissuspected[8].Naloxonecanbegivenby intramuscularorintravenousinjectionevery2to3minutes[8-10]. Themostrapidonsetofactionisachievedbyintravenous administration,whichisrecommendedinemergencysituations [9].Intravenousadministrationgenerallyisusedwithpatients whohavenohistoryofopioiddependence.Opioid-naivepatients maybegivenstartingdosesofupto2mgwithoutconcernfor triggeringwithdrawalsymptoms[8]. Theintramuscularrouteofadministrationmaybemore suitableforpatientswithahistoryofopioiddependencebecause itprovidesasloweronsetofactionandaprolongedduration ofeffect,whichmayminimizerapidonsetofwithdrawal symptoms[8]. Pregnant patients.Naloxonecansafelybeusedtomanageopioid overdoseinpregnantwomen.Thelowestdosetomaintain spontaneousrespiratorydriveshouldbeusedtoavoidtriggering acuteopioidwithdrawal,whichmaycausefetaldistress[8]. MONITOR THE PATIENT’S RESPONSE. Patientsshouldbe monitoredforre-emergenceofsignsandsymptomsofopioid toxicityforatleast4hoursfollowingthelastdoseofnaloxone (however,patientswhohaveoverdosedonlong-actingopioids requiremoreprolongedmonitoring)[8]. Mostpatientsrespondtonaloxonebyreturningto spontaneousbreathing,withmildwithdrawalsymptoms[8]. Theresponsegenerallyoccurswithin3to5minutesofnaloxone administration.(Rescuebreathingshouldcontinuewhilewaiting forthenaloxonetotakeeffect.) Thedurationofeffectofnaloxoneis30to90minutes. Patientsshouldbeobservedafterthattimeforre-emergence ofoverdosesymptoms.Thegoalofnaloxonetherapyshould berestorationofadequatespontaneousbreathing,butnot necessarilycompletearousal[8-10]. More than one dose of naloxone may be required to revive the patient. Those who have taken longer-acting opioids may require further intravenous bolus doses or an infusion of naloxone [8]. Therefore,itisessentialtogetthepersontoan emergencydepartmentorothersourceofacutecareasquickly aspossible,evenifheorsherevivesaftertheinitialdoseof naloxoneandseemstofeelbetter. SIGNS OF OPIOID WITHDRAWAL:Withdrawal triggeredbynaloxonecanfeelunpleasant.As aresult,somepersonsbecomeagitatedor combativewhenthishappensandneedhelpto remaincalm. Thesignsandsymptomsofopioidwithdrawal inanindividualwhoisphysicallydependenton opioidsmayinclude,butarenotlimitedto,the following:bodyaches,diarrhea,tachycardia,fever, runnynose,sneezing,piloerection,sweating, yawning,nauseaorvomiting,nervousness, restlessnessorirritability,shiveringortrembling, abdominalcramps,weakness,andincreased bloodpressure[9].Withdrawalsyndromesmay beprecipitatedbyaslittleas0.05to0.2mg intravenousnaloxoneinapatienttaking24mg perdayofmethadone. Inneonates,opioidwithdrawalalsomay produceconvulsions,excessivecrying,and hyperactivereflexes[9]. NALOXONE-RESISTANT PATIENTS:Ifapatient doesnotrespondtonaloxone,analternative explanationfortheclinicalsymptomsshouldbe considered.Themostlikelyexplanationisthat thepersonisnotoverdosingonanopioidbut rathersomeothersubstanceormayevenbe experiencinganon-overdosemedicalemergency. Apossibleexplanationtoconsideriswhether theindividualhasoverdosedonbuprenorphine, along-actingopioidpartialagonist.Because buprenorphinehasahigheraffinityforthe opioidreceptorsthandootheropioids,naloxone maynotbeeffectiveatreversingtheeffectsof buprenorphine-inducedopioidoverdose[8]. Inallcases,supportofventilation,oxygenation, andbloodpressureshouldbesufficienttoprevent thecomplicationsofopioidoverdoseandshould begiventhehighestpriorityifthepatient’s responsetonaloxoneisnotprompt. NOTE:Allnaloxoneproductshaveanexpirationdate. Itisimportanttochecktheexpirationdateandobtain replacementnaloxoneasneeded. INFORMATION FOR PRESCRIBERS LEGAL AND LIABILITY CONSIDERATIONS RESOURCES FOR PRESCRIBERS Health care professionals who are concerned about legal risks associatedwithprescribingnaloxonemaybereassuredbythefact thatprescribingnaloxonetomanageopioidoverdoseisconsistent withthedrug’sFDA-approvedindication,resultinginnoincreased liabilitysolongastheprescriberadherestogeneralrulesof professionalconduct.Statelawsandregulationsgenerallyprohibit physiciansfromprescribingadrugsuchasnaloxonetoathird party,suchasacaregiver.(Illinois,Massachusetts,NewYork,and WashingtonStatearetheexceptionstothisgeneralprinciple.)More informationonstatepoliciesisavailableatwww.prescribetoprevent. org/ or from individual state medical boards. Additional information on prescribing opioidsforchronicpainisavailableatthe followingwebsites: CLAIMS CODING AND BILLING Mostprivatehealthinsuranceplans,Medicare,andMedicaidcover naloxoneforthetreatmentofopioidoverdose,butpoliciesvaryby state.Thecostoftake-homenaloxoneshouldnotbeaprohibitive factor.Notallcommunitypharmaciesstocknaloxoneroutinelybut canalwaysorderit.Ifyouarecaringforalargepatientpopulation likelytobenefitfromnaloxoneyoumaywishtonotifythepharmacy whenyouimplementnaloxoneprescribingasaroutinepractice. ThecodesforScreening,BriefIntervention,andReferralto Treatment(SBIRT)canbeusedtobilltimeforcounselingapatient abouthowtorecognizeoverdoseandhowtoadministernaloxone. BillingcodesforSBIRTareasfollows: CommercialInsurance:CPT99408(15to30minutes) Medicare:G0396(15to30minutes) Medicaid:H0050(per15minutes) www.opioidprescribing.com. Sponsoredby theBostonUniversitySchoolofMedicine, withsupportfromSAMHSA,thissite presentscoursemodulesonvariousaspects ofprescribingopioidsforchronicpain.To viewthelistofcoursesandtoregister,goto http://www.opioidprescribing.com/overview. CMEcreditsareavailableatnocharge. www.pcss-o.org or www.pcssb.org. SponsoredbytheAmericanAcademyof AddictionPsychiatryincollaborationwith otherspecialtysocietiesandwithsupport fromSAMHSA,thePrescriber’sClinical SupportSystemoffersmultipleresources relatedtoopioidprescribingandthe diagnosisandmanagementofopioid usedisorders. www.medscape.com. Two course modules sponsoredbytheNationalInstituteon DrugAbuseandpostedonMedScapecan beaccessedathttp://www.medscape. org/viewarticle/770687 and http://www. medscape.org/viewarticle/770440.CME creditsareavailable. INFORMATION FOR PRESCRIBERS REFERENCES 1.CentersforDiseaseControlandPrevention(CDC).CDCgrand rounds:Prescriptiondrugoverdoses—AU.S.epidemic.MMWR Morb Mortal Wkly Rep.2012;61(1):10–13. 2.HarvardMedicalSchool.Painkillersfuelgrowthindrugaddiction; Opioidoverdosesnowkillmorepeoplethancocaineorheroin. Harvard Ment Hlth Let.2011;27(7):4–5. 3.BeletskyL,RichJD,WalleyAY.Preventionoffatalopioidoverdose. JAMA.2012Nov14;308(18):1863–1864. 4.IsaacsonJH,HopperJA,AlfordDP,ParranT.Prescriptiondruguse andabuse.Riskfactors,redflags,andpreventionstrategies.Postgrad Med.2005;118:19. 5.CoffinPO,SullivanSD.Cost-effectivenessofdistributingnaloxoneto heroinusersforlayoverdosereversal.Ann Internal Med. 2013;58:1–9. 6.FinchJW,ParranTV,WilfordBB,WyattSA.Clinical,legalandethical considerationsinprescribingdrugswithabusepotential.InRiesRK, AlfordDP,SaitzR,MillerS,eds.Principles of Addiction Medicine, Fifth Edition.Philadelphia,PA:Lippincott,Williams&Wilkins,Ch.109, inpress2013. 7.MichnaE,RossEL,HynesWL,etal.Predictingaberrantdrug behaviorinpatientstreatedforchronicpain:Importanceofabuse history.J Pain Symptom Manage.2004;28:250. 8.BMJEvidenceCentre.Treatmentofopioidoverdosewithnaloxone. British Medical Journal.UpdatedOctober23,2012.[AccessedMarch 24,2013,atwww.bmj.com] 9.RxList[AccessedMarch24,2013,atwww.rxlist.com] 10.Drugs.com[AccessedMarch24,2013,atwww.drugs.com] 10 Acknowledgments This publication was prepared for the Substance Abuse and Mental Health Services Administration (SAMHSA) by the Association of State and Territorial Health Officials, in cooperation with Public Health Research Solutions, under contract number 10-233-00100 with SAMHSA, U.S. Department of Health and Human Services (HHS). LCDR Brandon Johnson, M.B.A., served as the Government Project Officer. Disclaimer The views, opinions, and content of this publication are those of the authors and do notnecessarilyreflecttheviews,opinions,orpoliciesofSAMHSAorHHS. Public Domain Notice Allmaterialsappearinginthisvolumeexceptthosetakendirectlyfromcopyrighted sourcesareinthepublicdomainandmaybereproducedorcopiedwithout permissionfromSAMHSAortheauthors.Citationofthesourceisappreciated. However,thispublicationmaynotbereproducedordistributedforafeewithout the specific, written authorization of the Office of Communications, SAMHSA, HHS. Electronic Access and Copies of Publication This publication may be ordered from SAMHSA’s Publications Ordering Web page at www.store.samhsa.gov. Or, please call SAMHSA at 1-877-SAMHSA-7 (1-877-726-4727) (EnglishandEspañol). Recommended Citation SubstanceAbuseandMentalHealthServicesAdministration.SAMHSAOpioid OverdosePreventionToolkit:InformationforPrescribers.HHSPublication No.(SMA)13-4742.Rockville,MD:SubstanceAbuseandMentalHealthServices Administration, 2013. Originating Office Division of Pharmacologic Therapies, Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration, 1 Choke Cherry Road, Rockville, MD 20857. 11 HHS Publication No. (SMA) 13-4742 Printed 2013