* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Orally Used Aminoglycosides
Urinary tract infection wikipedia , lookup
Trimeric autotransporter adhesin wikipedia , lookup
Microorganism wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Molecular mimicry wikipedia , lookup
Human microbiota wikipedia , lookup
Marine microorganism wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Magnetotactic bacteria wikipedia , lookup
Disinfectant wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Bacterial cell structure wikipedia , lookup
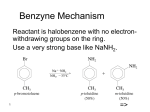
PHARMACOMEDICINAL CHEMISTRY I PHA 4430 [NSL] Antibacterial Antibiotics Antibiotics, antimicrobials or anti-infective agents. Agents used to treat infections by suppressing or destroying the causative microorganisms. Antibiotic traditionally refers to substances of microbiological origin that suppress the growth of other microorganisms. The term antibacterial is broader in meaning since it includes synthetic as well as natural compounds. Many currently used agents are produced industrially by chemical synthesis or are semisynthetic (main component of drug is obtained through fermentation followed by minor alterations). These are therefore appropriately described as antimicrobials. Historical Background: 500 to 600 B.C.: Chinese used molded curd of soybean to treat boils and carbuncles. Moldy cheese used by Chinese and Ukrainian peasants to treat infected wounds. 1929: Sir Alexander Fleming (a physician) accidentally discovered the antibacterial properties of penicillin when a pathogen culture he was preserving was contaminated by the airborne fungus, Penicillium notatum. The state of the art, his background and training hindered further development. 1938: Penicillin introduced into therapy by the group of English chemists that included Abraham, Heatley, Florey, and Chain. 1877: Pasteur and Joubert discovered that anthrax bacilli died in culture in the presence of other bacteria. Vuillemin coined the term “antibiosis” which literally means “against life” as a “survival of the fittest” concept of natural selection. Antibiotics are produced by microorganisms or are synthetic analogs. Antibiotics (at low concentrations) have the ability to inhibit the growth and/or kill other microorganisms. 1 Sources of Antibiotics: Antibiotic Microorganism Bacitracins Polymixins Tyrothricin Gramicidins Bacteria Bacillum lichenifirmis B. polymyxa B. brevis B. brevis Amphotericin Carbomycin Chloramphenicol Chloretetracycline D-Cycloserine 6-Demethyltetracycline Erythromycin Fusidic acid Kanamycins Neomycins Novobiocin Nystatin Oleandomycin Oxytetracycline Paramomycin Ristocetins Spiramycins Streptomycins Tetracycline Vancomycin Viomycin Actinomycetes Sterptomyces Spp. S. halstedii S. venezuelae S. aureofaciens S. lavendulae S. aureofaciens S. erythreus Fusidium coccinium S. kanamyceticus S. fradiae S. spheroids, S. niveus S. noursei S. antibioticus S. rimosus S. albo-niger Norcadia lurida S. albofaciens S. griseus Streptomyces Spp S. Orientalis S. floridae Penicillin Cephalosporin C Griseofulvin Fumugillin Fungi Penicillium notatum Cephalosporium notatum P. griseofulvum, P. nigricans Aspergillus fumigatus 2 Bateriostatic and Bactericidal Drugs: Bacteriostatic drugs: Arrest the further growth and replication of bacteria at serum concentrations achievable in patients. The body’s immune system then attacks, immobilizes and eliminates the pathogens. Bactericidal agents: Kill the bacteria. Medically Important Microorganisms: Gram (+) cocci Gram (+) bacilli Gram (-) Cocci Enterobacteriaceae Other Gram (-) bacilli Chlamydia Spirochetes Mycoplasma Others. 3 Antibiotic Spectrum: The spectrum of an antibiotic is the range of microorganisms that it is effective against. The spectrum indicates whether the antibiotic has limited or general cytotoxicity. Extended spectrum- refers to those antibiotics that are effective against gram positive and a significant number of gram negative bacteria. Broad spectrum- refers to antibiotics that are effective over a wide range of microbial species e.g. tetracyclines. The administration of a broad spectrum antibiotic might alter the nature of normal bacterial flora and cause a superinfection by other organisms such as Candida that would normally be competed against by the presence of other microorganisms. Due to the development of resistance, the term broad spectrum may be much less useful in clinically combating infections. Antibiotics Inhibitors of Bacterial Cell Wall Biosynthesis Bacterial Cell Wall: Bacterial cell wall is chemically distinct from mammalian structures. Differences exist between Gram (+) and Gram (-) bacteria cell walls. The Gram (+) cell wall is less complex than the Gram (-) cell wall. The Gram (+) bacteria cell wall consists of: o Characteristic polysaccharides and proteins on the outside that make up antigenic determinants, vary from species to species, recognize and bind to specific cell types. o The peptidoglycan layer, a spongy, gel-forming layer consisting of alternating N-acetylglucosamine (NAG) and N-acetylmuramic acid (NAM) linked (1,4)-β in a long chain. 4 o Beneath the peptidoglycan layer is the lipoidal cytoplasmic membrane which is the only layer that can prevent antibiotic entry. o Proteins float in this membrane layer. These include β-lactam receptors known as the penicillin-binding proteins (PBPs). o There are at least 7 PBPs believed to construct and repair the cell wall. 5 o β-Lactam antibiotics bind to these proteins and prevent them from fulfilling this role. Gram (-) bacterial cell walls are more complex and more lipoidal. They contain: o An additional outer membrane. o The outer membrane contains complex lipopolysaccharides that are antigenic, cause septic shock and influence morphology. o It also contains enzymes and exclusionary proteins such as porins. o Porins are transmembranal of 2 or 3 monomers with central pores of varying sizes, shapes and lipophilicity. o Because of this, antibiotics penetrate Gram (-) bacteria with greater difficulty than Gram (+) bacteria. o Below the outer membrane is the peptidoglycan layer that is less complex than that of Gram (+) bacteria. o Next is a periplasmic space that contains β-lactamases. o Then is the lipid-rich cytoplasmic membrane which contains PBPs (transpeptidases). o The β-lactamases remain in the periplasmic space (are not secreted as in Gram (+) bacteria). o There are energy-dependent proteins that pump out antibiotics. 6 Mechanism of Action of Inhibitors of Cell Wall Biosynthesis: o The antibiotics in this case selectively and irreversibly inhibit the enzymes that process the developing peptidoglycan layer. o Amide bonds are formed between the free –COOH of the lactic moieties of the N-acetylmuranic acid and a series of peptides of which L-Ala-D-GluL-Lys_D-Ala is typical. o The D-stereochemistry confers resistance to host peptidases. o The terminal D-alanyl unit is bonded to the Lysyl residue of an adjacent tetrapeptide through a pentaglycyl unit. o This last step is a transamidation whereby the terminal amino on the last glycine of the A strand displaces the terminal D-Alanyl unit of the nearby B strand forming a cross link. o The cross-linking adds structural strength on the 3rd dimension. o This provides the strong barrier against osmotic stress. o This step is catalyzed by a cell wall transamidase (one of the penicillinbinding proteins) which is highly sensitive to the β-lactam antibiotics. o The transaminase recognizes the β-lactam antibiotics as its normal substrate. o The highly strained β-lactam ring is more reactive than the typical amide bond. o However, while the normal substrate is hydrolyzed into two components (the terminal D-Ala unit diffusing away), hydrolysis of the β-lactams results in a heterocyclic structure still covalently bonded to the active site. 7 o This sterically hinders the pentaglycyl unit from the active site, prevents the active site from being regenerated and the cell wall precursors from being cross-linked. o Result = Defective cell wall and inactivated enzyme. o Water is too poor a nucleophile to be able to cleave the β-lactam-Enzyme complex. o The autolysins constitute a group of enzymes that enhance the effects of the β-lactams. o They hydrolyze the acetylmuramic acid to L-ala peptide bond causing the amino acid side chain to fall off. o 8 β-Lactam Antibiotics Lactam refers to cyclic amides. In older chemical nomenclature, the 1st carbon next to the –COOH of a carboxylic acid is α-carbon and the 2nd is the β-carbon, etc. Thus a β-lactam is a cyclic amide with 4 atoms in its ring. The β-lactam structure is the main component of the pharmacophore. The penicillin subclass has a 5-membered thiazoldine ring fused to the β-lactam to form a “V” shaped molecule. The β-lactam is thus strained and more sensitive to hydrolysis than the planar amides. Lactam N O H Ring and numbering systems of clinically available -Lactam antibiotics. 4 4 6 7 O 5 S 6 3 N 1 7 2 8 O 6 N 1 S N 1 2 N 1 O 2 Carbapenem 3 4 4 3 2 2 N 1 O Monobactam Cefem 9 4 3 7 Penem 5 S 5 6 3 O Penam 7 5 PENICILLINS: Original penicillins were derived from uncontrolled fermentations of the fungus, Penicillium chrysogenum. Mixtures were thus obtained in which different substituents on the β-Lactam moiety were obtained. Culture media enriched with phenylacetic acid resulted in it being preferentially incorporated into molecule to form benzylpenicillin or Penicillin G. When phenoxyacetic acid was used instead of phenylacetic acid, phenoxymethyl penicillin or Penicillin V was obtained. Other penicillins were obtained in this way but not used clinically. Completely excluding side chain acid precursors yielded 6-aminopenicillanic acid (6-APA) in poor yield. 6-APA is a poor antibiotic. It can however be chemically derivatized (partial chemical synthesis) on its primary amino with suitable side chains to enhance both its potency and antibacterial spectrum. Bacterial enzymes and more recently, chemical processes that specifically cleave less interesting side chains from β-lactams are used to produce suitable quantities of 6-APA for partial chemical synthesis of antibiotics to resist βlactamase and/or acid hydrolysis. Sodium and potassium salts of penicillins are crystalline, hygroscopic and water-soluble. They hydrolyze rapidly in aqueous solution (most stable in pH range of 6.07.2). Procaine and Benzathine salts benzylpenicillin are water-insoluble, used in formulations for continuous long-term delivery. 10 R1OCHN H H S CH3 6 * * CH3 N O * COOH * = asymmetric centers R1 Trade Name Fermentation-derived penicillins 6-Aminopenicillanic acid Benzylpenicillin (Penicillin G) Phenoxymethylpenicillin (Penicillin V) Semi-synthetic Penicillinase-Resistant Parenteral Penicillins Methicillin H C6H5-CH2C6H5-OCH2- Generic Generic OCH3 OCH3 Nallpen, Unipen C2H5O Nafcillin Semi-Synthetic Penicillinase-Resistant Oral Penicillins Oxacillin (X=Y=H) Cloxacillin (X=H, Y=Cl) Dicloxacillin (X=Y=Cl) Semi-synthetic Penicillinase-sensitive, Broad spectrum, parenteral Penicillins Carbenizillin (R2 = H) Carbenicillin phenyl (R2 = C6H5) ) Carbenicillin indanyl (R2 = X Bactocill Cloxapen N O CH3 Y Dycil, Pathocil COOR2 Geocillin COOH Tycar Ticarcillin S O Azlocillin (X=H) Mezolcillin (X=CH3SO2- Mezlin Piperacillin Pipracil X N O N H C6H5 O O C6H5 Semi-synthetic Penicillinase-sensitive, Broad-Spectrum, Oral Penicillins Ampicillin Amoxicillin N C6H5 O N N N NH2 Principen, Omnipen Amoxil, Trimox X Wymox 11 Clinically-Relevant Degradation Reactions of Penicillins: Most unstable bond is the highly strained and reactive β-lactam amide bond. It cleaves slowly in cold water but rapidly in hot water and in alkaline solutions to produce penicilloic acid. R1OCHN H H S N O R1OCHN H H CH3 OH- or -lactamase CH3 HO COOH S CH3 N CH3 O H COOH Penicilloic acid Penicillin inactive β-Lactamases in bacteria catalyze the cleavage of the same bond and constitute a principal mode of resistance to β-lactam antibiotics. Alcohols and amines also cause the cleavage of the β-lactam amide bond to form the corresponding esters and amides. **Amino-containing antibiotics such as aminoglycosides are incompatible with β-lactams as their amino groups react with the penicillins and the cephalosporins in this manner. **Nucleophiles in proteins conjugate with the β-lactams (haptens) to form antigenic conjugates that cause allergies to penicillins and related compounds. Such conjugates (penicilloyl proteins) may originate from culture as contaminants or may be high molecular weight self-condensation polymers formed in highly concentrated solutions. In acidic solutions, the side-chain at the 6 position is involved in the hydrolysis. H N R O O H H S N H CH3 H + O HO CH3 + H N R COOH Penicillin O H H S N H Penicilloic acid Penilloic acid, penilloaldehyde, D-penicillamine 12 CH3 CH3 COOH Note in the figure, the role of the carbonyl oxygen of the side chain amide in the acid-catalyzed reaction. R groups that are electron-withdrawing are more stable to acid hydrolysis and more suitable for oral systemic use. Electron-withdrawing groups reduce the electron density on the side chain carbonyl oxygen, thus increasing acid stability. Metal ions such as mercury, zinc and copper catalyze the degradation of the penicillins. Lipophilic side chains increase serum protein binding and protection from degradation but reduce the effective bactericidal concentration of the drug. Peniclillins are secreted into the urine by an active transport system in the kidneys. Resistance to β-Lactam Antibiotics: Intrinsic resistance due to reduced cellular uptake and lower affinity to the PBPs. Elaboration of the β-lactamases (enzymes or serine proteases produced by microorganisms that catalyze the hydrolysis of the β-lactam amide bond. The β-lactamases resemble the cell wall transamidases in their interactions with the β-lactam antibiotics. However, unlike the transamidases, the βlactamase active sites can be regenerated to degrade more β-lactam molecules. Gram (+) bacteria shed β-lactamases into the medium while Gram (-) bacteria shed them into the periplasmic space so that these enzymes encounter the antiobiotics before the antibiotics encounter the PBPs. Drugs: Benzylpenicillin: Used mainly against Gram (+) bacteria. It is cheap, shows efficacy and lacks toxicity except in highly sensitive cases. It is the most widely used antibiotic. Used against infections of the upper and lower respiratory and genitourinary tracts. Poor oral absorption and acid instability. Most effective route of administration is parenteral. 13 To combat the poor oral absorption, acid instability, sensitivity to βlactamases, narrow bacterial spectrum and allergenicity, other analogs were developed. Phenoxymethyl Penicillin: Fermentation media enriched with phenoxyacetic acid result in penicillin V. It is more acid stable than benzylpenicillin. This acid stability is believed to be due to the electronegative oxygen on the C-7 amide side chain that inhibits participation in the β-lactam bond hydrolysis. It is similarly sensitive to β-lactamases as is Penicillin G. Penicillinase-resistant Parenteral Penicillins: β-lactamases are less tolerant of bulky groups on the side chain amide than are the PBPs. An aromatic structure that is directly attached to the side chain amide with with dimethoxy ortho substitutions result in the β-lactamase-resistant Methicillin (unstable in acid, ½-life of 5 min at pH 2). Movement of one methoxy to the para position or replacement with a H causes susceptibility to β-lactamases. A methylene added between the aromatic ring and the 6-APA leads to βlactamase sensitivity. H3CO O O 6-APA 6-APA OCH3 OCH3 O * OCH3 O * 6-APA OCH3 H3CO Insensitive to-Lactamases * 6-APA O OCH3 OCH3 14 6-APA Sensitive to -Lactamases Penicillinase-Resistant Oral Penicillins: Formed by replacing the benzene ring with an isoxazolyl ring with a benzene on one flank and a substituted ring on the other flank. Oxacillin, Cloxacillin and dicloxacillin are more acid stable and can be taken orally. They are highly serum protein-bound and are not a good choice for treating septicemia. Penicillinase-sensitive, Broad-Spectrum, Oral Penicillins: Agents such as ampicillin are significantly acid stable and good for oral use. Many common gram (-) pathogens are susceptible. Side chain methylene is replaced by an amino group which when protonated, draws electrons from the side chain thus decreasing participation in β-lactam bond hydrolysis. Half-life of ampicillin is about 15 to 20 h at pH 2 and 35 C. Lacks resistance towards β-lactamases. Additives to ampicillin such as clavulanic acid are used to combat this βlactamase-susceptibility. Clavulanic acid is a mold product with little intrinsic antibacterial activity but is an excellent mechanism-based irreversible β-lactamase inhibitor. Sulbactam is also a β-lactamase inhibitor as clavulanic acid. Both agents are not useful against penetration barrier forms of resistance to antibiotics. Antigenic aggregates formed from intermolecular reactions of ampicillin amino groups with the β-lactam bonds of adjacent molecules may cause allergic reactions. H HO O S CH3 N CH3 O COOH Sulbactam O H O O S CH3 CH2OH N N N O COOH Clavulanic acid 15 N O COOH Tazobactam N Penicillinase-sensitive, Broad-Spectrum, Parenteral Penicillins: Also known as acylureidopenicillins due the presence of a variety of ureas on their structures. These include Azlocillin, Mezlocillin and piperacillin. They preserve the Gram (+) properties of ampicillin but have higher activities against Gram (-) bacteria. Longer side chain moiety may better mimic the peptidoglycan chain resulting in better binding interactions with the PBPs. β-lactamases are a source of resistance. Tazobactam is sometimes coadministered with piperacillin, the former inhibiting the β-lactamases. Carbenicillin and Ticarcillin: Carbenecillin is a benzylpenicillin in which one of the side chain methylene hydrogens has been replaced with a –COOH group. The stereochemical effect of the resulting compound is obliterated by the configurational instability. Isomers mutarotate to produce a mixture of isomers. The side chain –COOH enhances antiGram (-) activity to make carbenecillin one of the broadest-spectrum penicillin. It is acid-unstable, therefore parenteral administration often in conjuction with aminoglycoside antibiotics. Chemical incompatibility means the 2 must be kept in separate solutions until administration. Carbenecillin can decarboxylate to form benzylpenicillin which is useless against the organisms for which it is indicated. Large doses of Carbenecillin sodium may be required, which could be problematic for heart patients. 16 CEPHALOSPORINS Original cephalosporin-producing culture was Cephalosporium acremonium in sewage off the Sardinian coast. Components of the cultured products were active against penicillin-resistant bacteria due to their resistance to β-lactamases. The side chain of the not so potent compound was removed to form 7aminocephalosporanic acid (7-ACA) that could be derivatized with unnatural side chains in like manner to 6-aminopenicillanic acid. The semisynthetic procedures were aimed at: o Increased acid stability o Improved Pharmacokinetic properties o Broadened antimicrobial spectrum o Increased activity against resistant microorganisms o decreased allergenicity. The products differ from each other by virtue of antimicrobial spectrum, βlactamase stability, GI absorption, metabolism, stability and side effects. The cephalosporins are less reactive because their β-lactam ring is less strained since it is fused to a 6-membered rather than a 5-membered ring as in the peniccilins. The lost reactivity is compensated by the olefinic link between carbons 2 & 3. The β-lactam bond hydrolysis is modulated by the nature of both the C-3 and C-7. Antibiotic activity is significantly lost if the olefinic linkage is moved to carbons 3 and 4. Most cephalosporins form water-soluble sodium salts that are unstable in aqueous solution. Free acids are relatively water-insoluble. General structure H ROCHN 7 8 O H 6 4 S B A N 1 Ring A = b-Lactam ring 4 Ring B = Dihydrothiazine 3 R 2 COOH 17 Mechanism of Action: Cephalosporins are believed to kill bacteria by the same manner as penicillins through binding to penicillin-binding proteins followed by cell lysis. Resistance: Similar mode of resistance to the penicillins. Hydrolyzed by β-lactamases. Strategically placed steric bulk may impede access to β-lactamase active sites and thus confer resistance to β-lactamase hydrolysis. Allergenicity: Less common and less severe than in penicillins. Cross allergenicity with penicillins is relatively common. Can be administered to patients who have shown mild and delayed reaction to penicillin. Side effects mild and temporary nausea, vomiting and diarrhea due to disturbance of the normal flora. Nomenclature and Classification: Most cephalosporin generic names start with cef- or ceph-. First generation cephalosporins are active in vitro against mainly Gram (+) bacteria. Second generation cephalosporins retain the activity against Gram (+) bacteria but add better activity against some Gram (-) bacteria. Third generation cephalosporins are much more active against Gram (-) bacteria than either the 1st or 2nd generations. They are useful against multidrug-resistant, hospital-acquired bacteria strains. The appellation of first, second and third generation cephalosporins is roughly based on: o Time of discovery o Antimicrobial properties o With respect to their antimicrobial properties, 1st to 3rd generation is associated with broadening of gram-negative antibacterial spectrum, reduction in anti-gram (+) activity and enhanced resistance to βlactamases. 18 Therapeutic Applications: Resistance is common so in vitro tests are conducted to investigate susceptibility before therapy is instituted. Infections of upper and lower respiratory tract, skin, urinary tract, bone s and joints, bile tract, septicemias, endocarditis and intra-abdorminal and bile tract are treated with cephalosporins. Susceptible Gram (+) bacteria are treated with 1st generation cpds while Gram (-) and serious infections are treated parenterally with 3rd generation cpds. Metabolism: Hydrolysis of the β-lactam bond is the principal mode inactivation. Cephalosporins with acetyl group on side chain tend to be hydrolyzed to form a hydroxymethyl substituent at C-3. The resulting product may then undergo lactonization with the C-2 carboxyl group to form inactive products. H H ROCHN S N Deacetylation R O COOH Acylase -lactamase ROCHN H2N H H N S N S OH O R O H H ROCHN COOH 7-Aminocephalosporanic acid (7-ACA) HOOC H H COOH S HN Spontaneous lactonization R COOH Cephalosporoic acid ROCHN H H S N O O O Desacetylcephalosporin lactone 19 20 First Generation Cephalosporins ROCHN H H N X O COOH Generic name Trade name R X Salt OAc Na Parenteral agents Cephapirin Cefadyl N SCH2 pyridyl Cefazolin Ancef, Kefzol Zolisef N N CH2 N N tetrazolyl H3C S S Na N N thiadiazole Oral agents Cephalexin Keflex, Biocef Keftab D H HCl H - NH2 Cefadroxil Duricef D HO NH2 Oral and parenteral agents Cephradrine D Velosef NH2 21 H - Specific Agents: First Generation: Cephapirin: Pyridylthiomethylene-containing side chain. Relatively resistant to Staphylococcal β-lactamases but susceptible to other βlactamases. Subject to host deacetylation in liver, kidneys and plasma. Cefazolin: Less irritating on injection compared to related cpds. Longer ½ life than cephapirin. Dose should be decreased in kidney damage situations. Cephalexin: Contains ampicillin-like side chain which confers stability at low pH. Has no activating group at C-3, is thus less potent but is not metabolically deactivated Rapid and complete GI absorption. Cefadroxil: Amoxicillin-like side chain, therefore oral availability. Some evidence of immuno-stimulation through T-cell activation. Cephradine: Acid stable and rapidly and completely absorbed from GI tract. Parenteral and oral availability is useful in that the latter can replace the former as patient is discharged from hospital. 22 Second Generation Cephalosporins ROCHN Y H Z N X O COOH Generic name Parenteral agents Cefamandole Nafate Cefonicid D Mandol D Cefuroxime Cefoxitin Mefoxitin Cefotetan Cefotan Salt H S - H S diNa CH2OCONH2 H S Na N H3C N NN S OH Ceftin Kefurox Zinacef Z S OCHO Monocid Y X R Trade name HO3S N N NN NOCH3 O S CH2OCONH2 OCH3 H2NOC S S HOOC S H3C N N NN OCH3 S Na S diNa Oral agents Cefaclor D Ceclor Cl H S Cl H CH2 H S NH2 Loracarbacef D Lorabid NH2 Cefprozil Cefzil CH3 D HO NH2 23 Specific Agents –Second Generation: Cefamandole Nafate: C-7 side chain formate ester apparently stabilizes cefamandole when stored in dry form. C-7 side chain formate ester is rapidly cleaved in host to release cefamandole. Loss of C-3 5-thio-1-methyl-1-H-tetrazole (NMTT) group is linked to thrombin deficiency and bleeding as well as acute alcohol intolerance. Used against susceptible organisms in respiratory and urinary tracts, skin, bone and joint infections and septicemia. Cefonicid: Similar group at C-7 as cefamandole except that it is not esterified. C-3 methylsulfothiotetrazole group. Lacks side effects of cefamandole. Unstable in light and heat. Longer half-life than group members. Cefuroxime: Has Syn-oriented methoxyimino moiety as part of C-7 moiety which confers resistance to most β-lactamases. Resistance to Pseudomonas may be due to lack of penetration. C-3 carbamoyl moiety shows intermediate metabolic stability compared to acetyl and thiotetrazoles. Its penetration into the cerebrospinal fluid means that is used to treat H. influenzae meningitis Cefuroxime axetil is a more lipophilic pro-drug form that shows good oral availability. It is activated by de-esterification to an intermediate that loses acetaldehyde spontaneously to form cefuroxime. Stable for up to 24 h when dissolved in apple juice. 24 O H H H C N S O N OCH3 O Cefuroxime axetil N O O O C NH2 C O O C CH3 O CH3 Cefoxitin: The H at C-7 is replaced by an α-oriented methoxy. The increased steric bulk confers resistance against β-lactamases. This feature (methoxy) was inspired by its presence in cephamycin C, natural antibiotic. Cefoxitin is useful against gonorrhea. Cefotetan: C-7 methoxy is also cephamycin-inspired. C-3 5-thio-1-methyl-1-H-tetrazole (NMTT) implies caution against bleeding and alcohol consumption. Incompatible with tetracycline, aminoglycosides and heparin due to formation of ppts. Better activity against anaerobes (like cefoxitin) than other 2nd generation cephalosporins. Causes cell lysis and death of Gram (-) bacteria Cefaclor: Differs from Cephalexin primarily by the bioisosteric replacement of C-3 – CH3 with Cl. Acid-stable and good orally. Loracarbef: Synthetic C-5 “carba” analog of cefaclor. Smaller methylene (than S) makes drug more reactive and more potent. More stable chemically. Diarrhea is common side effect especially in children. Cefprozil: Amoxicillin-like side chain at C-7 and a 1-propenyl at C-3. 25 The 1-propenyl group is present in its 2 geometric forms, both of which are active. The trans form is more preponderant and much more active. About 90% is orally bioavailable. 26 Third Generation Cephalosporins Y H ROCHN S N X O COOH Generic name Parenteral agents Cefotaxime N OCH3 Claforan Salt X R Trade name CH2OAc N Na H2N Ceftrizoxime N OCH3 S N Cefizox Na H2N S Ceftrioxone H N OCH3 H2CS N Rocephin N H2N S Ceftazidime Cefoperazone Fortaz Ceptax Tazidime Tazicef CH3 N O C COOH CH3 N H2N HO Cefobid H or Na N N O O NH N N N N H3C O N OCH2COOH N H2N C CH2 H S CH2COOH Ceftibuten Cedax N H H2N S N OCH3 Cefpodoxime proxetil Vantin N CH2OCH3 H2N S N OH Cefdinir Omnicef diNa O CH2 S C2H5 N Suprax OH S Oral agents Cefixime CH3 N N N H2N S 27 C CH2 H Na Specific Agents Third Generation Cefotaxime: Like cefuroxime, has syn-methoxyimino moiety at C-7 which conveys βlactamases-resistance. May induce chromosomal-mediated β-lactamases in some organisms. Like other 3rd generation cpds, it has excellent activity against gram (-) bacteria. 90% of its activity is lost when the C-3 acetoxy group is metabolically hydrolyzed. Heat and light-sensitive. Ceftizoxime: C-3 side chain is omitted to prevent deactivation. Ceftriaxone: Shares common C-7 moiety with cefotaxime and ceftizoxime. C-3 side chain is metabolically stable and activating thiotriazinedione. Used to treat some meningitis infections caused by Gram (-) bacteria. Stable to β-lactamases except some inducible chromosomal β-lactamases. Ceftazidime: The Oxime on the C-7 side chain is more complex. Thus causes more stability against β-lactamases. The C-3 pyridinium enhances water-solubility and highly activates the βlactam ring towards cleavage. Not stable under certain conditions such as the presence of aminoglycosides, NaHCO3 and vancomycin. Resistance is due to inducible β-lactamases and lack of penetration. Cefoperazone: Has C-3 NMTT associated with bleeding and alcohol intolerance. C-7 side chain does not confer sufficient resistance against β-lactamases. Cefixime: Syn-oximino acidic ether at C-7 confers β-lactamases stability. Anti-Gram (-) potency intermediate between 2nd and 3rd generation cpds. 28 Orally active. Ceftibuten: A cis ethylidinecarboxyl at C-7 confers resistance to β-lactamases. The 75-90% oral availability is significantly decreased by food. Its lipophilicity and acidity increases its serum protein binding. Used for respiratory, otitis media, pharyngitis, tonsillitis and UT infections. Cefpodoxime Proxetil: It is a prodrug that is enzymatically cleaved to cefpodoxime in the walls of the gut. Used against pharyngitis, UT, upper and lower respiratory and skin infections. Cefdinir: Has an unsubstituted syn-oxime at C-7. This may account for its improved Gram (+) activity. Oral availability is 20-25%. Specific Agents -Fourth Generation Agents: Agents are characterized by enhanced antistaphylococcal and broader antiGram (-) activity than the 3rd generation of cpds. Cefepime has a syn-methoxyimine and an aminothiazolyl group at C-7 which broaden its spectrum and increases β-lactamase stability. Quaternary N-methylpyrrolidine group at C-3 may help its penetration of Gram (-) bacteria. O S H2N C N N OCH3 H H H N S N O Cefepime (Maxipime) N H3C COOH 29 Other β-Lactam Antibiotics: Carbapenems: Thienamycin and Imipenem: Thienamycin was isolated from Streptomyces Cattleya. Extremely intense and broad sprectrum antibiotic. It inactivates β-lactamases as well kills the bacteria in like manner to the other β-lactam antibiotics by binding to the PBPs. It differs from the penicillins and cephalosporins in that the ring sulfur atom is replaced by a methylene group. This causes a significant ring strain since C is about half the size of S. The Carbapenem ring system is highly reactive and susceptible to the βlactam bond cleavage. Endocyclic olefinic bond also increases reactivity of the β-lactam ring. The nucleophilic terminal amino group attacks the β-lactam ring especially in concentrated solutions making theinamycin very unstable. This amino group was thus changed to a less nucleophilic N-formiminoyl by a semisynthetic process to achieve imipenem. There is a C-6 2-hydroxylethyl group with α-stereochemistry. Absolute conformation is 5R,6S,8S which is different from the penicillins and the cephalosporins. They bind differently to PBPs with very broad spectrum and potent activity. Both penetrate the porins well, are stable and even inhibit β-lactamases. Imipenem is less effective in UT infection treatment because renal dehydropeptidase-1 hydrolysis and inactivates it. In combination with cilastatin (an inhibitor of renal dehydropeptidase-1), it is highly efficacious. 30 HO H CH3 H H HO H NH2 S N CH3 N O O COOH Thienamycin HO H N H H H N O NH S COOH Imipenem NH2 H3C H3C CH3 HN H H C COOH Cilastatin H S COONa CH3 H H S O H NH CH3 N CH3 Meropenem COOH Meropenem: Synthetic carbapenem with a more complex side chain at C-3 and a chiral methyl group at C-5 which confers resistance to hydrolysis by dehydropeptidase-I. It can be administered as a single agent in the treatment of severe bacterial infections. Monobactams Monocyclic β-lactam antibiotics obtained by fermentation of unusual microorganisms. None has proven important except in inspiring the synthesis of Aztreonam. Aztreonam: Totally synthetic parenteral antibiotic almost totally devoted to the treatment of Gram (-) bacteria. Capable of inactivating some β-lactamases. Unprecedented sulfamic acid moiety attached to the β-lactam ring. The electron-withdrawing nature of the sulfamic acid group makes the βlactam bond vulnerable to hydrolysis. The α-methyl at C-2 increases stability to β-lactamases. MOA similar to those of the penicillins, cephalosporins and the carbapenems. 31 Primarily used to treat hospital-derived severe Gram (-) infections. Used against UT, upper respiratory, bone, cartilage, abdorminal, obstetric, gynecologic infections and septicemia. O H CH3 S H2N HN N N O H3C H N O SO3Na CH3 CO2Na 32 Aztreonam disodium Inhibitors of Bacterial Protein Biosynthesis Both eukaryotic and prokaryotic cells synthesize their proteins on ribosomal assemblies with similar sequences of events. In bacteria the 70S ribosomal particle is made up of RNA and 55 different structural and functional proteins (21 on the 30S and 34 on the 50S particle). The bacterial ribosomal proteins differ from the eukaryotic 80S ribosome. The antibiotics bind to sites on the proteins or the nucleic acid of the 70S ribosome. Aminoglycosides bind to a site on the mRNAs of the 30S subparticle. Macrolides, lincosaminides and chloramphenicol bind to a site on the 50S subparticle. The tetracyclines bind to sites on both subparticles. At normal doses, the compounds do not bind to nor interfere with 80S (of eukaryotes) protein synthetic machinery. These agents thus interfere with bacterial protein synthesis thus preventing repair, cellular growth and reproduction. At clinical doses, they are either bacteriostatic or bactericidal. Tetracyclines Consist of highly functionalized partially reduced naphthacene ring. Naphthacene is 4 linearly fused 6-membered rings, hence tetracyclines. 7 6 5 5a 8 D 4 4a A B C 3 9 2 11a 10 Naphthacene 11 12a 12 1 Tetracycline They are amphoteric in nature with 3 pK values that can be determined by titration (2.8-3.4, 7.2-7.8 and 9.1-9.7. Isoelectric point is about pH 5. The basic group is the C-4-α-dimethyylamino moiety. 33 Water-soluble HCl salts are marketed. The conjugated enone system from C-10 to C12 is associated with pKa of 7.5. The conjugated trione from C-1 to C-3 is associated with pKa of 3. Chelation is an important feature of tetracycline chemistry as salts with polyvalent cations (Fe2+, Al3+, Ca2+, Mg2+) are insoluble at neutral pH. This makes solution preparation difficult and also interferes with oral absorption to achieve adequate blood levels. They are incompatible with co-administered multivalent ion-rich antacids, daily consumption of Ca-rich products. Bones (rich in Ca) accumulate tetracyclines. Progressive and permanent coloration of teeth with the yellow color of tetracyclines occurs with long term use. Extreme absorption of the tetracyclines eventually weakens the teeth. Not given to kids when permanent teeth are forming. Tetracycline injections are painful due to the formation of insoluble Ca complexes. Oral administration is the preferred route. Injectable preparations contain EDTA and buffered at pHs<7 to minimize chelation. X R1 R2 R3 H N(CH3)2 OH H NH2 OH Generic name Tetracycline Demeclocycline Minocycline Sancycline Oxytetracycline Methacycline Doxycycline O OH OH O O Trade Name X R1 Achromycin Sumycin Tetralan Declomycin Minocin H OH CH3 H OH H H OH H H H CH3 CH2 CH3 H H H OH OH OH Teramycin Vibramycin Doryx Cl N(CH3)2 H H H H 34 H R2 R3 Cehimical instability of the Tetracyclines: Epimerization The α-stereo orientation of the C-4 dimethylamino moiety is essential for bioactivity. The tricarbonyl system of ring A allows for enolization that involves the loss of the C-4 hydrogen. Reprotonation could be from above or below the ring. Reprotonation from above the ring regenerates tetracycline while reprotonation from below creates inactive 4-epitetracycline. At equilibrium, ~ equal proportions of both diastereoisomers exist. Old tetracycline may only contain 50% of its original activity. During manufacture, capsules are overfilled by 15% to maintain a shelf life at approximately the labeled dose. Epimerization of tetracycline OH X R1 R2 R3 H H X N(CH3)2 OH R1 OH H OH OH O NH2 H NH2 O N(CH3)2 H Base H OH R3 R2 OH O O OH OH O Tetracycline H Base X R1 R2 R3 H H N(CH3)2 OH H NH2 OH O OH OH O O 35 4-epitetracycline O Dehydration Most natural tetracyclines have a C-6 tertiary and benzylic hydrogen. This has the ideal geometry for acid-catalyzed dehydration involving the C-5a α-oriented hydrogen. The product is a naphthalene derivative. The C-5a,6-anhydrotetracycline is much deeper in color than tetracycline and is biologically inactive. Discolored tetracycline should thus be discarded. Inactive 4-epitetracyclines can dehydrate to form 4-epianhydrotetracyclines and anhydrotetracycline can epimerize to produce the same product. 4-epianhydrotetracyclines are toxic to the kidneys and is fatal in extreme cases. Commercial samples are thus closely monitored for 4epianhydrotetracyclines. 36 Base-Catalyzed Cleavage At or above pH 8.5, cleavage of the C-ring occurs. This involves the C-6-hydroxyl group. The product, isotetracycline, is an inactive lactone. OH X H3C H H X N(CH3)2 OH Base H H CH3 OH O O O OH O NH2 NH2 OH N(CH3)2 OH O O O OH O O Isotetracycline Tetracycline Photosensitivity Some tetracyclines, especially those with a C-7 chlorine absorb visible light and generate free radicals that cause severe erythryma in sensitive patients on exposure to sunlight. Mechanism of Action of Tetracyclines: Tetracyclines bind to 30S and perhaps 50S ribosomal particles. When bound, it inhibits the binding of aminoacyltransfer-RNA to the ribosome. This leads to premature polypeptide chain termination and non-functional proteins. More lipophilic tetracyclines such as minocycline disrupt cell membrane function. This causes leakage nucleotides and other essential cell molecules. Mechanism of Resistance to Tetracyclines: Elaboration of the bacterial proteins TET (M), TET (O) and TET (Q). The proteins interact with ribosomes making them continue protein synthesis even in the presence of bound tetracyclines. R-factor-mediated, energy-requiring, active efflux of Mg2+-chelated tetracyclines is particularly prominent in Gram (-) bacteria. Mycoplasma and Neisseria have membranes that either accumulate less tetracyclines or have porins that are less permeable to tetracyclines. 37 Binding to eukaryotic 80S ribosomes at high doses and consequent anabolic suppression is problematic especially in pregnancy situations. Therapeutic Uses: Wide range of bacteriostatic activity. Resistance and side effects has discouraged their use. Used at low dose oral and topical treatment of acne and UT infections, STDs, respiratory tract and ophthalmic infections, prophylaxis for malaria, traveler’s diarrhea, cholera, Helicobacter, Lyme disease, etc. Also used in large quantities in agriculture. Drugs: Tetracycline: Produced by fermentation of Streptomyces aureofaciens and related species or be catalytic reduction of Clortetracycline. Oral absorption is irregular due to possible interferences from ions in food and milk. It is generic and comparatively cheap. Demeclocycline: Lacks the C-6-methyl of tetracycline. Produced by fermentation of a genetically modified S. aureofaciens. It is a secondary alcohol, thus less prone to dehydration than tetracycline. Food and milk consumption adversely affects its absorption by 50% of the 50-80% absorption rate. Minocycline: Semisynthetic from demeclocycline. The C-7-chloro and C-6-hydroxy can both be removed by catalytic reduction to yield sancycline. Minocycline is more lipophilic than precursors, 90-100% is absorbed. Food and milk will reduce absorption by ~20%. Less painful on IM administration, broader antimicrobial spectrum. 38 Oxytetracycline: Obtained by fermenting Streptomices rimosis and other soil microorganisms. Most hydrophilic tetracycline in use. 60% bioavailable. Doxycycline: Well absorbed (90-100%, 70-90% with food or milk) following oral administration. Causes fewer gastrointestinal disturbances. Does not degrade through dehydration involving C-6. Therefore tetracycline of choice. 39 Aminoglycosides and Aminocyclitols Contain 1,3-diaminoinositol moiety as pharmacophore. The 1,3-diaminoinositol could either be streptamine, 2-deoxystreptamine or spectinamine. H2N NH HN 2 1 OH HO NH2 N HO OH H NH Streptamine H2N HO HO OH NH2 2-deoxystreptamine H3CHN HO HO OH OH NHCH3 Spectinamine Several of the –OH groups of the 1,3-diaminoinositol are substituted through glycosidic bonds with characteristic aminosugars to form pseudooligosaccharides. The combination of 1,3-diaminoinositol and the arrangement and identity of the substituents account for the chemistry, spectrum, pharmacokinetics, potency and toxicity of the different compounds. The aminoglycosides are water-soluble at all pHs. They are basic and form acid salts. Are not readily absorbed from the GI tract. Oral administration is mainly for GI infections. Excreted in active form at high concentrations by the kidneys following IM injection or perfusion. Sprays of tobramycin into the lungs have been used to treat lung infections in cystic fibrosis patients. Toxicity: Toxic levels may be attained if doses are not modified in kidney damage. They have a broad spectrum of activity but are limited to treat severe Gram (-) due to their potential for toxicity. Hearing loss and vertigo due to interference with the 8th cranial nerve. Kidney tubular necrosis resulting in decreased glomerular function is also associated with their use. Curare-like neuromuscular blockade due to competitive inhibition of Calciulion-dependent acetylcholine release at neuromuscular junction. 40 The latter can exacerbate muscle weakness in myasthenia gravis and Parkinson’s disease. Toxic effects may be of delayed onset. Mechanism of Action: At sub-toxic levels, aminoglycosides bind to external lipopolysaccharides and diffuse into the cytoplasm of the bacteria cells where they bind to 16Sribosomal DNA portion of the 30S ribosomal subparticle. This impedes the proofreading function of the ribosome. Mistranslation of the mRNA template occurs, use of the wrong amino acids and the synthesis of nonsense proteins that cannot fulfill cellular functions. The unnatural proteins upset the membrane function of the bacteria. The semi-permeability of the membranes is destroyed and cannot be repaired without the de novo synthesis of functional proteins. Initial membrane damage leads to increased penetration of aminoglycosides which causes the protein synthesis machinery to halt altogether. The initial diffusion of aminoglycosides into the cell is inhibited by Ca and Mg ions and are partially incompatible therapeutically. At high concentrations, aminoglycosides/aminocyclitols will also inhibit eukaryotic protein biosynthesis. Resistance: Increased synthesis of R-factor mediated enzymes that N-acetylate, Ophosphorylate and O-adenylate specific functional groups. These groups subsequently sterically prevent binding of the aminoglycosides to ribosomes. Chemical modification of the antibiotics by deleting the targeted functional groups still results in a molecule with antibiotic properties but no longer a substrate. Resistance due to decreased penetration of aminoglycosides into bacteria is also encountered. Therapeutic Applications: Show broad spectrum of activity against both Gram (+) and Gram (-) bacteria. Serious and delayed onset toxicities mean the agents are reserved for serious Gram (-) infections. 41 They are active against Gram (-) aerobes such as Acenetobacter sp., Citrobacter sp., Eneterobacter, Klebsiella sp., E. coli, Salmonella sp., Shigella sp., etc. Streptomycin is used mainly against tuberculosis and spectinomycin against gonorrhea. Drugs: Kanamycin: Mixture of at least 3 components; A, B and C, with A predominating. It is isolated from Streptomyces kanamyceticus Gentamicin, neomycin and paromomycin are among the most chemically stable of the antibiotics. Can be heated for prolonged periods of time in acid or alkali and can withstand autoclaving. Kanamycin is O-phosphorylated on the C-3’ –OH. It is also N-acetylated on the C-6’ amino group. Both reactions inactivate the antibiotic. Pseudomonas aeruginosa and anaerobes are usually resistant. Injections of Kanamycin are painful enough to require local anesthetics. Amikacin: Derived from Kanamycin by semisynthesis. The L-hydroxylaminobuteryl amide (HABA) moiety at N-3 inhibits adenylation as well as phosphorylation in the distant amino sugar ring (at C-2’ and C-3’) despite the HABA not being where the actual phosphorylation occurs. This is believed to be due to decreased affinity for the R-factor-mediated enzymes. This change enhances both potency and spectrum. 42 6' NH2 O O-adenylation HO X 3' N-acetylation 1' H 2' Y Phosphorylation N-acetylation H2N O HO 1 NHR 3 O HO HO Tobramycin (X=H, Y=NH2, R=H) Kanamycin A (X=OH, Y=OH, R=H) Amikacin (X=Y=OH, R=COCHOHCH2CH2NH2) O OH O-adenylation H2N N-acetylation Tobramycin: One of components (factor 6) from Streptomyces tenebrarius fermentation. Lacks C-3’ –OH, therefore is not O-phosphorylated. It is inactivated by adenylation at C-2’, acetylation at C-3 and C-2’. Widely used parenterally to treat difficult infections. Gentamicin: Mixture of several component antibiotics with Gentamicin C-1, C-2 and C-1a being the major components. Fermented from Micomonospora purpurea and other related microorganisms. It is the most important of the aminoglycoside antibiotics still in use. Used against the virulent Pseudomanas aeruginosa infections of burns, pneumonias and UT infections. Most targets for the R-factor enzymes are absent, thus improving their antibacterial spectrum. They are however inactivated through C-2’ adenylation and C-6’ and C2’ acetylation. -Lactam antibiotics will react with the C-1 amino, causing both antibiotics to lose potency. 43 NH2 H3C N-acetylation lactam antibiotics O NH2 N-acetylation H2N O 1 HO N-acetylatin NH2 O Gentamicin C-2 O HO O-adenylation CH3 NHCH3 OH Neomycin: Mixture of 3 compounds obtained from Streptomyces fradiae. Used in preoperative bowel sanitation E. coli infections. NH2 O HO HO NH2 H 2N O Neomycin B HO NH2 O OH O O H2 N O OH NH2 OH OH Netilmicin: Similar clinical properties as gentamicin and tobramycin. Orally Used Aminoglycosides Kanamycin, neomycin and paromomycin are used in certain cases to suppress gut flora. This is prophylactic before gut surgery to avoid post surgical peritonitis. Paromomycin is used to treat amoebic dysentery. 44 Streptomycin: *Modified pharmacophore –diaminoinositol is streptamine. Streptomycin has an axial hydroxyl group at C-2 and 2 highly basic guanidino groups at C-1 and C-3 instead of the primary aminos in 2deoxystreptamine. Produced by fermentation of Sterptomyces griseus and related soil microorganisms. Most useful aminoglycoside antibiotic against tuberculosis, introduced in 1943. Its usefulness against tuberculosis was such that its discoverer, Selmon Waksman, was awarded the Nobel Prize in 1952. -Hydroxyaldehyde is unstable making sterilization by autoclaving impossible. Therefore sterilized by ultrafiltration. Resistance to streptomycin is by N-acetylation, O-phosphorylation and Oadenylation of specific functional groups in the molecule. Streptomycin is not useful against unusual mycobacteria of immunosuppressed AIDS sufferers. It is useful against bubonic plague, leprosy and tularemia. Streptomycin H2N NH HN Streptidine ring H OH N HO HO NH CHO H3CHN O H O OH O Adenylation & phosphorylation HO OH 45 OH NH2 CH3 Spectinomycin: Obtained by fermenting Streptomyces spectabilis. The diaminoinositol unit (spectinamine) contains 2 mono-N-methyl groups and the –OH between them is of a stereochemistry that is opposite to that of spectinomycin. The glycosidically attached sugar is unusual in having 3 overt or masked carbonyls, fused by 2 bonds to spectinamine to form an unusual fused 3 ring structure. Spectinomycin is bacteriostatic when used in a single bolus IM injection against (penicillinase-producing) Neisseria gonorrhea. Resistance to spectinomycin by an unknown mechanism. CH3 OH HN OH O O NHCH3 O OH O CH3 Spectinomycin 46 Spectinamine ring Macrolides: The term macrolide is derived from the large lactone ring found in them. The clinically important members have 2 or more characteristic sugars attached to the 14-membered ring. One of the sugars carries a substituted amino group that makes them weakly basic overall (pKa = 8). Free bases are not soluble in water. Certain salts (with glucoheptonic and lactobiononic acids) are more water-soluble. Other salts (with laurylsulfonic and stearic acids) are less soluble. Macrolides with 16-membered rings are popular outside the US; one exception (tylosin) finds extensive agricultural use in the US. The 14-membered ring macrolides are synthesized from propionic acid units making every second carbon (of erythromycin) bear a methyl group and the other carbons (except 1) bear oxygens. Two hydroxyls are glycosylated while 2 carbons bear extra oxygens added after ring synthesis. Mechanism of Action: Inhibit ribosomal protein biosynthesis by inhibiting translocation of aminoacyl t-RNA. These bind to domain V of bacterial 23S rRNA. Resistance: R-factor enzymes methylate a specific guanine nucleotide on their own rRNA. This methylation decreases protein synthesis efficiency but makes macrolides bind poorly to them. The soil microorganisms that produce erythromycin employ this mechanism to protect themselves from this toxin. Another mechanism of resistance is through mutation of adenine 2058 to guanine which decreases the binding affinity of erythromycin and clarithromycin to 23S rRNA by 10,000-fold. Active efflux requiring energy also accounts for resistance in some cases. Resistance in Gram (-) bacteria is mainly due to lack of penetration since isolated ribosomes are susceptible. 47 Chemical Reactivity: Erythomycin-like macrolides are unstable in acid due to the formation of internal cyclic ketal that makes them inactive. Acid-catalyzed intramolecular ketal formation H+ + H N(CH3)2 RO O HO O O HO O HO OH N(CH3)2 O HO O OH OCH3 RO O O OH O O O N(CH3)2 RO O HO O O O O O OH OCH3 O O O O O OH OCH3 Inactive spiroketal Active macrolide Therapeutic Application: Used for the treatment of upper and lower resp. tract infections caused by Gram (-) bacteria. Prophylaxis against endocarditis. Together with sulfonamides are used to treat otitis media infections caused by haemophilus influenzae. Mycoplasmal infections in AIDS, multidrug cocktails to treat H. pyloricaused gastric ulcers. Used orally for mild systemic infections. Oral absorption is somewhat irregular especially when taken with food. Drug-Drug Interactions: Competition for oxidative liver enzymes (CYP3A4 of the P-450 family) with other drugs may increase ½ lives leading to severe toxicity. Interfering drugs include ergotamine, theophylline, carbamazepine, bromocryptine, warfarin, digoxin, oral contraceptives, cyclosporin, astemizole, terfenadine, midazolam, triazolam and methylprednisone. 48 Drugs: Erythromycin Estolate: One of the 2 most popular prodrugs that leads to higher blood levels. It has a C-2”-propionyl ester. It is an N-laurylsulfate salt. In a minority of cases, severe cholestatic jaundice occurs in which granular bile forms in the duct blocking flow and causing the bile salts to back up into the circulation. Drug must be replaced with non-macrolide cpd. R N(CH3)2 RO O9 HO Erythromycin base H -----Erythromycin HCl H HCl Erythromycin Estolate COCH2CH3 CH3(CH2)11OSO3H Erythromycin Ethylsuccinate CO(CH2)2CO2C2H5 ---Erythromycin Gluceptate H Structure A Erythromycin lactobionate H Structure B Erythromycin Stearate H CH3(CH2)16COOH 10 O O HO 6 OH 14 O O O O Salt OH OCH3 Erythromycin A A= H H HO H H COOH OH OH H OH OH CH2OH H B = HO H H COOH OH H O HO OH O CH2OH OH OH CH2OH Erythromycin Ethyl Succinate: Mixed double ester pro-drug, one –COOH of succinic acid is esterified to the C-2” OH and the other –COOH is esterified to ethanol. Oral suspension for pediatric use. Some associated cholestatic jaundice. Clarithromycin: C-6 hydroxyl of erythromycin is replaced with a methoxy group. C-6 –OH of erythromycin is involved in the intramolecular ketal formation, one of the breakdown products causing GI cramping. 49 Therefore, clarithramycin is more lipophilic, more stable because it does not form internal ketals and thus less GI upsets. Higher blood levels. Extensive first-pass metabolism to a more potent C-14 hydroxy analog. N(CH3)2 Clarithromycin HO O HO 6 H3CO O O OH O O O OH OCH3 O Azithromycin: Azithromycin (azalide) is formed from a semisynthetic expansion of the ring to a 15-membered structure with an N-methyl inserted between C-9 and C-10 of erythromycin and the carbonyl at C-9 removed. It does not form a cyclic ketal. It is more acid stable than erythromycin and has a longer thus improving compliance. Azithromycin (a 15-membered ring) N(CH3)2 HO H3C N HO 6 H3CO O O OH O O O O 50 OH OCH3 Dirithromycin: Semisynthetic pro-drug that is hydrolyzed to erythomycyclamine which is a semisynthetic active erythromycin analog. N(CH3)2 HO H N H2 H3COH2CH2C O C Dirithromycin 6 H3CO O O O OH O O O OH OCH3 O Metabolism (gut) N(CH3)2 HO H2N HO 6 H3CO O O OH O O O O OH OCH3 51 Erythromycyclamine Miscellaneous Antibiotics Lincosamides (Lincomycin and Clindamycin): They contain an unusual 8-carbon sugar –thiomethylaminooctoside (Othiolincosamine). This 8-carbon sugar is linked via an amide bond to an N-propyl substituted N-methylpyrrolidylcarboxylic acid. Lincosamides are weakly basic forming clinically useful HCl salts. Chemically distinct but pharmacologically similar to the macrolides. Lincomycin is isolated from Streptomyces lincolnensis. It serves as reactant in the synthesis of clindamycin by an SN2 mechanism which changes the C-7 R –OH to a C-7 S-Cl. The lincosamides bind to the 50S ribosomal subparticle that partially overlaps the macrolide binding sites. The macrolides and the lincosamides thus have essentially the same MOA. They also show cross resistance. The clindamycin spectrum is similar to that of macrolides although it penetrates bones better. CH3 CH3 CH3 HO H CH3 H HO NHC HO N O O HO H H SOCl2 Cl NHC HO CH3 O HO OH SCH 3 N O H CH3 OR SCH 3 R=H, Clindamycin R= PO3H, Clindamycin phosphate Lincomycin 52 Chloramphenicol: Originally isolated from Streptomyces venezuelae. Its simple structure resulted in total chemical synthesis. Unwanted diastereomers must be removed from the total synthetic products before use. First oral broad spectrum agent (1947) that was once very popular. Severe potential blood dyscrasia has limited its use in N. America. Rapid and complete oral absorption. Excreted in urine as a C-3 glucuronide conjugate. Deamidation and dehalogenation does occur. Chloramphenicol is bacteriostatic as inhibits protein synthesis in bacteria. It binds on the 50S ribosomal subparticle close to the macrolide binding site. Resistance is mediated by R-factor enzymes that acetylate the side chain – OH groups. The acetylation prevents their binding to the ribosomes. Two prodrug forms are used; the palmitate and the hemisuccinate. The cloramphenicol hemisuccinate improves the poor water-solubility of the drug. The chloramphenicol palmitate is used in suspensions that limits the extremely bitter taste. Cl2HC O H CH2OR C N * H H * OH * Asymmetric carbons, 4 diastereomers only 1R, 2R is significantly active NO2 R= H R= COCH2CH2COOH R= CO(CH2)12CH3 Chloramphenicol Chloramphenicol hemisuccinate Chloramphenicol palmitate 53 Cyclic peptides: Several bacteria species produce antibiotic mixtures of cyclic peptides. These are made with uncommon amino acids as well as the D-isomers of common amino acids. These make them difficult to metabolize. They may have an associated fatty acid. They are water-soluble, and extremely lethal to susceptible bacteria. They attach themselves to the bacterial membranes, disrupt their semipermeability and cause valuable nutrients to leak out and toxic compounds to leak into the bacterial cell. These agents are also toxic to humans thus limiting their use to severe situations with few therapeutic options. Drugs: Vancomycin: Produced by fermenting Nocardia orientalis. One of about 200 glycopeptide antibiotics in clinical use. Useful against Gram (+) bacteria only. Low oral availability. Very irritating on IV administration, so slowly instilled. Despite about 40 years of use, resistance is only becoming apparent. Resistance is due to the conversion of D-Ala-D-Ala units on the peptidoglycan cell wall to D-Ala-D-Lactate units. Vancomycin loses effectiveness due to its greatly diminished affinity for the new linkage. OH H2N OH CH3 HO OH H3 C O O O O Cl O O HO O O HN N H H O H N O N H H2 N HO2C HO O O OH OH Vancomycin 54 OH O H N N H NHC H3 Bacitracin: Mixture of similar peptides from Bacillus subtilis with component A predominating. Named from Bacillus and Tracy, the first person to be treated with it. Mainly active against Gram (+) bacteria. Shows neuro- and nephro-toxicities. Zinc ions enhance its activity. It acts by inhibiting the synthesis of the peptidoglycan chain and disruption of plasma membrane function. CH3 H3C Bacitracin A S H2N N O L-His D-Asp D-Phe L-Ile D-Orn 55 L-Asn L-Lys L-Ile L-Leu D-Glu