* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Brain Abscess
Survey
Document related concepts
Transcript
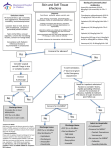
Brain Abscess What is brain abscess? Focal collection within brain parenchyma Pathogenesis? Direct 20-60% of the cases Focal abscess Hematogenous Multiple abscesses No identifiable souces in 20-40% of the cases Primary sources in direct spread and distribution of abscess Otitis media – inferior temporal lobe and cerebellum Frontal or ethmoid sinuses – frontal lobe Dental caries – frontal lobe Foreign bodies - bullet Primary sources hematogenous spread Chronic pulmonary infections – lung abscess and empyema Skin infection Intrabdominal and pelvic infection Bacterial endocarditis Cyanotic congenital heart disease – most common in children Microbiology Clues to the primary source Anaerobics Usually mouth flora May be from pelvic or intraabdominal infections – multiple abscesses Examples – anaerobic streptococci, bacteroides species, fusobacterium Aerobics Gram positive Staphylococcus aureus – neurosurgery and trauma Streptococcus milleri – proteolytic enzymes that cause necrosis Others – viriddans streptococci, microaerophilic streptocci Gram negative Usually from trauma or neurosurgery Klebsiella pneumoniae, Pseudodomonas species, E. coli, and Proteus species Immunocompromised hosts? Opportunistic infections Toxoplasma gondii Listeria Fungi – Aspergillus, cryptococcus neoformans, coccidiodidides immitis, Candida albicans Immigrants Parasites Cysticercosis – 85% of brain infection in Mexico city Symptoms? Headache – most common Neck stiffness Associated with occipital abscess Abscess leaks into lateral ventricle Altered mental status – cerebral edema Vomiting – increased intracranial pressure Physical finding? Fever – not very reliable, since only 45-50% present Focal neurological deficit – days or weeks after onset of headache Seizure 25% of the cases May be first manifestation of brain abscess Grand mal in frontal infection Third or sixth cranial palsy – increased intracranial pressure Papilledema – cerebral edema Tests? CT scan with contrast MRI with gadolinium diethylenetriamine Lumbar puncture Contraindicated Analysis WBC < 500/mm3 with predominately lymphocytes WBC > 1,000/mm3 consistent with meningitis but not improved with antibiotics, consider MRI for ruptured abscess Treatment options? Antibiotics – 6 to 8 weeks Surgical drainage Antibiotics? Penicillin G – aerobic and anaerobic streptococci from mouth flora Metronidazole – against anaerobes but not aerobes, good intralesional penetration Ceftriaxone or cefotaxime – Enterobacteraciae, particular chronic ear infection Ceftazidime – neurosurgery and p. aeruginosa Oxacillin or nafcillin – head trauma or neurosurgery, mainly staphylococcus aureus coverage Vancomycin – MRSA Aminoglycosides – poor blood brain barrier, not use Indications for surgical drainage? No clinical improvement within a week Depressed sensorium Increased intracranial pressure Progressive increase in the ring diameter of the abscess Surgical approach Needle aspiration Prefer approach because of less neurological deficit Under ultrasound or CT guided Surgical excision More neurological deficit Prefer in traumatic abscess, particularly with foreign body,and encapsulated fungal abscess Advantages: shorten antibiotics to 2 to 4 weeks and less relapse Steroid use? Mainly for mass effect Disadvantages Reduce contrast enhancement on CT scan Slow capsule formation Increase risk of rupture Decrease penetration of antibiotics Complications Neurological deficits – commonly seizure with frontal lesion Poor prognosis – mortality rate up to 30% Rapid progression of the infection Severe mental changes Rupture into ventricle