* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Antiparasitic Agents
Survey
Document related concepts
Transcript
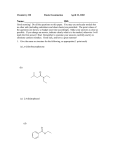
Antiparasitic Agents I. Parasitic Infections a. Spread via travel b. #1 disease is protozoal (malaria) c. General considerations i. Over 1 billion people have a parasitic infection ii. Usually found in developing countries where there is little financial incentive to market new drugs d. Protozoal infections i. Amebiasis 1. An intestinal disease caused by Entamoeba histolytica 2. Found in the US too 3. causes dysentery, diarrhea, nausea, tenderness and enlargement of liver 4. also and extra intestinal form (liver) 5. different forms are transmitted differently a. trophozoid: motile form and a cyst form i. infectious 1. protected fro the environment b. can have carriers ii. Giardiasis 1. an intestinal disease caused by Giardia lambila 2. more common 3. self limiting a. doesn’t need to be treated 4. called backpackers diarrhea 5. carried by wild animals 6. presents as diarrhea and cramps a. the bodies attempt to flush the bug out of the body 7. no extra intestinal form iii. Trichomoniasis 1. a protozoal infection caused by Trichomonas vaginalis 2. common 3. causes vaginitis a. can be many things b. effects the genital/urinary tracts 4. females have symptoms but not the male 5. transmitted through sexual acts 6. over 180 million people world wide have the infection iv. Leshmaniasis 1. very uncommon in the use a. one form: L. Mexicana II. i. Found in Mexico and some parts of Texas 2. Spread by the sand fly 3. It can infect many areas/body parts 4. Cause lesions an death 5. Has an extra intestinal form 6. Symptoms: fever, diarrhea, cough, enlarged liver an s spleen v. Trypanosomiasis 1. systemic protozoal infections caused by Trypanosoma cruzi (American trypanosomiasis or Chigas’ disease) and Trypanosoma bruci (African trypanosomiasis or sleeping sickness) 2. 50 million Africans at risk for developing the disease 3. organism can penetrate into the heart and cause a heart attack 4. spread by tsetse fly in Africa and the kissing bug (Chigas’) vi. Pneumocystis 1. an infection seen in immune compromised individuals caused by Pneumocystis carinii and organism with morphology somewhere between a protozoa and a fungi a. no ergosterol—difficult to classify 2. on of the 3 major secondary disease in immunocompromised patients vii. Malaria 1. a systemic infection caused by any of four Plasmodium a. P. flaciparum (very deadly), P. vivax, P. malariae, or P. ovale b. Most serious world wide disease viii. Cryptosporidiosis 1. parasitic org found in immunocompromised patients Drug therapy for protozoal infections a. Treatment of amebiasis, giardiasis, trichomonias and cryptosporidiosis i. Metronidazole (Flagyl, Metryl, Satric) 1. water soluble 2. HCl salt 3. MOA: Unsure a. May produce a super oxide radical anion (diradical) b. Nitro group picks up an electron and enters the reductive state forming a hydroxyl amine. c. The electron is then transferred to O2 forming a super oxide radical anion who can from a reactive oxygen species such as hydrogen peroxide d. The reactive oxygen species is though to attach to DNA leading to lethal fragmentation of the DNA 4. Metabolism: a. prodrug that under goes hydroxylation (active compound) and then glucuronide conjugation i. Conjugates found in the urine ii. Form off of either alcohol iii. Inactive b. Oxidation to an active compound 5. Therapeutic application a. Resistant strains of amebidisis and trichomonas b. Should not be taken during the 1st trimester i. Carcinogenic/ mutagenic in mice 6. Side effects a. Metallic taste, abdominal pains b. Causes a disulfuram like effect ii. Tinidazole 1. not available in the US 2. derivative of metronidazole iii. Diloxanide furoate (Furamide) 1. available from the CDC 2. under goes degradation in the GI tract to form Diloxanide (active compound) 3. metabolized to the glucuronide (inactive) 4. prescribed for asymptomatic amebiasis a. not useful for extraintestinal amebiasis iv. Nitazoxahide (Alina) 1. prodrug 2. appeared a few weeks ago 3. not carcinogenic or mutogenic 4. the nitro group is important for activity a. required fro the redox reactions 5. thiazole 6. used against a. G. intestinalis and T. vaginalis which are resistant to metrondiazole b. E. histolytica c. Cryptosporidium parvum d. H. Pylori e. And some helminthes 7. MOA: nitazoxahide and Tizoxanide (active compouind) are prodrugs which are activated by electron transfers from PFOR (pyruvate: ferredoxin oxido reductase) a. Effects NADH III. IV. b. Essential for anaerobic energy metabolism (an electron transfer reaction) 8. Tizoxanide is further conjugated with glucuronide to an inactive compound 9. Both nitazoxahide and tizoxanide have an NO2 Treatment of leishmaniasis a. Sodium stilbogluconate (pentostam) i. Available from the CDC ii. Diglucuronic with heavy metal 1. Sb = antimony 2. increases the affinity for sulfhydro groups 3. not very selective for pathogenic organisms iii. MOA: unknown, but it may inhibit (up to 90%) glucose catabolism resulting in decreased levels of ATP and GTP b. Pentamidine i. See below Treatment of pneumocystis (PCP) a. Common in immunocompromised b. Has no ergosterol so it is not a true fungus c. Sulfamethoxazole/trimethoprim (Bactrim, Septra) i. Interferes with THF reduction ii. DDS + trimethoprim interferes with PABA incorporation 1. used as a backup d. Pentamidine (Pentam 300 and Nebupent) i. Binds to the AT regions in DNA and inhibits Type 2 topoisomerase in mitochondria DNA 1. H-bonds to DNA 2. cross links the two strands so that they cannot unwind 3. the amidine group donates reacts with the extra electrons on the nitrogen ii. available IV or aerosol 1. good since PCP is a lung condition iii. 50% of patients on IV have toxic reactions 1. correlates to the rate of injection 2. breathlessness, tachycardia, dizziness 3. may be due to histamine release iv. poor CNS penetration v. high water solubility e. Atovaquone (Mepron) i. Used as a back up drug ii. Inhibits mitochondrial respiratory chain 1. ubiquinone reductase inhibitor V. a. important for electron transport and may be cytochrome BC1 iii. administered orally iv. poor absorption 1. better when administered with a fatty meal v. highly bound to plasma protein vi. excreted unchanged Treatment of Trypanosomiasis a. Suramin sodium i. Introduced in the 1020’s ii. Drug of choice for non CNS African trypanosomiasis iii. MOA: none proven 1. Inhibits dihydrofolate reductase 2. Inhibits thymidine kinase 3. Inhibits glycolytic enzymes iv. Water soluble v. Poorly absorbed vi. Given IV vii. Does not cross the blood brain barrier 1. limits used b/cause you can’t treat the active from of the disease viii. bound to plasma protein ix. prophylactic b. Pentamidine i. Used for east African sleeping sickness ii. Useful only in the early stages of the disease iii. Does not penetrate the BBB c. Eflornithine (Ornidyl, DFMO) i. Derivate of ornithine 1. ornithine normally is decarboxylated by ornithine decarboxylase to purtrescine and then spermine which leads to cell division ii. a poly-amine iii. forms a Schiff base iv. MOA: competes for ornithine decarboxylase 1. irreversible 2. yields a loss of HF 3. ODC attacks at the CHF of a decarboxylated compound causing the loss of the last F then it cleaves the pyridoxyl-5phosphate and permanently attaches so the enzyme can not carry out it’s proper reaction v. Suicide substrate VI. vi. Human cells can produce ODC rapidly but the bug can not so the drug has somewhat selective effects vii. Poor oral absorption viii. Zwitterionic ix. Given IV and PO x. Specturm of activity 1. Tb. gambinese a. Early and late 2. not effective against Tb. rhodesiense d. Nifurtimox i. Available from CDC ii. Contains a nitrofuran iii. MOA: generate ractive oxygen species 1. NO2 is the source of the electrons that it transfers to the O2 2. Damages lipid portion of the cell membrane 3. damages the DNA 4. inhibits trypanothione reductase iv. Drug of choice for Chigas’ disease (acute) e. Melarsoprol i. Available from the CDC ii. Has arsenic at the center of the compound iii. Developed in the 1040s iv. MOA: As has high affinity for sulf hydrol groups present in several key trypanosoma enzymes 1. trapanothione reductase 2. pyruvate kinase 3. phosphofructokinase v. administered IV vi. poorly absorbed vii. enters the CNS viii. drug of choice for late stage menigoencephalitic trypanosomasis 1. active against Tb. rhodesiense and Tb. gambinese ix. very serious side effects 1. 3-5% death 2. convulsions, cerebral edema, coma and encephalopathy Malaria a. Patients are non symptomatic when the bug is in the liver (Preerythrocytic stage) b. 300-500 million people have a clinical case of malaria c. 1.5-2.5 million deaths per year d. only the female mosquito bites e. disease foun di n all warmblooded animals f. difficult to control g. Tertian or quatrain malaria i. the symptoms occur every 3rd or 4th day h. Drugs: i. Quinine 1. original compound 2. entered into the London Pharmacopia about 1677 3. used the bark of the cincona tree 4. resistance has developed 5. developed quinacrine in 1934 a. closely related to quinine 6. chloroquine is the mainstay of treatment today a. the best anti-malarial b. developed in the 1940’s 7. quinoline nucleus is important for the compound 8. MOA: a. intercalculation into DNA i. Requires a flat molecule ii. Dose needed is much higher than the therapeutic dose iii. Probably not the MOA b. Ferriprotoporphyrin iX (FP9) i. Very possible ii. Because plasmodium degrades erythrocytes for amino acids iii. Also produces hemozin (contains FP9) 1. very toxic except when bound to protein iv. chloroquin can also bind (very toxic) c. weak base hypothesis i. plasmodium lysosome pka is about 4.8 – 5.2 ii. anti malarial forms salt and increases the pH iii. plasmodium’s digestion of the hemoglobin is diecreased iv. reasonable MOA 9. Resistance a. Increased drug efflux b. Increased Cyp 450 activity 10. Threepudic Application a. Active against erythrocytic plasmodium i. Erythrocytic schizonticide ii. Quinine 1. metabolized via Cyp 3A4 to a di-hydroxyl compound with poor activity iii. Choloroquine (Aralen) iv. v. vi. vii. viii. 1. metabolized via dealkalytion via CYP 450 to an active compound Mefloquine (Lariam) 1. CF3 protects against metabolism (bug can’t hydrolyze) 2. derivative of quinine 3. effective against resistant strains 4. suppressive prophylactic 5. has neuro-psychiatric side effects as well as GI disturbances, cardiovascular and skin effects 6. Metabolsim: the alchohol is oxidized and converted to a ketone and then COOH a. Inactive Halofantrine (Halfan) 1. metabolized via dealkylation to the active agent a. removal of a butyl group 2. good for resistant organisms 3. back up agent 4. useful for cholorquine resistant P. falciparius 5. Side effects: lengthens the QT interval Pyrinethamine (Daraprim, Fansidar) 1. contains a sulfer drug (Fansidar) 2. structure is similar to trimethoprim 3. inhibits DHF reductase and THFA synthesis 4. used in combination with sulfa drugs a. sequential blocking Proguanil 1. prodrug that undergoes oxidation and cyclization to cycloguanil (active) 2. similar to trimethoprim a. not an aromatic ring 3. melarone = Atovaquone an dProguanil 4. erytholytic shizontacide Artemisinin 1. started as a natural product a. all have an O-O peroxide 2. not on the market yet 3. kills through free radical oxidative mechanism a. membrane oxidation 4. therapeutic application: gametocytocidal agent a. prevents the spread of the disease