* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Occlusive vascular disorders of the retina
Survey
Document related concepts
Photoreceptor cell wikipedia , lookup
Blast-related ocular trauma wikipedia , lookup
Fundus photography wikipedia , lookup
Visual impairment wikipedia , lookup
Vision therapy wikipedia , lookup
Idiopathic intracranial hypertension wikipedia , lookup
Mitochondrial optic neuropathies wikipedia , lookup
Retinal waves wikipedia , lookup
Macular degeneration wikipedia , lookup
Transcript
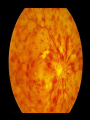
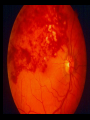
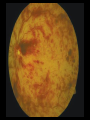
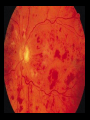
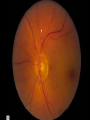
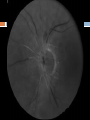
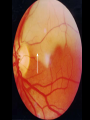
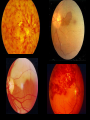
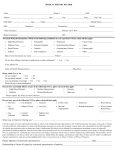
OCCLUSIVE VASCULAR DISORDERS OF THE RETINA AYESHA S ABDULLAH 27.02.2015 Learning outcomes By the end of this lecture the students would be able to Classify occlusive vascular disorders (OVD) of the retina. Correlate the clinical features of OVD of the retinal with the underlying pathophysiological changes. List treatment modalities for OVD List the complications of OVDs Retinal vein occlusion Central retinal vein occlusion (CRVO) Branch retinal vein occlusion (BRVO) Hemiretinal vein occlusion (HRVO) BRVO HRVO CRVO Epidemiology Retinal vein occlusion is the second most common cause of visual loss due to retinal vascular disease BRVO is the most common type It is a significant cause of severe visual loss in people over the age of 40 yrs Pathophysiology Can you think of some anatomical factors that could predispose retinal veins to occlusion? With occlusion of the central retinal vein (CRVO) increased venous & capillary pressure stagnation of the blood in the retinal venous system and increased resistance to venous blood flow ischemic damage to the retina increased production of vascular endothelial growth factor (VEGF) neovascularization of the posterior and anterior segment Neovascular Glaucoma , NVD, NVE,RD Capillary leakage Macular oedema CRVO The prognosis depends upon the reestablishment of patency of the venous system by recanalization, dissolution of clot, or formation of optociliary shunt vessels. Risk factors Blood Systemic Vessel wall Risk factors Age: 50% of these cases occur in patient over 65 years of age Systemic diseases like diabetes mellitus, hypertension, hyperlipidemics states, smoking & obesity Inflammatory diseases like sarcoidosis, Bechet disease Hyperviscosity syndromes like polycythemia, paraproteinemias Clotting disorders - Activated protein C resistance, lupus anticoagulant, anticardiolipin antibodies, protein C, protein S, antithrombin III Raised Intraocular pressure (IOP) Oral contraceptive use CRVO Clinical presentation Clinical entities Non –ischemic CRVO (about 75% of cases) Ischemic CRVO (worse prognosis) How would you diagnose retinal ischemia? CRVO Clinical presentation Asymptomatic Decreased vision Visual loss sudden or gradual, over a period of days to weeks. ranges from mild to severe. Patients can present with transient obscurations of vision initially, later progressing to constant visual loss. Photophobia Redness of eyes Painful blind eye Clinical examination Patients should undergo a complete eye examination, including visual acuity, pupillary reactions, slit lamp examination of the anterior and posterior segments, undilated examination of the iris….Why? gonioscopy, Dilated fundus examination Signs Visual acuity: (Best-corrected vision acuity) It is one of the important indicators of the final visual prognosis. Pupillary reactions: normal/ relative afferent pupillary reflex. If the iris has abnormal blood vessels, the pupil may not react. Conjunctiva: Advanced stages may show congestion on conjunctival and ciliary vessels. Cornea: Advanced stages may show diffuse corneal edema obscuring the visibility of internal structures. Iris: normal/ neovascularization The anterior chamber angle: it may show neovascularization with open angles and later show total peripheral anterior synechia and closed angles. Signs Fundus examination: Retinal hemorrhages Dilated tortuous veins Optic disc edema Cotton-wool spots Macular oedema Late signs: Neovascularization (NVD, NVE), optic disce cupping, optociliary shunt vessels at the disc (a prognostic sign), pigmentary changes in the macula Rubeosis – 100 day glaucoma Investigations Risk factors screening (Lab tests) FFA Electro-retinogram (ERG)- amplitude of the b-wave is decreased relative to the a-wave TREATMENT Depends on the type & stage of CRVO Principles of treatment are Treat the underlying cause Monitor Treatment modalities Intravitreal corticosteroid and anti-VEGF injections Dexamethasone intravitreal implant Laser photocoagulation Chorioretinal venous anastomosis Follow -up Regular follow –up “babysit" for these eyes during that period when they are at maximum risk of developing neovascular glaucoma, i.e. first 7-8 months Prognosis For nonischemic CRVO, complete recovery with good visual recovery occurs only in about 10% of cases. rd 50% of patients will have 6/60 or worse vision. About 1/3 of patients convert to ischemic CRVO within 3 years; 15% within the first 4 months. For ischemic CRVO, more than 90% of patients will have 6/60 or worse vision. About 60% of patients develop ocular neovascularization About 10% of patients can develop CRVO or other type of vein occlusions within either the same eye or the contralateral eye within 2 years. Conclusion a 54-year-old school teacher presented with acute visual loss in the left eye. He had history of uncontrolled hypertension and open angle glaucoma. Laboratory tests including complete hypercoagulability state and thrombotic workup were completed. Ophthalmologic exam showed best corrected visual acuity (BCVA)of 6/9 OD, 6/60 OS . Pupil exam showed sluggish left pupil with relative afferent papillary defect, and a reactive pupil on the right side. Intraocular pressures were 11 mmHg in the right, and 19 mmHg in the left. Slit lamp exam showed normal anterior segments with open angles bilaterally. How many risk factors can you identify in this case? What is the significance of relative afferent papillary defect ? What is the most likely diagnosis? Case 02- History (06.03.2015) A 65 year old man presented to the eye OPD with the complaints of sudden painless loss of vision in the left eye. He described the visual loss as seeing a black spot in his vision which spread over the entire visual field with in minutes. He didn’t have any pain or discomfort prior to his symptoms. He gave history of experiencing transient visual loss lasting for a minute or two for the past 06 months. He was a known hypertensive and had history of Myocardial Infarction and CVA. Physicals VA : (BCVA) 6/12 OD, HM OS Pupils: RAPD OS. Fundus: normal OD, see photos OS BP: 160/100 mm Hg IOP 12 OD , 14 OS Some questions What is the most likely diagnosis? Central Retinal Artery Occlusion Is it a common disorder? Fortunately, No How severe could be the visual loss? Loss of vision can be profound and permanent without immediate treatment. Irreversible retinal damage occurs after 90 minutes, but even 24 hours after symptoms begin, vision can still be partially restored Why is it considered an ophthalmic emergency? Who can be affected? Risk factors Age > 50 years Arteriosclerois Hypertension and other vascular disorders CAD and angioplasty Thromboembolic diseases Glaucoma Giant cell arteritis Retinal migraine How can it be treated? The goal of emergency treatment is to restore retinal blood flow Ocular massage Paracentesis Lowering of the IOP through medications There are no proven medical or surgical techniques for treating retinal artery occlusions Oral vasodilators, intravenous fibrinolytic agents tried with varying success. Anti VEGF, if neovascularization happens Risk modification Degenerative Disorders