* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Gathered: May 18, 2010 at 2:00pm Source: Patient Reliability: 90% I
Dental emergency wikipedia , lookup
Prenatal nutrition wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Prenatal development wikipedia , lookup
Medical ethics wikipedia , lookup
Maternal physiological changes in pregnancy wikipedia , lookup
Prenatal testing wikipedia , lookup
Adherence (medicine) wikipedia , lookup
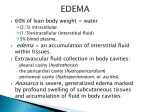
Patient safety wikipedia , lookup
Gathered: May 18, 2010 at 2:00pm Source: Patient Reliability: 90% I. PATIENT’S PROFILE A. General Data G.G, 33 y.o., G2P0(0100), 35 wks and 4/7 days AOG , Filipino, Roman Catholic,an office clerk, born on February 4, 1977 in Mati, Davao oriental, presently residing in B. Rodriguez, Cebu City, was admitted for the first time on May 14, 2010 at Cebu Doctors’ University Hospital. B. Menstrual History Menarche was at 17 y.o. with flow lasting for 5 days consuming 2-3 fully soaked pads per day. Subsequent menses occurred at in irregular interval of mostly two months with flow lasting for 5 days consuming 2-3 pads/day. Associated sign and symptom is breast tenderness. No dysmenorrheal, no intermenstrual bleeding noted. LMP was on September 9, 2009 and PMP was on July 10, 2009. C. Obstetric History OB score of G2P0(0100) Previous Pregnancies: G1 – April 20090, 32 weeks AOG, IUFD, D/C done in Maternity Hospital Present Pregnancy: LMP = September 9, 2009 EDC = June 16, 2010 AOG = 35 weeks and 4/7 days D. Prenatal History Patient’s first prenatal check up was done on December 23, 2009 at 15 weeks AOG at CDUH OPD. Vital signs were normal. The following laboratory tests were requested: CBC and FBS = normal, Urinalysis = (+) protein. She also has papsmear on her first prenatal which showed positive for N. gonorrheae. Patient took cefuroxime 500mg, 3x/day for 1 week at 24 weeks AOG and was resolved as claimed by the patient. Subsequent prenatal check up was done regularly, every 4 weeks until 32 weeks AOG and every 2 weeks until 35 weeks AOG. TT3 was given on March 2010. Patient took vitamins, Beniforte OD and Caltrate plus for calcium supplement. Quickening was observed on 16 weeks AOG. Present weight of 119 lbs with a weight gain of 20 lbs. Usual BP ranges 100/70 mmHg – 120/70 mmHg. Last prenatal check up was done on May 7, 2010. E. Contraceptive History Patient has no history contraceptive use. F. Sexual History Patient’s first coitus at the age of 31 years old with her husband as her only sexual partner. Coitus done regularly, satisfied, no dyspareunia noted. G. Past Medical History Childhood illnesses: (+) chickenpox and measles Immunizations: BCG, DPT, OPV, Hep B with booster with unrecalled dates -was given TT1 and TT2 during her first pregnancy. Hospitalization: in Maternity Hospital for her first pregnancy, IUFD, D/C was done on April 2009 Serious Illnesses : Preeclampsia on her first pregnancy and was resolved after taking Dopamet OD for 1 week. - Gonorrhea but was resoled as claimed by the patient after taking medication. H. Personal and Social History Patient is a college graduate and work as an office clerk. She had no allergies on food, drugs and dusts. No history of using prohibited drugs, non smoker and do not drink alcoholic beverages. She’s married for 3 years. Husband is 34 y.o and a driver and is apparently well as claimed by the patient. I. Family History Father: 66 years old, hypertensive Mother: 55 years old, apparently healthy Birthrank: 3rd / 5 children, all siblings are alive and healthy Heredofamilial diseases: Hypertension, no History of twinning, difficulty of delivery and congenital anomaly II. CHIEF COMPLAINT EDEMA III. HISTORY OF PRESENT ILLNESS Patient’s condition started 10 days PTA when patient noticed a non pitting edema on her feet. No pain felt. No fever, no dizziness but decrease urine output inspite increase fluid intake. No consultation done. 8 days PTA, during her prenatal check up, edema persisted and extended to her lower legs. Vital signs were normal. Patient was told by her OB that it was normal and was advised to elevate legs at home and while sleeping. Edema reduces upon waking up but recurs every afternoon and during activities. No medications taken. Few hours PTA, patient claimed that edema went up to her thighs thus decided to sought consultation in the ER. During PE, BP was noted to be elevated, fluctuating from 160/90 mmHg to 160/100 mmHg to 170/90 mmHg. Patient was advised for admission for close monitoring on her edema and BP. IV. REVIEW of SYSTEMS Weight gain of 20 lbs. Bilateral non-pitting edema on lower extremities oliguria Slight breast tenderness Striae gravidarum on abdomen and linea nigra V. PHYSICAL EXAMINATION General Survey: Patient is alert, coherent, oriented to time, date, place and person, not in distress, maintained eye contact, well-groomed. Vital Signs: BP: 120/70 mmHg, right arm, high fowlers TEMP: 38.8, left axilla PR: 90 bpm, regular rhythm, right radial pulse RR: 19 breaths/min, regular rhythm, high fowlers HT: 4’9” WT: 119 lbs BMI: Skin: warm, smooth, good mobility and turgor HEENT: Head: no lumps, symmetrical, no pain or tenderness Face: (+)facial edema, (+) periorbital edema, no lesion Eyes: visual acuity of 150/20 both eyes, anicteric sclera, (+) direct and consensual light reflex, (+) ROR, no blurring of vision, intact visual fields and EOM Ears: no pain on external ear, no hearing loss, no discharges, no tinnitus Nose: no tenderness of sinuses, no septal deviation Mouth and Throat: pinkish oral mucosa, no soreness, no ulcers, no sore throat, no tonsillitis, no gum bleeding, no pigmentation Neck: no enlarged lymph nodes, trachea midline, no goiter Breast and Axilla: no lumps, no nipple discharges, slight tenderness Chest and Lungs: equal chest expansions, no adventitious breath sounds, not tachypneic, equal tactile fremitus Heart: no murmur, no splitting of heart sounds Abdomen: protuberant, no mass, (+) striae gravidarum, (+) linea nigra, normoactive bowel sounds Palpation: Fundal height = not done Leopold’s Maneuver = not done Uterine contraction = not done Ausculation: normoactive bowel sounds Featal Heart Tone = not done Female Genitalia: positive pain Back and Extremities: (+) non-pitting edema on lower extremities, no muscle and joint pain Neurologic: intact cranial nerves, no loss of sensation, no muscle weakness, +4 muscle strength, good rapid alternating movements Rectal Examination: not assessed VI. DIAGNOSIS 1. Mild Preeclampsia Rule in = BP fluctuating from 160/90 to 160/100 to 170/90 mmHg at 35 wks 4/7 days AOG. (DBP : <100mmHg.) = Proteinuria = (+) = Oliguria = Edema 2. Pregnancy Uterine, 35 wks 4/7 days AOG, cephalic presentation, not in labor, delivered a premature baby girl by NVSD (induced). VII. DIFFERENTIAL DIAGNOSIS: 1. Severe Preeclampsia Rule in = oliguria Rule out = DBP not > 110 mmHG = proteinuria = not (++) 2. Gestational Hypertension Rule in = mild hypertension Rule out = no proteinuria 3. Chronic Hypertension Rule in = mild to severe hypertension Rule out = Chronic HPN occur <20 wks AOG or before pregnancy = no proteinuria 4. Eclampsia Rule in = Hypertension, Proteinuria, Edema Rule out = No seizure