* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 23 - Bakersfield College
Malnutrition wikipedia , lookup
Hunger in the United States wikipedia , lookup
Food safety wikipedia , lookup
Obesity and the environment wikipedia , lookup
Overeaters Anonymous wikipedia , lookup
Human nutrition wikipedia , lookup
Food studies wikipedia , lookup
Food politics wikipedia , lookup
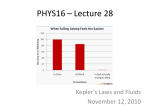
Food coloring wikipedia , lookup
Chapter 23 Nutrition and Fluids LEARNING OUTCOMES: Define the key terms and key abbreviations listed in this chapter Explain the purpose and use of the MyPyramid food guidance system Explain how to use the Dietary Guidelines for Americans Describe the functions and sources of nutrients Explain how to read and use food labels Describe the factors that affect eating and nutrition Describe the OBRA requirements for serving food Describe the special diets and between-meal nourishments Identify the signs symptoms, and precautions for aspiration Describe fluid requirements and the causes of dehydration Explain what to do when the person has special fluid orders Explain the purpose of intake and output records Identify what is counted as fluid intake Identify how to assist with food and fluid needs Explain how to assist with calorie counts Explain how to safely provide drinking water Explain how to prevent foodborne illnesses Perform the procedures described in the chapter The person’s diet affects physical and A poor diet and poor eating habits: mental well-being. •Increase the risk for infection •Increase the risk of acute and chronic diseases •Cause chronic illnesses to become worse •Cause healing problems •Affect physical and mental function, increasing the risk for accidents and injuries Culture, finances, and personal choice affect dietary practices. BASIC NUTRITION is the processes involved in the ingestion, digestion, absorption, and use of foods and fluids by the body. •Good nutrition is needed for growth, healing, and body functions. •A well-balanced diet and correct calorie intake are needed. Foods and fluids contain nutrients. •Nutrients are grouped into fats, proteins, carbohydrates, vitamins, minerals, and water. Nutrition The Dietary Guidelines for Americans 2005 are for persons 2 years of age and older. •Through diet and physical activity, the guidelines serve to: Promote health Reduce the risk of chronic diseases •The guidelines describe a healthy diet as one that: Is high in fruits, vegetables, whole grains, and fat-free or low-fat milk and milk products Includes lean meats, poultry, fish, beans, eggs, and nuts Is low in fats, cholesterol, salt (sodium), and added sugars The MyPyramid food guidance system is based on the Dietary Guidelines for Americans 2005. The MyPyramid symbol shows the “Steps to a Healthier You.” •The kind and amounts of food to eat daily Depend on the person’s age, gender, and activity level •Gradual improvement •Physical activity •Variety •Moderation •The right amount from each food group band Grains, vegetables, fruits, milk, meats and beans, and oils Nutrients •No food or food group has every essential nutrient. •Protein is the most important nutrient. It is needed for tissue growth and repair. •Carbohydrates provide energy and fiber for bowel elimination. •Fats provide energy. They add flavor to food and help the body use certain vitamins. •Vitamins are needed for certain body functions. They do not provide calories. •Minerals are used for many body processes. •Water is needed for all body processes. Food labels •Food labels are used to make informed food choices for a healthy diet. •Food labels contain information about: Serving size and the number of servings in each package Calories and calories from fat Nutrients •How a serving fits into the daily diet is called the Daily Value (DV). •The DV is expressed as a percent. The percent is based on a daily diet of 2000 calories. FACTORS AFFECTING EATING AND NUTRITION Meeting a person’s nutritional needs requires a team approach. The nutritional care plan involves: •The person’s likes and dislikes •The person’s life-long habits Age affects nutrition. Culture influences dietary practices, food choices, and food preparation. Selecting, preparing, and eating food often involve religious practices. People with limited incomes often buy the cheaper carbohydrate foods. Loss of appetite can occur from: •Illness, drugs, anxiety, pain, and depression •Unpleasant sights, thoughts, and smells Food likes and dislikes are personal. •Usually food likes expand with age and social experiences. Body reactions affect eating and nutrition. Appetite usually decreases during illness and recovery from injuries. •Nutritional needs are increased. Disease or injury can affect the hands, wrists, and arms. •Adaptive equipment lets the person eat independently. SPECIAL DIETS may order special diets: •For a nutritional deficiency or a disease •For weight control •To eliminate or decrease certain substances in the diet Regular diet, general diet, and house diet mean no dietary limits or restrictions. Many patients and residents need special diets. Doctors The sodium-controlled diet •Sodium causes the body to retain water. •Sodium control decreases the amount of sodium in the body. •The doctor orders the amount of sodium allowed. •Sodium-controlled diets involve: Omitting high-sodium foods Not adding salt to food at the table Limiting the amount of salt used in cooking Diet planning Diabetes meal planning is for people with diabetes. •The dietitian and person develop a meal plan. Consistency is key. •The meal plan involves: The person’s food preferences Calories needed Eating meals and snacks at regular times •You need to: Serve the person’s meals and snacks on time. Always check the tray to see what was eaten. Tell the nurse what the person did and did not eat. Tell the nurse about changes in the person’s eating habits. The dysphagia diet •Dysphagia means difficulty swallowing. Food thickness is changed to meet the person’s needs. •The doctor, speech-language pathologist, occupational therapist, dietitian, and nurse choose the right food thickness. •When feeding the person with dysphagia, you must: Know the signs and symptoms of dysphagia. Feed the person according to the care plan. Follow aspiration precautions. Report changes in how the person eats. Report choking, coughing, or difficulty breathing during or after meals at once. Report abnormal breathing or respiratory sounds at once. FLUID BALANCE Death can result from too much or Fluid balance is needed for health. too little water. •The amount of fluid taken in (intake) and the amount of fluid lost (output) must be equal. If fluid intake exceeds fluid output, body tissues swell with water. This is called edema. If fluid output exceeds intake, dehydration occurs. An adult needs 1500 mL of water daily to survive. •About 2000 to 2500 mL of fluid per day are needed for normal fluid balance. Common special fluid orders are: •Encourage fluids (The person drinks an increased amount of fluids.) •Restrict fluids (Fluids are limited to a certain amount.) •Nothing by mouth (NPO) (The person cannot eat or drink anything.) •Thickened liquids (All liquids are thickened, including water.) Intake and output records •The doctor or nurse may order intake and output (I&O) measurements. •I&O records are kept: To evaluate fluid balance and kidney function To help in evaluating and planning medical treatment When the person has special fluid orders •The following fluids are measured and recorded: All fluids taken by mouth Foods that melt at room temperature IV fluids and tube feedings •Output includes urine, vomitus, diarrhea, and wound drainage. •Measuring intake and output Intake and output are measured in milliliters (mL). A measuring container for fluid is called a graduate. The measuring device is held at eye level to read the amount. An I&O record is kept at the bedside. Amounts are totaled at the end of the shift. The purpose of measuring I&O and how to help are explained to the person. The urinal, commode, bedpan, or specimen pan is used for voiding. MEETING FOOD AND FLUID NEEDS following can affect appetite and ability to eat: •Weakness, illness, and confusion •Unpleasant odors, sights, and sounds •An uncomfortable position •The need for oral hygiene •The need to eliminate •Pain The Preparing for meals •To promote comfort when preparing patients and residents for meals Assist with elimination needs. Provide oral hygiene. –Make sure needed dentures are in place. Make sure eyeglasses and hearing aids are in place (if worn). Make sure incontinent persons are clean and dry. Position the person in a comfortable position. Assist the person with hand washing. Serving meal trays •You serve meal trays after preparing patients and residents for meals. •Serve trays in the order assigned by the health team. •If food is not served within 15 minutes, recheck food temperatures. When feeding the person •Serve food and fluids in the order the person prefers. •Offer fluids during the meal. •Use teaspoons to feed the person. •Let the person do as much as possible. •Always tell the visually impaired person what is on the tray. •When feeding visually impaired persons, describe what you are offering. For persons who feed themselves, describe foods and fluids and their place on the tray. Use the numbers on a clock to explain the location of foods. •Allow time and privacy for prayer. •Engage the person in pleasant conversation. •Allow time for chewing and swallowing. •Sit facing the person. •Wipe the person’s hands, face, and mouth as needed during the meal. Between-meal nourishments •These nourishments are served upon arrival on the nursing unit. •Follow the same considerations and procedures as for serving meal trays and feeding persons. Calorie counts •On a flow sheet, note what the person ate and how much. •A nurse or dietitian converts the portions into calories. Providing drinking water •Patients and residents need fresh drinking water each shift and whenever the pitcher is empty. •Follow the agency’s procedure for providing fresh drinking water. FOODBORNE ILLNESSES A foodborne illness (food poisoning) is caused by pathogens in food and fluids. Signs and symptoms depend on the pathogen. Food is not sterile. •Pathogens are present when food is purchased. •Foods can become contaminated from other foods. •Food handlers with poor hygiene can contaminate the food. •Pathogens grow rapidly between 40 and 140 F. This range is called the “danger zone” by the USDA. To keep food safe, the USDA recommends these 4 safety tips: •Clean. Wash hands, utensils, and counter tops often. •Separate. Avoid cross-contamination. •Cook. Cook food to a safe internal temperature. When re-heating cooked food, re-heat to 165 F. •Chill. Refrigerate or freeze food within 2 hours. If the air is 90 F or above, chill food within 1 hour.