* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES
Survey
Document related concepts
Transcript
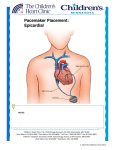
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES BANGALORE, KARNATAKA PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION 1. Name of the candidate and address : Praveena Justy Mathew I Year M.Sc. Nursing Mallige Institute of Nursing Sector-II, HMT Post, Bangalore-13 2. Name of the Institution : Mallige Institute of Nursing Sector-II, HMT Post, Bangalore-13 3. Course of Study and Subject : I Year M.Sc. Nursing Medical Surgical Nursing 4. Date of Admission to Course : 28.11.2011 5. Title of the Topic : “A study to evaluate the effectiveness of Self Instructional Module (SIM) on knowledge regarding cardiac pacemakers among final year B.Sc. nursing students at selected Nursing Colleges, Bangalore”. 1 6. BRIEF RESUME OF THE INTENDED STUDY 6.1. NEED FOR THE STUDY Heart rate (pulse) is a sign of life. The goal of life is to make your heartbeat match the beat of the universe, to match your nature with Nature. Joseph Campbell Life is about rhythm. We vibrate, our hearts are pumping blood, we are a rhythm machine, that's what we are. Mickey Hart The heart beats rhythmically, thanks to the existence of a special "engine": the sinus node, called "the natural pacemaker". The cells of the sinus node are able to generate a spontaneous regular action potential and thereby modulate heart rate. The heart has its own built-in electrical system, called the conduction system. Our heart has its own internal electrical system that controls the rate and rhythm of our heartbeat. With each heartbeat, an electrical signal spreads from the top of the heart to the bottom. As the signal travels, it causes the heart to contract and pump blood. Each electrical signal normally begins in a group of cells called the sinus node or sinoatrial (SA) node.1 Normally, the heart beats in a regular and coordinated way like a clock or metronome. However, many people with heart failure may have a heart that beats irregularly and/or too fast or too slow. These rhythm problems are often referred to as arrhythmias or dysrhythmias. They are often benign, which means these rhythm problems do not cause any deviation and are not related to any known abnormality of the heart. But arrhythmias may also be due to changes in the heart from either heart failure or a previous condition such as a heart attack or long-standing high blood pressure. Under these circumstances arrhythmias may be dangerous and are important to understand and treat. With proper treatment and self-care, people with heart failure can lead normal, active lives even if they also have a heart rhythm problem.1 The cardiovascular crisis in India has quadrupled in the last 40 years and WHO estimates that by 2020 close to 60% of cardiac patients worldwide will be Indian. The established risk factors of cardiovascular disease include lack of exercise, poor diet, and smoking. According to the study the Indian subcontinent (including India, Pakistan, Bangladesh, Sri Lanka, and Nepal) has the highest rates of cardiovascular disease (CVD) globally. The emerging field of environmental cardiology addresses exposures to chemicals and other environmental substances also have profound impact on heart health.2 Technology has helped the health lives of thousands of people around the world. All of these health findings are used to detect the diseases and help patients to cope with health problems. One of the technological health inventions is artificial pacemaker, invented by a Canadian John Hopps in 1950 and it was used for the first time in human body in 1958 after several modifications.3 Artificial pacemaker is an electrical device which delivers a small stimulant shock to the heart to effect cardiac contraction at a pre-determined rate. Many of today's pacemakers have two main components: the electrodes and the transducer (pulse generator). The electrodes are wires which are placed into the circulatory 2 system and make physical contact with the heart muscle. A small electrical discharge from the pacemaker electrode stimulates the muscular wall of the heart to contract, thus pumping blood in an organized fashion. The transducer is a small device, usually implanted under the skin, that generates the electrical discharge at a pre-determined frequency. Transducers can monitor the heart rate of contraction and deliver an electrical shock only when the heart is going too slow.4 There are several types of pacemakers. This can be permanent or temporary. Temporary pacing can be used in emergent or elective situation that require limited, short-time pacing(less than 1 week). Permanent pacing is indicated for chronic or recurrent dysrhythmias that are severe, unresponsive to antidysrhythmic medication and caused by AV block or SA node malfunction. Pacemakers can be implanted in the body, including single-chamber pacemakers, dual-chamber pacemakers, rate-responsive pacemakers, and demand pacemakers.5 A world-wide survey of cardiac pacing and implantable cardioverter-defibrillator (ICD) practices is held each 4 years. Survey was undertaken for calendar year 2009 and compared to a similar survey conducted in 2005. There were contributions from 61 countries: 25 from Europe, 20 from the Asia Pacific region, 7 from the Middle East and Africa, and 9 from the Americas. The 2009 survey involved 1,002,664 pacemakers, with 737,840 new implants and 264,824 replacements. The United States of America (USA) had the largest number of cardiac pacemaker implants (225,567) and Germany the highest new implants per million population (927). Virtually all countries showed increases in implant numbers over the 4 years between surveys.6 A survey reported that about 600,000 pacemakers are implanted each year worldwide and the total number of people with various types of implanted pacemaker has already crossed 3 million. There is a massive demand for pacemakers in the country. According to a recently published data, approximately 20,000 pacemaker implants take place annually. The most cost effective locations that offer up to almost 80% savings in comparison to the US are India, Thailand, Malaysia, Singapore, and Turkey.7 According to the St Jude company for the year 2008 and 2009 around 21 pacemaker implantation done in the entire state of Karnataka and this number is increasing further. Over the past few decades, cardiac pacemakers have become quite advanced, quite safe, and quite effective, and the people who receive them generally can lead entirely unrestricted lives. Today's pacemakers are truly remarkable devices. Pacemakers are necessary because, while there are many medications that prevent the heart from going too fast, there are only handfuls that make it go faster. Those that speed the heart rate are poorly tolerated and very often associated with serious side effects.8 A study was conducted on Preoperative assessment of patient with implanted cardiac pacemakers and defibrillators there are more than 400,000 patients with pacemakers or implantable cardioverter defibrillators in Japan, and more patients undergoing surgery will have an implanted cardiac device. In these patients, preoperative evaluation of the indication for the implant, such as arrhythmias and ischemic heart disease, should be performed based on guideline. It is also important to determine whether a patient is pacemaker 3 dependent, the type of device, and the programmed settings. In addition, many potential adverse interactions between electrical/magnetic activity and cardiac device function that may occur during the operative period should be assessed before surgery.9 A study was conducted about the COMPANION (Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure) in which 1500 patients took part. They were randomly assigned to one of three groups.20% of the patients were given medications alone, and other 40% of patients received medications plus an implantable bi-ventricular pacemaker. A third group (40%) received medications plus an implantable device, called a resynchronization pacemaker plus defibrillator. This study concluded that the pacemaker, whether alone or combined with a defibrillator, probably played a role in reducing hospitalizations, because it can relieve the symptoms of heart failure, such as congestion in the lungs. “The patient feels better and therefore is less likely to require treatment in a hospital.”10 A study was conducted on Change in quality of life in patients with permanent cardiac pacemakers the 42 subjects had moderate QOL (62.4 +/- 15.9 on a scale of 97) before pacemaker implantation and the QOL improved significantly after pacemaker implantation(p <.05). The QOL improvement reached a peak at the end of the fourth month and the scores decreased at the end of the sixth month vs. the fourth month (p <.05). They had significant improvement in general well-being, sleeping, appetite, physical activity, and physical symptoms (p <.05), but not in cognitive function, social participation, work capability and sexual function (p >.05). Subjects with spouses as their main caregivers had significantly better improvement in QOL after pacemaker implantation.11 A study was conducted on wound management and restrictive arm movement following cardiac device implantation. Recent guidelines on wound management published by The National Institute for Health and Clinical Excellence (NICE) in the UK recommend covering the wound postoperatively for 48 h with a lowadherent transparent dressing and letting patients shower thereafter. Since specific guidelines for cardiac device patients are lacking, we suggest that further research address whether or not the NICE guidelines can be extrapolated to this area. Studies showed that early mobilization and allowing a full range of arm movements following device implantation is safe. Further research must validate this findings.12 A prospective multicenter cohort study (the FOLLOWPACE study) was conducted among 1517 patients receiving a PM between January 2003 and November 2007. It was found that the complication incidence in modern pacing therapy is still substantial. Most complications occur early after PM implantation. Although various patient- and procedure-related characteristics are independent predictors for early and late complications, their ability to identify the patient at high risk is rather poor. This relatively high incidence of PM complications and their poor prediction underscores the usefulness of current guidelines for regular follow-up of patients with PM.13 Overall morbidity and mortality depend on the underlying cause of malfunction as well as the patient's dependency on the pacemaker. Most pacing system malfunctions are benign, although conditions such as cross-talk inhibition or runaway pacemaker can be life threatening. Maisel reported 1 in 75,000 death rate among pacer implants.14 4 A prospective study conducted to evaluate the patients with high incidence of cardiac device infection (CDIs) (45.4%). The rate of infections has ranged from 0.8 to 5.7%. The main cause of infections has been recently demonstrated to be local contamination during implantation. It is mentioned that skin contamination at the time of surgery can lead to subsequent PI. The most common symptoms in patients with pacemaker endocarditis are fever (84 to 100%) and chill (75 to 84%). Clinical evidence of CDI is defined as erythema, warmth, fluctuance, wound dehiscence, erosion, or tenderness at the generator site. Nursing personnel is present during all stages of pacemaker implantation and is therefore an important member of the multidisciplinary team involved in the procedure. The nurse’s various roles make apparent the need for a high quality of knowledge and skills, concerning all aspects of general nursing principles, along with details of this specialized cardiac procedure.15 A cross-sectional descriptive study was performed on nurses, to examine their performance in giving care to patients with temporary and permanent pacemakers. Data was collected by a researcher-made questionnaire with 36 questions on nursing care (15 items on hospital care and 21items on discharge time nursing care). The study concluded that, nurses’ lack of information on patient education and the critical situation suggest, establishing nursing re-education courses and adding courses with functional content to nursing curriculum.16 In the light of above facts and evidences, there are fewer studies done on nursing knowledge and hardly any studies on nursing students. Among the studies conducted on nurse’s knowledge shows a wide gap in the knowledge and skills in taking care of client with cardiac pacemakers. As it is the advanced technology, the nurse must be competent enough to render their care in a highly sophisticated way. In which teaching students is a better option, where in the student could be trained and equipped with necessary knowledge. Hence, This study is directed towards providing Self Instructional Module on cardiac pacemakers and to measure the efficacy of the same, so as to provide better client care, which in turn will reduce the incidence of cardiac pacemakers failure in hospitals and in community there by helping in increasing the quality of life in patient. 5 6.2. REVIEW OF LITERATURE A literature review discusses published information in a particular subject area, and sometimes information in a particular subject area within a certain time period. A world-wide survey of cardiac pacing and implantable cardioverter-defibrillator (ICD) was undertaken for calendar year 2009 .There were contributions from 61 countries: 25 from Europe, 20 from the Asia Pacific region, 7 from the Middle East and Africa, and 9 from the Americas. The 2009 survey involved 1,002,664 pacemakers, with 737,840 new implants and 264,824 replacements. The United States of America (USA) had the largest number of cardiac pacemaker implants (225,567) and Germany the highest new implants per million populations (927) .A recent report said that 60% of the world’s heart patients will be in India. Patients with severe heart arrhythmias are at risk of dying within months without the aid of a pacemaker. Approximately 20,000 pacemaker implants take place annually. India, Thailand, Malaysia, Singapore, and Turkey are the most cost effective locations that offer up to almost 80% savings in comparison to the US. Health care centers of Goa, Delhi and Kerala provide most modern equipments available for Pacemaker in India.6 A study was conducted to evaluate the risk of pacemakers causing unintended cardiac stimulation following exposure to a simulated MRI magnetic field. Researchers found that when exposed to the strong, "gradient," magnetic field, the pacemaker could deliver a drastically altered pulse and stimulate the heart inappropriately."MRI systems emit several types of extremely intense magnetic fields which causes injury to patients due to interactions with pacemakers," "Cardiologists who choose to scan patients with cardiac pacemakers must assess the risks versus the benefits of the scan."17 A study conducted to evaluate the complications related to permanent endocardial pacing in the era of modern pacemaker therapy. 446 patients, who received permanent endocardial pacemakers, were reviewed retrospectively using patient records. Attention was paid to the occurrence of any complication during the implantation or follow-up. An early complication was detected in 6.7%, and 4.9% of patients were treated invasively due to the early complication. Late complication developed in 7.2% and reoperation was required in 6.3% of the patients. Complications related to the implantation procedure occurred in 3.1%. Inadequate capture or sensing was observed in 7.4% of the patients. Pacemaker infection was detected in 1.8% and erosion in 0.9% of the patients. An AV block developed in 3.6% (1.6%/year) patients who received an AAI(R)-pacemaker due to sick sinus syndrome. There was no mortality attributable to pacemaker therapy. A great majority (68%) of the complications occurred within the first 3 months after the implantation. Complications associated to modern permanent endocardial pacemaker therapy are not infrequent. 11% of patients needed an invasive procedure due to an early or late complication.18 A study was conducted to evaluate the effects of cardiac resynchronization therapy (CRT) in heart failure patients with narrow QRS complex (<120 ms) and evidence of left ventricular (LV) dyssynchrony on tissue Doppler imaging (TDI). Cardiac resynchronization therapy is beneficial in selected heart failure patients with wide QRS complex (≥120 ms). Patients with narrow QRS complex are currently not eligible for CRT, and the 6 potential effects of CRT are not well studied. 33 consecutive patients with narrow QRS complex and 33 consecutive patients with wide QRS complex (control group) were prospectively included Cardiac resynchronization therapy appears to be beneficial in patients with narrow QRS complex and severe LV dyssynchrony on TDI, with similar improvement in symptoms and comparable LV reverse remodeling to patients with wide QRS complex.19 A retrospective study of 459 consecutive patients on chronic warfarin therapy who underwent device surgery from April 2004 to September 2008. Warfarin was continued in 222 patients during the perioperative period. Warfarin was temporarily held and bridging therapy administered in 123 patients. Warfarin was temporarily held without bridging therapy in 114 patients. There were three groups. Patients who continued taking warfarin had a lower incidence of pocket and a shorter hospital stay than did patients in the bridging group. Holding warfarin without bridging is associated with a higher incidence of transient ischemic attacks. Temporarily interrupting anticoagulation is associated with increased thromboembolic events, whereas cessation of warfarin with bridging anticoagulation is associated with a higher rate of pocket hematoma and a longer hospital stay. Continuing warfarin with a therapeutic international normalized ratio appears to be a safe and cost-effective approach when implanting a pacemaker or defibrillator in patients with moderate to high thromboembolic risk.20 A study was performed to test the protection offered by electromagnetic filters of cardiac pacemakers against cellular phone ringing. Researchers performed 330 consecutive tests in 158 patients at the time of routine examination in our pacemaker follow-up clinic. The programmed parameters remained unchanged before testing. During electrocardiographic monitoring, 2 single-band digital cellular phones consecutively placed over the pacemaker pocket each received a call. The phone systems tested were 1) GSM at a maximal power output of 2 W, operating on a 900 MHz carrier frequency, and 2) PCS at a maximal output of 1 W, operating on a 1800 MHz carrier frequency .Interference was noted in only 5 tests, due to interaction by the GSM system with 4 unprotected pacemaker models. The GSM test was negative in 12 other tests of identical pulse generator models. The overall incidence of interference was 1.5% of tests. Interference by cellular phone ringing occurred only with unprotected pacemaker models. Standard programming of these unprotected models was associated with a low incidence of interference.21 A descriptive cross sectional survey was carried out on consecutive patients at the pacemaker clinic. A 47-question tool was developed and tested. Patients' perceptions of safety of performing various routine activities, along with socio demographic data were recorded. The final sample included 93 adult patients (45% males). 41% were illiterate. 77.4% recalled receiving counselling at implantation. A considerable proportion of patients considered many routine activities unsafe including driving automobiles (28%), passing through metal detectors (31%), bending over (37%), and sleeping on the side of the pacemaker (30%). Also considered unsafe were operation of household appliances- TV/VCR (television/video cassette recorders) (53%), irons (55%)) and electrical wall switches (56%).For nearly all variables neither literacy nor history of counselling improved incorrect perceptions. This study shows that the pacemaker patients perceive many 7 routine activities as unsafe, potentially leading to disabling life style modifications. The tremendous investment in pacemaker technology to improve patient performance is not going to pay dividends if patients continue to remain disabled due to incorrect perceptions. Further studies are required to determine the reasons for these misperceptions, and to determine if these problems also exist in, and hinder, other patient populations.22 A study conducted to compare the heart's energy use during pacing and the energy use during dobutamine use. Left bundle branch block (LBBB) patients with DCM were studied. All measurements were done in a cath lab. Catheters were used to take the measurements, which included the heart's "squeezing" strength, pulse pressure, heart output, pressure to size relationships, and oxygen use. The patients were studied using LV (left ventricular) pacing, BV (biventricular) pacing, and IV dobutamine separately. This study suggests that pacing "stresses" the heart less than IV dobutamine, so pacing's long-term effects may be milder Pacing makes the heart's chambers beat as a team again.23 A recent 4 randomized controlled studies that compared rhythm control versus rate control therapy demonstrated that rate control therapy is an acceptable alternative to rhythm control therapy. The control of heart rate achievable with pharmacologic therapy is imperfect and, in many patients, difficult to obtain. Pacing therapy offers better control of heart rate than drug therapy. The aim of the PAF 2 trial was to evaluate the effect of antiarrhythmic drug therapy on long-term maintenance of normal sinus rhythm after ablation and pacing therapy and to evaluate the effect of maintenance of normal sinus rhythm. In this multicenter randomized controlled trial, 68 patients with severely symptomatic paroxysmal atrial fibrillation were assigned, after successful atrioventricular junction ablation and pacing treatment, to antiarrhythmic drug therapy with amiodarone, propafenone, flecainide or sotalol and were compared with 69 patients assigned, after successful AV junction ablation and pacing treatment, to no antiarrhythmic drug therapy. Although patients in the antiarrhythmic drug arm had a reduction in the risk of developing chronic atrial fibrillation, there was no clinical benefit beyond that obtained with ablation and pacing alone. On the contrary, antiarrhythmic therapy was associated with more serious adverse clinical events, i.e. episodes of heart failure and hospitalization. This suggests that the control of ventricular rhythm by ablation and pacing has a greater beneficial effect on short-term clinical outcome than the preservation of atrial contraction. Therefore, the results of PAF2 study are consistent with the drug trials comparing rhythm and rate control.24 A study was conducted on Care and safety of pacemaker electrodes in intensive care and telemetry nursing units. Responses were received from 476 units representing 388 (43%) of the 895 institutions. Most respondents reported using gloves, although few hospitals had policies mandating this practice. The insulating materials used most often, in order, were a glove or finger cot, tape, and gauze. Few units (25%) use any measure to reduce static electricity generated by movement over carpeting. Little attention was paid to insulating exposed epicardial temporary pacing electrodes at the generator.25 A study was conducted on multiprogrammable pacemakers, Complications and Nursing care. The study of 927 patients of both sexes, with multiprogramable pacemakers, at the "Comandante Manuel Fajardo" 8 Teaching Hospital and the Institute of Cardiology and Cardiovascular Surgery. Complications accounted for 14.9% and the most frequent were, in decreasing order, as follows: sepsis of the pocket (46.7%), hematoma of the pocket, increased threshold and, in a lower percentage, aseptic necrosis (5.7%). Emphasis is made in the role of the nurse in front of a patient with pacemaker and of the different complications presented.26 A cross-sectional descriptive study was performed on nurses, to examine their performance in giving care to patients with temporary and permanent pacemakers. Data was collected by a researcher-made questionnaire with 36 questions on nursing care (15 items on hospital care and 21items on discharge time nursing care). The study conclude that, considering nurses’ lack of information on patient education and the critical situation suggest establishing nursing re-education courses and adding courses with functional content to nursing curriculum.16 A self-instructional module for registered nurses was effective in increasing knowledge of basic human genetic concepts and risk assessment. 262 registered nurses involved in this study. Participants completed a pretest questionnaire used to measure baseline knowledge of basic human genetic concepts and risk assessment and collect descriptive data. Participants then reviewed a self-instructional module and completed a posttest questionnaire. There was a significant increase of 20.8% in participants' mean knowledge score on the posttest (M = 89.0%, SD = 8%, range = 67%-100%) as compared with the pretest (M = 69.0%, SD = 12%, range = 42%-92%), based on paired t-test analysis (t = 11.74, SE = 0.426, p < .0001). In conclusion self-instructional module is effective in increasing nurse’s knowledge.27 9 6.3. PROBLEM STATEMENT A study to evaluate the effectiveness of Self-Instructional Module (SIM) on knowledge regarding cardiac pacemakers among final year B.Sc. nursing students at selected nursing colleges, Bangalore. 6.4. OBJECTIVES OF THE STUDY 1. Assess the existing knowledge regarding cardiac pacemakers among final year B.Sc. nursing students by conducting pretest. 2. Evaluate the effectiveness of Self Instructional Module on knowledge regarding cardiac pacemakers among final year B.Sc. nursing students by comparing mean pretest and posttest knowledge scores. 3. Find the association between pretest knowledge scores regarding cardiac pacemakers among final year B.Sc. nursing students with selected socio-demographic variables 6.4.1. HYPOTHESES H1: -There will be significant difference between pre-test and post-test knowledge scores regarding cardiac pacemakers among final year B.Sc. nursing students. H2: -There will be significant association between pre-test knowledge scores regarding cardiac pacemakers among final year B.Sc. nursing students with selected socio-demographic variables. 6.4.2. RESEARCH VARIABLES Independent Variable: In this study the independent variable is Self Instructional Module on cardiac pacemakers. Dependent Variable: In this study the dependent variable is knowledge of final year B.Sc. nursing students regarding cardiac pacemakers. 6.5. OPERATIONAL DEFINITIONS Effectiveness: It refers to the positive changes that the Self Instructional Module will produce on knowledge of final year B.Sc. nursing students regarding cardiac pacemakers as evaluated by comparing the pre-test and post-test knowledge scores. Self Instructional Module: Self Instructional Module is a planned written material with appropriate visual aids for a person to learn by himself/herself so as to improve their knowledge regarding pacemaker. Knowledge: It refers to the awareness of final year B.Sc. nursing students regarding cardiac pacemakers as measured by the number of correct responses given to the items in the structured knowledge questionnaire. 10 Pacemaker: Pacemaker is an electronic medical device, implanted in the human body which generates electrical impulses at a pre- determined heart rate, to regulate the beating of the heart. Final B.Sc. nursing student It refers to students in their 4th year of Baccalaureate in nursing programme. 7. MATERIAL AND METHODS 7.1 SOURCES OF DATA: Data will be collected from final year B.Sc. nursing students at selected nursing colleges, Bangalore. 7.2 METHOD OF COLLECTION OF DATA 7.2.1 Inclusion and exclusion criteria Inclusion criteria B.Sc. nursing students who are Studying final year at selected nursing colleges, Bangalore. Willing to participate in the study. Available at the time of data collection. Exclusion criteria B.Sc. nursing students who are – not willing to participate in the study. not available at the time of data collection. 7.2.2 Research Design: Quasi-experimental, one group pre test –post test design 7.2.3 Setting: Selected Nursing Colleges, Bangalore 7.2.4 Sampling technique: Non probability sampling: Purposive sampling technique. 7.2.5 Sample size: The sample size will be 100. 7.2.6 Tools of research: A structured self administered knowledge questionnaire will be given to final year B.Sc. nursing students regarding cardiac pacemakers to assess the pre-test and post-test knowledge. The tool consists of two parts 11 Part A: Socio – demographic variables Part B: Structured self administered knowledge questionnaire on cardiac pacemakers 7.2.7 Collection of data: The investigator collects the data from final year B.Sc. nursing students. Pre test will be conducted by using structured self administered knowledge questionnaire. Later, Self Instructional Module will be distributed among final year B.Sc. nursing students to educate them about cardiac pacemakers. After 7 days, the post test will be conducted by using the same questionnaire to evaluate the effectiveness of SIM on cardiac pacemakers. The data collection period will be four weeks. 7.2.8 Method of data analysis and presentation: Data analysis will be done through descriptive and inferential statistics. Descriptive statistics: The investigator will use descriptive statistical techniques like frequency, mean, percentile and standard deviation for data analysis. The analyzed data will be presented in the form of tables, diagrams and graphs based on the findings. Inferential statistics: Test of significance such as t-test and chi square test will be used depending on the results obtained. 7.3 Does the study require any investigation to be conducted on patients or other human or animals? If so, please describe briefly? No, the study requires no investigations or interventions to be conducted on patients or other human beings or animals. This study includes knowledge assessment of final year B.Sc. nursing students and providing self instructional module 7.4 Has ethical clearance has been obtained from your institution in case of 7.3? Yes, Administrative permission and ethical clearance with regard to the study will be obtained from the institution and samples prior to conduct the study. 12 8. LIST OF REFERECE 1. www.abouthf.org/module10/default.htm - 14k 2. neocardiabcare.com/alarming-statistics-india.htm - 10k 3. www.top10notes.com/most-important-health-inventions/ - 28k 4. www.biology-online.org/dictionary/Cardiac_pacemaker - 25 5. Gregoratos, G., Abrams, J., Epstein, A.E., et al. (2002). ACC/AHA/NASPE 2002 Guideline update for implantation of cardiac pacemakers and antiarrhythmia devices: Summary article: A report of the American College of Cardiology/ American Heart Association task force on practice guidelines (ACC/AHA/NASPE committee to update the 1998 pacemaker guidelines). Circulation, 106(16), 2145-2165. 6. Nursing and Health Sciences, Monash University, Melbourne, Victoria, Australia. 2011, The Authors. Journal compilation ©2011 Wiley Periodicals, Inc. www.heartpoint.com/pacemakers.html 7. www.surgeryplanet.com/cardiology/pacemaker-implantation.html - 80k 8. www.heartpoint.com/pacemakers.html 9. Kawano T, Oshita S, et al., Preoperative assessment of patient with implanted cardiac pacemakers and defibrillators, Department of Anesthesiology, Tokushima University School of Medicine, Tokushima 770-8503. [Pub med]. 10. Pacemaker/defibrillator devices significantly reduce death & hospitalization in heart failure patients campanion trail: http://www.umm.edu/news/releases/pacemaker.htm#ixzz1qEGPzHvK September 14, 2011 in Cardiology 11. Chen HM, Chao YF., et al., Change in quality of life in patients with permanent cardiac pacemakers: a six-month follow-up study, School of Nursing, Chang Gung Institute of Nursing. [Pub med]. 12. Bavnbek K, Ahsan SY, et al., wound management and restrictive arm movement following cardiac device implantation - evidence for practice The Heart Hospital, University College London Hospitals, UK. [email protected]. [Pub med]. 13. Incidence and predictors of short- and long-term complications in pacemaker therapy: The FOLLOWPACE study Heart Rhythm 2008 14. Maisel WH. Pacemaker and ICD generator reliability: meta-analysis of device registries. JAMA. Apr 26 2006;295(16):1929-34. [Medline]. 15. Little L. About 9% of ICD and pacemaker patients have non-infectious complications. 2005 Medscape Medical News http: //www.medscape.com/viewarticle/504457. 16. www.inhc.ir/browse.php?a_id=69&slc_lang=en&sid=1&ftxt=1 17. FDA researchers identify new MRI safety risk for patients with pacemakers 11 Dec 2009 www.biomedcentral.com/presscenter/pressreleases/20091211 18. Complications related to permanent pacemaker therapy. www.medscape.org/viewarticle/588690 45k Kiviniemi MS, Pirnes MA, Eränen HJ, Kettunen RV, Hartikainen JE.Department of Medicine, Kuopio University Hospital, Finland. 13 19. Cardiac Resynchronization Therapy in Patients With a Narrow QRS Complex. Bleeker, Gabe B.; Holman, Eduard R.; Steendijk, Paul; Boersma, Eric; van der Wall, Ernst E.; Schalij, Martin J.; Bax, Jeroen J. Journal of the American College of Cardiology vol. 48 issue 11 December 5, 2006. p. 22432250 20. HeartRhythm Volume 7, Issue 6 , Pages 745-749, June 2010 Published by Elsevier Inc 21. Heart Rhythm Volume 2, Issue 8 , Pages 837-841, August 2005 22. Pacemaker patients' perception of unsafe activities: a survey http://www.biomedcentral.com/1471-2261/8/31 23. Pacing, CHF, and Patient Energy Level December 19, 2000 Left Ventricular or Biventricular Pacing Improves Cardiac Function at Diminished Energy Cost in Patients With Dilated Cardiomyopathy and Left Bundle-branch Block, Nelson GS, Berger RD, Fetics BJ, et al. Circulation 2000;102:3053-3059 24. Department of Cardiology, Arrhythmologic Centre, Ospedali del Tigullio, via Don Bobbio 25, 16033 Lavagna, Italy. [email protected] 25. Baas LS, Beery TA, et al., Care and safety of pacemaker electrodes in intensive care and telemetry nursing units, College of Nursing and Health, University of Cincinnati, Ohio, USA. [Pub med]. 26. Ruiz Rodriguez G, Madrazo Ríos JM, et al., Multiprogrammable pacemakers, Complications and Nursing care, Article in Spanish. [Pub med]. 27. Institute of Genetic Medicine, the John Hopkins University, Baltimore, MD 21287, USA. [email protected] [PubMed - indexed for MEDLINE] 14 9. Signature of the candidate : 10. Remarks of the guide : The research topic selected is appropriate as it attempts to enrich the knowledge among final year B.sc. nursing students regarding cardiac pacemakers, which helps to provide better care to the clients. 11. Name and Designation of 11.1. Guide : Mrs. N Sakthi Bharathi Asst. Professor, Mallige Institute of Nursing Sector II, HMT Post, Bangalore -13. 11.2 Signature : 11.3 Co-guide : Mrs. Mariam Jaisy G Assoc.Professor, Mallige Institute of Nursing Sector II, HMT Post, Bangalore -13. 11.4 Signature : 11.5 Head of the Department : Mrs. N Sakthi Bharathi Asst. Professor, Mallige Institute of Nursing Sector II, HMT Post, Bangalore -13. 11.6 Signature : 12. Remarks of the Chairman/Principal : This study is appropriate as it enhances the knowledge of nursing students in relation to Pacemaker. Since pacemakers are life saving devices used in certain cardiac emergencies 12.1 Signature : 15