* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Operational Definitions
Survey
Document related concepts
Transcript
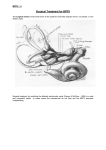
BPPV Operational Definitions Dates: Enter all dates using the format MM/DD/YYYY, with one digit in each box. Include a “0” in the first box for months or days with a single digit number. Enter the date the initial evaluation is being performed, the date of birth, and the patient’s age on the day of the initial visit. Enter the date of onset of current symptoms. If the patient cannot recall the precise dates, enter the first day of the month and year symptoms began. For example, 04/01/2008. Applicable Medical Diagnoses: Check only those diagnoses made by the referring physician at the time of the initial evaluation. If the diagnosis is not clear on the prescription, attempt to obtain records from the referring MD to include a working diagnosis. If no diagnosis has been made, leave all boxes blank. Vertigo History: Enter the date of the most recent vertigo attack, prior to the one that is currently being treated. Continue to use the format above for dates, with the first day of the month recorded if a specific date is unknown. Also record the date of the first episode of vertigo. If this is the first episode, enter the date of the evaluation. Record the number of prior vertigo attacks, not counting the current episode being evaluated. Enter “99” if the patient has had numerous attacks and can no longer recall an estimate of the number of attacks accurate within 2 episodes. If the vertigo is related to any incident of head trauma, indicate the day of the traumatic episode, or the first day of the month and year in which the trauma occurred. Medications: Record only medications prescribed to treat the current condition. Record any diuretic prescribed specifically for BPPV. Do not record diuretics previously prescribed for other medical conditions. Medications may include migraine medication, anxiety medication, steroids, vestibular suppressants or anti-nausea medications. Enter the date medications were started, again using the first day of the month if specific information is not available. Test Results: If VNG, ECoG or VEMP test results are available, enter test results. Record percentage of weakness for VNG and side(s) involved as well as any nystagmus of peripheral or central origin. ECoG and VEMP test results can be entered as ‘normal’ or ‘abnormal’ with reference to right or left sides. Whiplash History: Indicate whether the patient has a history of whiplash injury using the yes/no box selection. Then record the date of the injury using MM/DD/YYYY format if applicable. 1 Vertebral Artery Test: A vertebral artery test should be performed on all patients prior to evaluation of vertigo. Indicate presence or absence of a positive vertebral artery test. If positive, the patient should be referred to the MD. First Visit: Enter the date of the initial evaluation using MM/DD/YYYY format. Last Visit: When the BPPV is cleared, this is the date of the last visit. If a patient clears during the session, a final session will be scheduled to determine if the BPPV remains clear over the course of ½ to 1 week. If the BPPV is not cleared, but the patient is referred back to the physician for further medical work-up, indicate the date the patient was recommended to return to the MD. Discharge Date: If the patient discontinues therapy when the BPPV is clear, enter the date of the last visit. If the patient requires ongoing intervention, check the box for “further vestibular/balance therapy required”. Clinical Information Once a positive Dix-Hallpike is recorded at the initial evaluation, the patient will proceed with the following data collection at each visit. Each outcome measure should be performed in the sequence listed below, and all data should be collected prior to performing the Dix-Hallpike procedure and performing intervention. This sequence will allow assessment of the efficacy of the prior treatment session and baseline evaluation of symptoms at each visit prior to further intervention. Dizziness Analog: The patient should rate his or her dizziness on a scale of 0-10. A score of “0” indicates no dizziness. A score of “10” Nausea Analog: The patient should rate his or her dizziness on a scale of 0-10. A score of “0” indicates no nausea. A score of “10” indicates active vomiting. Falls: Record the number of fall reported by the patient. At the initial evaluation, record the number of falls in the last 6 months. At all other visits, record the number of falls since the prior visit. A fall is defined as “a sudden, unintentional change in position causing an individual to land at a lower level, on an object, the floor, or the ground, other than as a consequence of sudden onset of paralysis, epileptic seizure, or overwhelming external force.” (Tinetti) This definition of a fall is used by the Medicare Fall Prevention Act. Dizziness Handicap Inventory: Enter the score of the 5-item short form the Dizziness Handicap Inventory. The patient should complete the inventory at the onset of each visit, prior to any verbal dialogue, assessment or intervention that could influence results. All score sheets should be filed in the patient record. 2 Timed Up & Go (TUG): The TUG should be administered at each visit. Record the number of seconds and/or minutes to complete the test. Record the time and use the following key to indicate use of an assistive device: S = single point cane Q = quad cane H = hemi walker W = standard walker RW = rolling walker 4W = 4-wheel walker Dynamic Gait Index: Record the total score on the DGI conducted at each visit. Full score sheets should be placed in the patient record for reference to specific items. Indicate use of an assistive device with the above key as in the TUG. Dix-Hallpike Test: Record whether the patient has a positive Dix-Hallipke test on the right or left, with the direction of nystagmus observed according to the following key: +R UT +R DT +L UT +L DT +R V +L V + Right Dix-Hallpike, Upbeat torsional nystagmus, Right Posterior Canal BPPV + Right Dix-Hallpike, Downbeat torsional nystagmus, Left Anterior Canal BPPV + Left Dix-Hallpike, Upbeat torsional nystagmus, Left Posterior Canal BPPV + Left Dix-Hallpike, Downbeat torsional nystagmus, Right Anterior Canal BPPV + Right Dix-Hallpike, Vertical nystagmus, Central vertigo + Left Dix-Hallpike, Vertical nystagmus, Central vertigo Roll Test: Record whether the patient has a positive Roll Test on the right or left, with the direction of nystagmus observed according to the following key: +R, G +R, AG +L, G +L, AG + Right Roll Test, Geotrophic nystagmus + Right Roll Test, Ageotrophic nystagmus + Left Roll Test, Geotrophic nystagmus + Left Roll Test, Ageotrophic nystagmus Subjective Vertigo: If the patient has no nystagmus on Dix-Hallpike or Roll Test, but is symptomatic (significant elevation in dizziness or nausea), circle “Y”. If Dix-Hallpike and Roll Test are negative and there is no evidence of a typical vertigo presentation, circle “N”. Symptoms consistent with canal sensitivity following resolution of BPPV are NOT considered subjective vertigo. 3 Canal Treated: Based on findings from Dix-Hallpike and Roll Tests, indicate which canal(s) are to be treated at each visit. Use the following format: 1 – R Post 1 – L Post 1 – R Hor 1 – L Hor 1 – R Ant 1 – L Ant 2 – R Post 2 – L Post 2 – R Hor 2 – L Hor 2 – R Ant 2 – L Ant 1º Canal Treated – Right Posterior 1º Canal Treated – Left Posterior 1º Canal Treated – Right Horizontal 1º Canal Treated – Left Horizontal 1º Canal Treated – Right Anterior 1º Canal Treated – Left Anterior 2º Canal Treated – Right Posterior 2º Canal Treated – Left Posterior 2º Canal Treated – Right Horizontal 2º Canal Treated – Left Horizontal 2º Canal Treated – Right Anterior 2º Canal Treated – Left Anterior Interventions List the interventions utilized at each visit according to the numbers assigned in the table in the MDS form. Before the intervention indicate whether the intervention was used for the primary canal or secondary canal being treated by writing “1” or “2” and a dash. Following the assigned intervention number, place the number of repetitions of the intervention in parentheses. For example, if the modified Epley maneuver was performed three times in the same session for the primary affected canal, write “1-3(3)”. Separate each subsequent intervention using a comma. The numerical list of interventions described below correlates with the numbers assigned in the MDS form. Each item listed contains a description of the intervention with accepted method of performance for standardization. (1) Patient Education: Indicate if education is provided at the evaluation or any subsequent visit regarding the three systems for balance and regarding BPPV. (Handout) (2) Settling Techniques: Settling techniques utilized to reduce dizziness and nausea by increasing awareness of proprioceptive input. (Handout) (3) Modified Epley Maneuver (CRP): This maneuver is used to treat posterior or anterior canal BPPV. An example will be given for treatment following a positive right Dix-Hallpike (which could indicate either positive right posterior or left anterior canal depending on the direction of nystagmus). The patient starts in sitting (A) and is brought into supine with the head rotated to the right 45º and with the neck extended 20-30º (B). The position is held 15-30 seconds, then the cervical extension is maintained while the head is turned 45º to the left (C). This position is again held for 15-30 seconds. The patient is asked to roll onto their left side, and the head is turned to look down at the floor (D). The position is held 15-30 seconds, after which the patient returns to sit and maintains the head turned to the left side (E). 4 (4) Semont/Liberatory Maneuver: This maneuver is used to treat posterior canal BPPV. The example will be used for a positive right Dix-Hallpike revealing nystagmus that is clockwise in direction. The patient starts seated at the edge of a mat table with the head rotated to the right 45 degrees. Assist the patient to lie on their left side, maintaining the head rotated 45 degrees to the right. The patient should be in left sidelying with the head turned to look up at the ceiling and the neck extended so the head touches the table. Hold this position for 30 seconds. Assist the patient in maintaining the head rotated 45 degrees to the right and move back up through sitting and into right sidelying. The patient should now be lying on their right side while looking down to the floor. Hold this position for 30 seconds. Then return to sitting with the head still turned 45 degrees to the right side. (5) Lempert/BBQ Maneuver: The BBQ maneuver is used to treat horizontal canal BPPV. The example will be used to treat a positive right Roll Test. The patient begins in long sitting with the head rotated to the right side. The patient is assisted to a supine position with the head flexed 15-20 degrees. This position is held for 15-30 seconds, and then the head is rotated to the left side with maintained 15-20 degrees of cervical flexion and held in position 2 for 15-30 seconds. The head is held relatively still as the patient rolls through the left side and into prone on elbows with the head slightly flexed (chin tuck). Position 3, prone on elbows is held 15-30 seconds, and then the patient’s head is maintained in alignment while the patient rolls through the right side back into supine. The head is maintained in 15-20 degrees of flexion and turned to the left side. The patient remains in this position for 1-2 minutes prior to sitting upright. (6) Modified BBQ Maneuver: This is a slight variation of the BBQ roll, used for persistent horizontal canal BPPV. An example is provided with the use of a positive right Roll Test. The patient begins in long sitting on the mat with the head turned 45 degrees toward the affected (right) side. The patient is brought into a lying position with the head rotated to the left side 45 degrees as the patient comes down into supine, keeping the 5 head in slight flexion (20º). This position is held 30 seconds, followed by rolling through the left side onto prone on elbows. The prone position is maintained for 30-60 seconds. The patient is then rolled through the right side back to supine with the head maintained in 45º right rotation and 20º flexion. The position is held for 30-60 seconds before turning the head to the left 45º. The patient remains in the final position for 1 minute prior to returning to sit. (7) Liberatory Maneuver for the Horizontal Canal: This technique is recommended for clearing horizontal canal BPPV following a positive Roll Test with geotropic nystagmus. An example will be used for a positive right Roll Test. The patient begins sitting on the edge of a mat and is quickly brought into lying on the unaffected (left) side. The position is maintained for 1 minute. The head is then quickly turned 45 degrees downward to look at the floor, with the position held 1 minute. The patient then returns to sitting. (8) Mastoid Vibration: Mastoid vibration was originally used in the Epley maneuver. A vibrator is held behind the ear on the mastoid bone throughout the Epley maneuver to facilitate movement of the calcium carbonate crystals through the canal. Vibration is typically only used in posterior canal BPPV. Indicate how many Epley maneuvers are performed with vibration. (9) Cranial Oscillation: Indicate if cranial osciallation is performed. If performed, use the following procedure for treatment. The example of a positive right Dix-Hallpike with persistent BPPV, which has failed resolution using either the modified Epley CRP or the Semont/liberatory maneuvers in 3 PT sessions. Place the patient in left sidelying with the affected ear (right) up, but with the head tilted down to the left approximately 20 degrees. Use a gentle wrap such as ace bandage to position the vibrator behind the right ear on the mastoid bone. Have the patient remain in this position for 30 minutes with the vibrator on to help dislodge any otoliths jammed against the endolymphatic duct. This treatment should be repeated once weekly for 4 weeks. No sleep precautions should be given with cranial oscillation. No repositioning should be required at the cranial osciallation visits. (10) Post-Maneuver Precautions: Indicate if sleeping precautions were issued to the patient after repositioning. Sleep precautions include: Sleep with the head slightly elevated. This means approximately 1 extra pillow to maintain the head in slight flexion. Do not lie on the side which produced a positive Dix-Hallpike or Roll Test. Limit head motion. If the patient is conducting household activities, (s)he should be advised to keep the head stacked on the body and to bend at the knees to avoid tipping the head forward or backward, or performing head rotation for 24-48 hrs. 6 (11) Brandt-Daroff Exercises: The patient is instructed in the use of Brandt-Daroff exercises for use in the home to extinguish canal sensitivity following anterior or posterior canal BPPV. The exercises consist of sitting on the edge of a bed and lying onto the right or left side with the head turned to look up at the ceiling and the neck slightly extended to contact the bed surface. The position is held for 30 seconds, or until dizziness subsides. The patient then returns to sit on the edge of the bed for 30 seconds, and then lies on the opposite side with the head turned again to look up at the ceiling with the neck slightly extended. The position is held 30 seconds prior to returning to sit. The entire sequence is repeated twice, and is performed twice daily. 7