* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download POST-TEST I
Survey
Document related concepts
Transcript
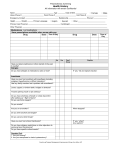
1 NUR 1021 CLINICAL FOCUSES – WEEK 2 CLINICAL PREP: (This top section should be completed prior to your first clinical day.) 1. Download Clinical Homework Forms from Canvas. 2. Get patient assignment. 3. Complete Patient Data form and Trending Sheet. Complete timeline for day one. (Day two will need to be completed for Friday morning.) 4. Complete a Medical or Surgical Diagnosis sheet for this patient’s primary diagnosis. 5. Complete a Secondary Diagnosis sheet for other patient diagnoses for which the patient is receiving medications. 6. Begin Assessment Booklet (if applicable). 7. Bring all of the above, your clinical packet, and the Gulanick Nursing Care Plans book to clinical each week. ___________________________________________________________________________________ CLINICAL FOCUSES: Surgical Nursing 1. Discuss and/or demonstrate preparing a client for surgery, including physical and emotional preparation. 2. Identify nursing interventions used to promote patient safety in the operating room. 3. Identify type of anesthetic agent and other medications used during the surgical procedure and effect on the patient. 4. Observe care given to patients in the PACU and discuss rationale for nursing interventions carried out; identify discharge criteria. 5. Plan and implement care for a postoperative patient to prevent major complications such as atelectasis, deep vein thrombosis (DVT), and wound infection. 6. Implement dependent and independent nursing interventions for a postoperative patient to relieve nausea, vomiting, pain, and constipation. Nutrition: 1. Correctly assist patients to select foods for clear liquid, full liquid, soft, or regular diets. 2. Discuss nutritional needs of the medical-surgical patient. Medications 1. Administer medications as assigned, with assistance of instructor. 2. Identify your patient’s allergies and where to POST-CONFERENCE TOPICS Review nursing process (concept map) with students using their major diagnosis form as a guide. Discuss “Care of Postoperative Patient Receiving Anesthesia” (handout). Discuss “Surgery Post-Conference” (handout). Review the rationale for the therapeutic diets the patients are receiving for their current medical/surgical condition Review procedure for passing medications on specific hospital unit Review medication sheet example and directions for administration of medications (handout) Review dosage problems that involve reconstitution Review the lab values on assigned patients and correlate alterations with rationale related to the patient’s health stressors OVER 2 locate on your patient’s record. Mixing Powders: 1. Discuss how to reconstitute powders. 2. Complete dosage problems that involve reconstitution of powders. Lab Values: 1. Identify the significance and causes of abnormal vital signs & lab values ___________________________________________________________________________________ HOMEWORK (due the Monday of Week 3 by 0950) 1. 2. 3. 4. 5. 6. 7. 8. Journal per “Clinical Journal Guidelines”. Skill’s List – updated. Patient Data Form and Trending sheet completed on this patient. Medical or Surgical Diagnosis sheet(s) completed on this patient. Secondary Diagnoses sheet completed on this patient. Assessment Booklet completed on this patient (if applicable). Care plan or concept map (if applicable). Students completing surgical and other observations for this week: - Objectives for each day - Journal per “Clinical Journal Guidelines” - Article summary with attached article 3 NUR 1021 What should students know about meds they are administering? EXAMPLE GENERIC NAME: BRAND NAME(S): GALANTAMINE – ORAL (ga-LAN-tuh-meen) (They should know the generic name) Razadyne, Reminyl PRECAUTIONS: Tell your doctor your medical history, especially of: heart problems (e.g., bradycardia, AV block, arrhythmia), stomach/intestinal problems (peptic ulcer disease, GERD), difficulty urinating, convulsions, lung disease (severe asthma, obstructive pulmonary disease), liver or kidney disease, recent tobacco use, recent/frequent alcohol use, any allergies (including allergy to daffodil plants). This drug may make you dizzy; use caution when performing activities that require alertness such as driving or using machinery. Limit alcoholic beverages because it may cause dizziness and make your stomach more likely to bleed. Caution is advised when using this drug in the elderly, as they may be more sensitive to drug side effects. Galantamine should be used only when clearly needed during pregnancy. Discuss the risks and benefits with your doctor. It is not known if this drug passes into breast milk. Breast-feeding is not recommended while using galantamine. DRUG INTERACTIONS: Tell your doctor of all prescription and nonprescription medication you may use, especially: anticholinergic drugs (e.g., benztropine, scopolamine), cholinergic drugs (e.g., bethanechol), other cholinesterase inhibitors (e.g., donepezil), succinylcholine-type muscle blocking drugs, aspirin, NSAIDS (e.g., ibuprofen, naproxen). Also report use of heart drugs (those which decrease heart rate or block AV impulse conduction) such as: digoxin, beta-blockers (e.g., metoprolol, propranolol), calcium channel blockers (e.g., diltiazem, verapamil). Do not start or stop any medicine without doctor or pharmacist approval. ACTION: Q: How does galantamine work? A: It is a competitive inhibitor of acetylcholinesterase. Q: What is acetylcholinesterase? A: It is the enzyme that is responsible for the breakdown of acetylcholine. Q: Why do we care? (Also phrased, What does acetylcholine do?) A: Acetylcholine—part of the cholinergic system—helps memory, attention, and modulates (regulates) excitatory impulses. So. . . , if we have more acetylcholine, it can help with transmission of impulses for memory, attention, and response to stimuli. And. . . , by taking an acetylcholinesterase inhibitor, we can keep more acetylcholine in our brain. 4 REVISITING DRUG INTERACTIONS: Q: Why are anticholinergic drugs listed in drug interactions (previous page)? A: Anticholinergics and galantamine work against each other. Q: Why are cholinergic drugs listed in drug interactions (previous page)? A: Too much of a good thing. Q: Why are beta blockers listed in drug interactions (previous page)? A: We don’t want to give something (galantamine) that could speed the heart when the other med is trying to slow the heart. ADDITIONAL QUESTIONS: 1. Are we giving a safe dose? 2. Why is this patient on this drug? 3. Is the patient allergic to this drug? 4. How will you evaluate effectiveness of this drug? 5 DIRECTIONS FOR PREPARATION IN GIVING MEDICATIONS A. Preclinical Preparation 1. 2. 3. 4. 5. B. List all medications (dosage, time, and route) to be given to assigned patient. Check med sheet against the doctor's order sheet to see that all drugs were correctly ordered and still current. Bring your drug book for reference. If drugs are not in your book, you must use the PDR, Lexicomp or other acceptable reference. Bring med sheets to clinical (from Assessment Booklet). If you are giving a med, you must have looked it up prior to clinical! Clinical Day 1. 2. 3. 4. 5. 6. 7. 8. 9. Bring your drug book for reference. Be able to state why the patient is on this drug, action, dose, and nursing considerations for all drugs. Before pre-conference, again check med sheet or MAR against doctor's order sheet for new or cancelled orders. Assess patient as necessary (example: BP, apical pulse) before instructor is present to check meds. Get fresh water, straw, anything else needed to give meds. Review the patient allergies for any possible contraindications. Have hands washed before instructor gets there. Students must accept responsibility to give medications within accepted time allowance. It may be necessary for student to seek out instructor to supervise medication administration. Do not use nursing staff as preceptor for assisting with medications administration. You never give a med until your instructor has “checked your meds” with you. See sample Medication List for information to come prepared with (over). Often it is helpful to make condensed “focus” note cards on medication information that organizes the major points about the medications you are administering. 6 NUR 1021 –Post-Conference Care of Postoperative Patient Receiving Anesthesia 1. Describe type of anesthetic administered to patient: 2. List side effects of anesthetic(s): a. Major SE: B. Common SE: 3. Describe how anesthetic can impact your patient’s recovery (i.e., effect on major organ systems such as lungs, kidneys, liver, etc.): 4. What are some potential complications that can occur in patients receiving general anesthesia? 5. How would you prevent these complications? 6. What are potential complications associated with epidural or spinal anesthetics? 7. List nursing measures to take when working with a patient after: 8. a. General anesthesia b. Epidural anesthesia c. Spinal anesthesia d. Local anesthesia List other medications patient received during surgery related to anesthesia. Drug Classification Action Side Effects 7 SURGERY POST-CONFERENCE List how surgery affects different body systems based on: Categories of Human Functioning and Nursing Interventions to Prevent Potential Complications. Categories of Human Functioning Comfort and Rest (Sleep/Rest/Pain/Comfort) Sensory Perceptual Function (Neurological) Fluid Gas Transport Function (Cardiovascular) Fluid Gas Transport Function (Respiratory) Elimination Function (Gastrointestinal) Elimination Function (Genitourinary) Nutrition Function (Nutrition/Metabolic) Protective Function (Hygiene, Skin, Integumentary) Activity/Mobility/Movement Fnct. (Musculoskeletal) Growth and Development Fnct. (Male or Female) Psycho/Social/Cultural/Spiritual Function (Role Relationships, Psycho-Social Behavior, Values/Beliefs/Spiritual) Protective Function (Education/Discharge Planning) NUR 1021 Spring 2016 Effects of Surgery and Potential Complications Nursing Interventions to Prevent Potential Complications