Click here for handout
... cannabis dependence. Symptoms were treated with SSRIs, but discontinued secondary to “activation.” • Physical exam WNL. Labs positive for cannabis. ...
... cannabis dependence. Symptoms were treated with SSRIs, but discontinued secondary to “activation.” • Physical exam WNL. Labs positive for cannabis. ...
Psychological Disorders
... accumulated from gambling. He also has been feeling extreme pressure about not being able to take care of his eight children. After having too much to drink, Carson ran over a child crossing the street. Immediately following this episode, Carson could not remember who he was. This ...
... accumulated from gambling. He also has been feeling extreme pressure about not being able to take care of his eight children. After having too much to drink, Carson ran over a child crossing the street. Immediately following this episode, Carson could not remember who he was. This ...
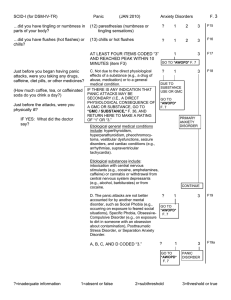
SCID-I (for DSM-IV-TR) Panic (JAN 2010) Anxiety Disorders F. 3
... 4 - In Partial Remission: The full criteria for the disorder were previously met but currently only some of the symptoms or signs of the disorder remain. 5 - In Full Remission: There are no longer any symptoms or signs of the disorder, but it Is still clinically relevant to note the disorder--for ex ...
... 4 - In Partial Remission: The full criteria for the disorder were previously met but currently only some of the symptoms or signs of the disorder remain. 5 - In Full Remission: There are no longer any symptoms or signs of the disorder, but it Is still clinically relevant to note the disorder--for ex ...
Borderline personality disorder, bipolar disorder
... months, combined with consistent daily fluctuations of symptoms—the patient feeling worse in the mornings and mood improving gradually every evening, with a relentless repetitiveness of such daily cycles over weeks—characterizes a typical major depressive episode. "While it may be clear that these s ...
... months, combined with consistent daily fluctuations of symptoms—the patient feeling worse in the mornings and mood improving gradually every evening, with a relentless repetitiveness of such daily cycles over weeks—characterizes a typical major depressive episode. "While it may be clear that these s ...
ANXIETY DISORDERS
... Biological pathways Major anxiety disorders: development & treatment Post Traumatic Stress Disorder ...
... Biological pathways Major anxiety disorders: development & treatment Post Traumatic Stress Disorder ...
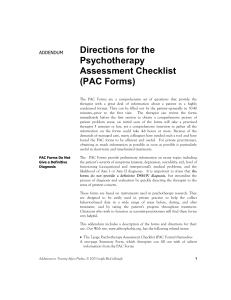
PAC Forms - Affect Phobia Therapy
... discussed in Chapter 3) Axis II criteria are the behavioral embodiments of defensive functioning. Axis II items must change if personality disorders are to be resolved. Items marked “yes” on this form alert you very quickly to the type of defensive functioning that will need further exploration. For ...
... discussed in Chapter 3) Axis II criteria are the behavioral embodiments of defensive functioning. Axis II items must change if personality disorders are to be resolved. Items marked “yes” on this form alert you very quickly to the type of defensive functioning that will need further exploration. For ...
Screening, Referral and Treatment for Attention Deficit and Hyperactivity
... Attention Deficit Hyperactivity Disorder, originally thought to occur just in childhood, is now widely understood as persisting into adulthood. Between 50 to 65 percent of adults diagnosed with childhood ADHD will continue to have symptoms of inattention, distractibility and impulsivity causing func ...
... Attention Deficit Hyperactivity Disorder, originally thought to occur just in childhood, is now widely understood as persisting into adulthood. Between 50 to 65 percent of adults diagnosed with childhood ADHD will continue to have symptoms of inattention, distractibility and impulsivity causing func ...
DSM-5: Implications for Social Work Practice Latino Social Work Organization October 16, 2014
... • There are no repetitive patterns or restricted interests (i.e. criteria for ASD would not be met). • Language impairment is a common associated feature as is ADHD, behavior problems and specific learning disorders. Family history of ASD, LD or communication disorder increases the risk for social c ...
... • There are no repetitive patterns or restricted interests (i.e. criteria for ASD would not be met). • Language impairment is a common associated feature as is ADHD, behavior problems and specific learning disorders. Family history of ASD, LD or communication disorder increases the risk for social c ...
Eating Disorders
... Visiting the bathroom immediately after meals. This is often a sign that the person is planning to induce vomiting. Practicing strict weight-loss programs followed by eating binges. Excessive exercise. ...
... Visiting the bathroom immediately after meals. This is often a sign that the person is planning to induce vomiting. Practicing strict weight-loss programs followed by eating binges. Excessive exercise. ...
Lundbeck Institute Campus Slide deck library
... (1) WHO. Global burden of mental disorders and the need for a comprehensive, coordinated response from health and social sectors at the country level. 2011. Retrieved from: http://apps.who.int/gb/ebwha/pdf_files/EB130/B130_9-en.pdf. Accessed April 2016; (2). WHO The Global Burden of Disease 2004 Upd ...
... (1) WHO. Global burden of mental disorders and the need for a comprehensive, coordinated response from health and social sectors at the country level. 2011. Retrieved from: http://apps.who.int/gb/ebwha/pdf_files/EB130/B130_9-en.pdf. Accessed April 2016; (2). WHO The Global Burden of Disease 2004 Upd ...
PROLONGED GRIEF DISORDER IN THE DSM-V - trauma-ptsd
... disorders such as emotional numbing (posttraumatic stress disorder; PTSD) and a diminished sense of self (major depressive disorder; MDD), PGD sufferers would be overlooked or “forced” into an inappropriate diagnostic category if they were assessed using only psychiatric disorders that are presently ...
... disorders such as emotional numbing (posttraumatic stress disorder; PTSD) and a diminished sense of self (major depressive disorder; MDD), PGD sufferers would be overlooked or “forced” into an inappropriate diagnostic category if they were assessed using only psychiatric disorders that are presently ...
Cluster B – Borderline
... Age: Personality disorders generally should not be diagnosed in children and adolescents because personality development is not complete and symptomatic traits may not persist into adulthood. Therefore, the rule of thumb is that personality diagnosis cannot be made until the person is at least 18 ...
... Age: Personality disorders generally should not be diagnosed in children and adolescents because personality development is not complete and symptomatic traits may not persist into adulthood. Therefore, the rule of thumb is that personality diagnosis cannot be made until the person is at least 18 ...
Borderline Personality Disorder: Podcast Script #1 A personality
... A personality disorder can best be described as behavior that is very different from what is considered “normal” for one’s culture (American Psychiatric Association [DSM-IV-TR], 2000). Personality disorders are stable over time, usually cause great distress or impairment to those affected, and typi ...
... A personality disorder can best be described as behavior that is very different from what is considered “normal” for one’s culture (American Psychiatric Association [DSM-IV-TR], 2000). Personality disorders are stable over time, usually cause great distress or impairment to those affected, and typi ...
Mood Disorders: An overview
... psychomotor symptoms, from motoric immobility as well as mutism and rigidity. Catatonic features are very common with ...
... psychomotor symptoms, from motoric immobility as well as mutism and rigidity. Catatonic features are very common with ...
Premenstrual Dysphoric Disorder (PMDD)
... Although the mood symptoms associated with PMS sound similar to PMDD, they are different in one key respect: PMDD is much more severe. Premenstrual dysphoric disorder should be diagnosed only when mood symptoms seriously impact relationships and impair functioning at work or school. Depending on how ...
... Although the mood symptoms associated with PMS sound similar to PMDD, they are different in one key respect: PMDD is much more severe. Premenstrual dysphoric disorder should be diagnosed only when mood symptoms seriously impact relationships and impair functioning at work or school. Depending on how ...
Eating Disorders and Trauma
... This Research was conducted in response to Briere’s and Corstophine’s work mainly concerned about the interaction between adverse childhood experiences and eating disorder behaviors. In the first article, Brewerton (Levitt’s assistant) provides a review of the comorbidity between eating disorders an ...
... This Research was conducted in response to Briere’s and Corstophine’s work mainly concerned about the interaction between adverse childhood experiences and eating disorder behaviors. In the first article, Brewerton (Levitt’s assistant) provides a review of the comorbidity between eating disorders an ...
Bipolar disorder, also known as manic
... blues” when it is short-lived but is termed “dysthymia” when it is chronic.Then there is normal or balanced mood, above which comes hypomania (mild to moderate mania), and then severe mania. In some people, however, symptoms of mania and depression may occur together in what is called a mixed bipola ...
... blues” when it is short-lived but is termed “dysthymia” when it is chronic.Then there is normal or balanced mood, above which comes hypomania (mild to moderate mania), and then severe mania. In some people, however, symptoms of mania and depression may occur together in what is called a mixed bipola ...
this PDF file - Journal of Research and Practice in K
... internalizing symptoms. Internal states of excessive fear and anxiety and resulting behavioral changes are characteristic of Anxiety Disorders. The focus of this category is on the emotional fear response to real or perceived imminent threat or the anticipation or anxiety of future threat. These fea ...
... internalizing symptoms. Internal states of excessive fear and anxiety and resulting behavioral changes are characteristic of Anxiety Disorders. The focus of this category is on the emotional fear response to real or perceived imminent threat or the anticipation or anxiety of future threat. These fea ...
Substance Use and Schizophrenia | Schizophrenia Society
... ubstance use complicates the course of illness and the treatment of people with schizophrenia, even when relatively small amounts of substances are used. The misuse of substances adversely affects the medication taken for psychiatric symptoms, and can exacerbate all the symptoms. People in treatment ...
... ubstance use complicates the course of illness and the treatment of people with schizophrenia, even when relatively small amounts of substances are used. The misuse of substances adversely affects the medication taken for psychiatric symptoms, and can exacerbate all the symptoms. People in treatment ...
Personality Disorders
... Low-dose antipsychotics have been used for borderline and schizotypal personalities. They have been shown to be effective in symptom control in double-blind studies, though they may not help deeper problems with personal relations. The benefits of these drugs must be balanced against the risk of tar ...
... Low-dose antipsychotics have been used for borderline and schizotypal personalities. They have been shown to be effective in symptom control in double-blind studies, though they may not help deeper problems with personal relations. The benefits of these drugs must be balanced against the risk of tar ...
Dissociative Identity Disorder handout
... bipolar disorder, because “switching” can look like rapid-cycling mood swings; schizophrenia or psychoses, because flashbacks can cause auditory and visual hallucinations; and addictions, because alcohol and drugs are frequently used to self medicate or to numb the psychic pain. Q: What Other Mental ...
... bipolar disorder, because “switching” can look like rapid-cycling mood swings; schizophrenia or psychoses, because flashbacks can cause auditory and visual hallucinations; and addictions, because alcohol and drugs are frequently used to self medicate or to numb the psychic pain. Q: What Other Mental ...
PARTICIPANT HANDOUT Introduction The term "comorbidity" refers
... because of its frequency and because of its impact. Some psychiatric illnesses serve as risk factors for alcohol use disorders, and others may develop as a result of chronic alcohol use/abuse. However, they do have the power to alter significantly the course and treatment outcomes related to alcohol ...
... because of its frequency and because of its impact. Some psychiatric illnesses serve as risk factors for alcohol use disorders, and others may develop as a result of chronic alcohol use/abuse. However, they do have the power to alter significantly the course and treatment outcomes related to alcohol ...
Ch8
... Criteria 1: Major depressive episode • Marked by five or more symptoms lasting two or more weeks • In extreme cases, symptoms are psychotic, including • Hallucinations ...
... Criteria 1: Major depressive episode • Marked by five or more symptoms lasting two or more weeks • In extreme cases, symptoms are psychotic, including • Hallucinations ...
Schizoaffective disorder

Schizoaffective disorder (abbreviated as SZA or SAD) is a mental disorder characterized by abnormal thought processes and deregulated emotions. The diagnosis is made when the patient has features of both schizophrenia and a mood disorder—either bipolar disorder or depression—but does not strictly meet diagnostic criteria for either alone. The bipolar type is distinguished by symptoms of mania, hypomania, or mixed episode; the depressive type by symptoms of depression only. Common symptoms of the disorder include hallucinations, paranoid delusions, and disorganized speech and thinking. The onset of symptoms usually begins in young adulthood, currently with an uncertain lifetime prevalence because the disorder was redefined, but DSM-IV prevalence estimates were less than 1 percent of the population, in the range of 0.5 to 0.8 percent. Diagnosis is based on observed behavior and the patient's reported experiences.Genetics, neurobiology, early and current environment, behavioral, social, and experiential components appear to be important contributory factors; some recreational and prescription drugs may cause or worsen symptoms. No single isolated organic cause has been found, but extensive evidence exists for abnormalities in the metabolism of tetrahydrobiopterin (BH4), dopamine, and glutamic acid in people with schizophrenia, psychotic mood disorders, and schizoaffective disorder. People with schizoaffective disorder are likely to have co-occurring conditions, including anxiety disorders and substance use disorder. Social problems such as long-term unemployment, poverty and homelessness are common. The average life expectancy of people with the disorder is shorter than those without it, due to increased physical health problems from an absence of health promoting behaviors including a sedentary lifestyle, and a higher suicide rate.The mainstay of current treatment is antipsychotic medication combined with mood stabilizer medication or antidepressant medication, or both. There is growing concern by some researchers that antidepressants may increase psychosis, mania, and long-term mood episode cycling in the disorder. When there is risk to self or others, usually early in treatment, brief hospitalization may be necessary. Psychiatric rehabilitation, psychotherapy, and vocational rehabilitation are very important for recovery of higher psychosocial function. As a group, people with schizoaffective disorder diagnosed using DSM-IV and ICD-10 criteria have a better outcome than people with schizophrenia, but have variable individual psychosocial functional outcomes compared to people with mood disorders, from worse to the same. Outcomes for people with DSM-5 diagnosed schizoaffective disorder depend on data from prospective cohort studies, which haven't been completed yet.In DSM-5 and ICD-9 (which is being revised to ICD-10, to be published in 2015), schizoaffective disorder is in the same diagnostic class as schizophrenia, but not in the same class as mood disorders. The diagnosis was introduced in 1933, and its definition was slightly changed in the DSM-5, published in May 2013, because the DSM-IV schizoaffective disorder definition leads to excessive misdiagnosis. The changes made to the schizoaffective disorder definition were intended to make the DSM-5 diagnosis more consistent (or reliable), and to substantially reduce the use of the diagnosis. Additionally, the DSM-5 schizoaffective disorder diagnosis can no longer be used for first episode psychosis.