* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The Heart Chambers and Valves Of the cardiac chambers, only the
Cardiovascular disease wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Rheumatic fever wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Artificial heart valve wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
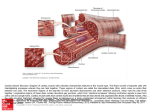
The Heart Chambers and Valves Of the cardiac chambers, only the main parts of the atria have a smooth wall. In the auricles (parts of the atria) and especially in the ventricles, muscular ridges (trabeculae carneae) protrude into the chambers. A single layer of epithelium (endocardium) covers all the chambers. The four valves of the heart are anchored in dense fibrous connective tissue rings that lie nearly in a plane (Fig. 5.5). Together with the connective tissue between them they form a unit, the so-called cardiac skeleton, to which the atria are separated from the ventricles above and below the skeleton. The cusps of the valves between the atria and ventricles (atrioventricular valves) arise as double layers of endocardium from the cardiac skeleton (Fig. 5.5).The free ends of the valve cusps are attached by tendinous threads (chordae tendineae) to the papillary muscles. These cone-shaped processes on the inner ventricular walls, together with the chordae tendineae, prevent the cusps from flapping back during ventricular contractions (Figs. 10a, b). A valve with three cusps (tricuspid valve) is situated between the right atrium and the right ventricle. A valve with two cusps (bicuspid valve, mitral valve) separates the left atrium and left ventricle (Fig. 5.6). The semilunar valves are situated at the entrances to the pulmonary artery and the aorta. They prevent the blood from flowing back after a completed ventricular contraction (Fig. 3). The pulmonary and aortic valves consist of three pockets of duplicated endocardium that project into the lumen with their inferior surfaces directed toward the heart. When the margins of the semilunar valves are tightly apposed, the corresponding exit valve is closed. As the pressure in the ventricles increases, the margins of the semilunar valves draw apart, and the exit valve opens. 8 Cardiovascular System Lecture No; 2 Dr. Abdul-Majeed Alsaffar Wall of the Heart. The heart wall consists of three layers of different thickness and structure (Fig. 5.7): an inner serous coat (endocardium) the actual cardiac muscle (myocardium) an outer serous coat (epicardium) Between the epicardium and the inner side of the pericardium lies a thin serous cavity, scantily filled with fluid, which allows the frictionless movement of the heart in the pericardial sac. The myocardium consists of striated cardiac muscle and is about 0.7 cm thick in the right ventricle. The wall of the left ventricle about 1.4 cm in thickness, because of its higher pressure and the consequently increased load, averages. Differences between Cardiac and Skeletal Muscle The cardiac-muscle cells of the myocardium are arranged in layers that are tightly bound together and completely encircle the blood-filled chambers. When the walls of a chamber contract, they come together like a squeezing fist and exert pressure on the blood they enclose. Cardiac muscle combines properties of both skeletal and smooth muscle. The cells are striated (Figure11) as the result of an arrangement of thick myosin and thin actin filaments similar to that of skeletal muscle. Cardiac-muscle cells are considerably shorter than skeletal muscle fibers, however, and have several branching processes. Adjacent cells are joined end to end at structures called intercalated disks, within which are desmosomes that hold the cells together and to which the myofibrils are attached. Adjacent to the intercalated disks are gap junctions, similar to those in many smooth muscles. Approximately 1 percent of the cardiac-muscle cells does not function in contraction, but have specialized features that are essential for normal heart excitation. These cells constitute a network known as the conducting system of the heart and are in contact with the other cardiac-muscle cells via gap junctions. The conducting system initiates the heartbeat and helps Cardiovascular System Lecture No; 2 9 Dr. Abdul-Majeed Alsaffar spread the impulse rapidly throughout the heart. A single adequate stimulus for action potential in one myocyte results in the rapid spread of excitation to all myocytes via gap junctions. This is known as the all-or-none electrical response of the heart. One final point about the cardiac-muscle cells in the atria, are certain cells when they become stretched, secrete the family of peptide hormones collectively called atrial natriuretic factor. (ANF):During heart failure almost always excessive increase in both right left atrial pressure causing their wall stretch, the circulating levels of ANF in the blood increase from fivefold to tenfold in sever heart failure. The ANF in turn has a direct effect on kidneys to increase greatly their excretion of salt and water. Therefore, ANF plays a natural role to help prevent extreme congestive symptoms during cardiac failure. Fig.11 a−c Muscle tissue in longitudinal section a Smooth muscle tissue b Striated (skeletal) muscle c Cardiac muscle The Coronary Vessels The coronary arteries supply the heart muscle exclusively (Fig. 5.9). They arise from the aorta immediately above the aortic valve and send their major branches over the myocardium, their terminal branches entering the cardiac muscle from the outside. After leaving the aorta, the right coronary artery runs in the coronary sulcus, at first under the right auricle, then around the right cardiac border toward the diaphragmatic surface of the heart. It ends in the posterior interventricular branch, which runs to the apex of the heart (Fig. 5.9). The left coronary artery, after a short course, divides into two braches the anterior inter ventricular branch, which runs over the anterior surface, and the circumflex branch, which runs posteriorly. The veins collect the blood in the small, middle, and great cardiac veins, which collect in the coronary sinus and drain into the right atrium. If the coronary arteries narrow (arteriosclerosis), the affected cardiac muscle 10 Cardiovascular System Lecture No; 2 Dr. Abdul-Majeed Alsaffar suffers from lack of oxygen and can die (cardiac infarct) if the vessel is totally occluded. 11 Cardiovascular System Lecture No; 2 Dr. Abdul-Majeed Alsaffar References 1. Textbook of Medical Physiology 11th, Edition .by Guyton A.C. 2. Human Physiology The Basis of Medicine 2nd, Edition. by Gillian Pocock and Christopher D.R. 3. Human Physiology: The Mechanism of Body Function 10th Edition. by Vander, et al 12 Cardiovascular System Lecture No; 2 Dr. Abdul-Majeed Alsaffar