* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Tuberculosis (TB)
Survey
Document related concepts
Transcript
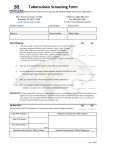
Tuberculosis (TB) PHCL 442 Lab Discussion Jamilah Al-Saidan, M.Sc Topics we will cover in TB.. • Tuberculin PPD skin test • Booster phenomenon • BCG vaccine • TB & pregnancy • TB & Lactation • TB & pediatrics Tuberculin PPD Skin Test • Also known as Mantoux method • Detects infection with M.tuberculosis & not necessary for diagnosis of active TB • PPD = Purified Protein Derivative of M.tuberculosis Tuberculin PPD Skin Test • Done by injecting 0.1 ml of 5-TU PPD intradermally into the dorsal surface of forearm • If a patient has previously been infected with M.tuberculosis sensitized T cells are recruited to the skin site where they release cytokines • These cytokines induce an induration (raised area) through vasodilatation, edema, fibrin deposition, and other inflammatory cells to the area. • Measure the diameter of the induration to interpret the results TU = Tuberculin Unit • Reaction best to be interpreted 48-72 hours. • Measure the diameter of the induration in millimeters to interpret the results PPD Skin Test PPD Skin Test Reading PPD Skin Test The person's medical risk factors determine at which increment (5 mm, 10 mm, or 15 mm) of induration the result is considered positive ≥ 5 mm ≥10 mm Recent contact to someone Patient with DM with active TB Patient with fibrotic changes on the CXR consistent with old TB Patient with CRF Organ transplant patient Patient with leukemia or lymphoma HIV patient Recent immigration <5 years from area with high prevalence of TB Immunosuppressed patient Employee of high risk settings Children < 4 years Mycobacteriology lab personnel Injection drug abusers ≥15 mm No risk factor for TB Does a Positive Test Indicate a TB Diagnosis?? • No- hence the term false-positive • To confirm diagnosis must obtain a culture • AFB (sputum smear) AFB = Acid Fast Bacilli False Positive Results • Previous administration of BCG vaccine • Cross reaction with other mycobacterial species • Qualified, experienced person must read the test BCG= Bacillus of Calmette-Guerin Does a Negative Test Eliminate a TB Diagnosis?? • No • 25% false negative results during initial evaluation of patients with active TB • False –ve results can occur in: 1. In persons who have had no prior infection with M.tuberculosis 2. Who have only recently been infected 3. Who are anergic Does a Negative Test Eliminate a TB Diagnosis?? Anergy • Decreased ability to respond to Antigens • Caused by: 1. Old age/ newborns 2. Corticosteroids 3. Immunosuppressive drugs 4. HIV infection 5. Recent viral infection 6. Malnutrition False Negative Results Factors due to the person being tested Factors due to administration Factors due to tuberculin used Factors due to reading the test Live virus vaccination SQ injection Improper storage In-experienced reader CRF Injecting too little Contamination antigen Recent TB infection (within 810 weeks of exposure) Corticosteroids & immunosuppressant agents age (less than 6 months old, elderly) Bacterial, viral or fungal infection Error in recording Booster Phenomenon • When a person experience a significant increase in the size of a tuberculin skin test reaction that may not be caused by M.tuberculosis • Could be due to: PPD skin test performed every 1-2 years Prior BCG vaccine Other mycobacteria Booster Phenomenon • Use two-step testing for initial skin testing of adults who will be retested periodically (e.g., health care workers). The incidence of this phenomenon appears to increase with age. • This ensures that any future positive tests can be interpreted as being caused by a new infection. Done for new employees. 1. Return to have first test read 48-72 hours after injection If first test is positive, consider the person infected. If first test is negative, give second test 1-3 weeks after first injection 2. Return to have second test read 48-72 hours after injection If second test is positive, consider person previously infected If second test is negative, consider person uninfected A person who is diagnosed as "infected" on two-step testing is called a "tuberculin converter". BCG Vaccine • Derived from an attenuated strain of M.bovis • Vaccine efficacy only ≤80% • More effective if given in childhood • Not recommended during pregnancy or for HIV infected individuals • Prior vaccination can cause positive PPD skin test • Side effects: prolonged ulceration at the vaccination site, lupoid reactions & death BCG: Bacillus of Calmette and Guerin Vaccine TB & Pregnancy • Untreated TB represents a greater risk to a pregnant women and her fetus than treatment • INH, rifampin, ethambutol & streptomycin have all been reported to be teratogenic in animals but no human reports • Studies have shown that INH, rifampin, & ethambutol are safe in pregnancy & can be used to treat TB and treatment should be continued for 9 months TB & Pregnancy • All pregnant women on INH should receive pyridoxine 25 mg /day to prevent CNS toxicity • Pyrazinamide have no enough data to support its use in pregnancy, only reserved for cases of drug resistance • Streptomycin is used only as a last resort due to fear of ototoxicity in infants INH = Isoniazide CNS = Central Nervous System TB & Lactation • Only minimum amounts are excreted in breast milk • Lactation is safe during anti-TB treatment TB & Pediatrics • Whenever a diagnosis is suspected start treatment due to risk of disseminated TB in children • Same drugs for adults can be used • Examine routinely for signs and symptoms of hepatitis, increase in LFT 2-3 times normal are common but benign and often transient. • Except for ethambutol not because it is more toxic but its more difficult to assess visual acuity in children TB & Pediatrics • In pediatrics three drugs are enough for treating TB • Start with INH 10 – 15 mg/kg/day + Rifampin 10 – 20 mg/kg/day + Pyrazinamide 15 – 30 mg/kg/day 2 months • Continue with INH 20-30 mg/kg/dose + Rifampin 10-20mg/kg /dose (two or three times weekly) 4 months • Use ethambutol 15 – 20 mg/kg/day or streptomycin 20 – 40 mg/kg/day in cases of resistance only