* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pyrexia of unknown origin
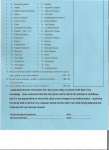
West Nile fever wikipedia , lookup
Hepatitis B wikipedia , lookup
Epidemiology of HIV/AIDS wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Tuberculosis wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Neonatal infection wikipedia , lookup
Orthohantavirus wikipedia , lookup
Oesophagostomum wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Yellow fever wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
1793 Philadelphia yellow fever epidemic wikipedia , lookup
Marburg virus disease wikipedia , lookup
Typhoid fever wikipedia , lookup
Diagnosis of HIV/AIDS wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Yellow fever in Buenos Aires wikipedia , lookup
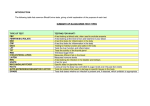
Pyrexia of unknown origin and Fever in returning traveller Dr Richard Drew Research Fellow Dept Clinical Microbiology What is PUO Originally defined in 1961 by Petersdorf and Beeson Fever >38.3C on 3 or more occasions Fever for more then three weeks Uncertain diagnosis after one week in hospital Very rare nowadays in hospital How to solve the problem History Physical examination Blood tests Imaging Endoscopy and tumour markers Aetiology 1. 2. 3. Infections Malignancies Connective tissue disorders History Fever: Pattern, periodicity, how was it measured Associated symptoms such as sweating, vomiting, headaches etc. Target specific organ systems if patient has problems in that system Past med and surg hx. NB prostheses in situ Medications/ vaccines Family hx of hereditary diseases, connective tissue disorders or recent illnesses (TB/ AIDS) Sexual history Occupation, pets, travel Examination Full physical examination is needed. Should be very detailed and review all systems. For exams make sure to examine: Hands for stigmata of infective endocarditis Retinal exam for candidiasis or toxoplasmosis Teeth (infective endo or abscess) Lymphadenopathy (AIDS or chronic infections) Hepatosplenomegaly (Lymphoma/leukaemia) Breast/testicular exams Any sore joints Infections Tuberculosis HIV/AIDS Abscess Osteomyelitis Infective Endocarditis tuberculosis Classical prevention is fever, haemoptysis, cough, weight loss and night sweats Risk Factors: Alcoholic, homeless, drug abuser, immigrant On exam can have pleural rub, pleural effusion and lymphadenopathy. Check if BCG vaccinated Do Mantoux test, CXR and sputum for AFB and TB culture. Treatment is 4 drug regimen (RIPE) and inform public health Isolate patient for 2 weeks in negative pressure room and wear FFP3 masks Always consider in differential of patient with cough and PUO HIV/ AIDS No classical presentation. Can present with fever, weight loss, sweats, lymphadenopathy or with opportunistic infection Hx: Sexual contacts, Birthplace, Maternal hx if child, Exposure events, occupation O/E Full exam. Lymph nodes and spleen Ix: HIV antibody test and HIV viral load, CD4 count Mx: Refer to ID team. HAART Osteomyelitis Infection of the bone Spontaneous osteomyelitis is rare apart from in Sickle cell disease patients Consider if prosthesis is in situ or if there is a history of preceeding compound fractures FBC, ESR, Imaging of joint, bone biopsy Mx: Targeted antimicrobial therapy and prosthesis removal Non-infectious causes Malignancies Lymphoma Leukaemia Solid organ tumours Connective tissue disorders Still’s disease Giant cell arteritis Malignancies Leukaemia/Lymphoma Solid Organ tumours Hx: fever, sweats, weight loss, fatigue O/E, Lymph nodes, hepatosplenomegaly Ix: Bone Marrow aspirate, blood smear, FBC Mx: Chemotherapy+/- Bone Marrow transplant Target the particular organ you feel is involved. Connective tissue disorders Hx: Fatigue, unexplained rashes, arthralgia, myalgia O/E arthralgia, uveitis, Raynaud’s phenomenon Ix: ESR Mx: Steroids, NSAIDs Investigations Basic tests FBC: WCC, blood smear, bone marrow aspirate ESR, CRP: Non-specific markers of inflammation CXR, Mammogram, Pap smear if relevant, Mantoux, Micro: Blood cultures (3 sets) Other tests to consider The clue is in the history as to what tests are needed HIV test, viral and bacterial serology CT thorax/ abdomen Tumour markers Echocardiogram Management Determine if critically ill. If not can hold off on antibiotics Don’t feel need to just treat a temperature Clue is in the history and the exam and then order relevant tests. Do not send random serological tests off. Often these will cause more trouble then you want!!! Returning Traveller Very common problem Geosentinel data review (Clin Infect Dis. 2007) of 25,000 ill returning travellers 28% had fever and 26% of these needed admission Malaria was the most common diagnosis Considerable geographical variation 17% had vaccine preventable diseases Will discuss methods of diagnosing the condition and not each disease in detail History Crucial. Will help to narrow down possible list of diseases. Don’t always get distracted by history of recent travel. May be more common diagnosis Exposure: Duration, exact location, urban/rural, type of accomadation Timing: Consider incubation period and onset of symtoms. 66% of dengue presents within one week of return. 34% of hepA presents within 6 weeks Food history is important Sexual history is important Vaccine history Examination Full examination as per previous PUO talk Need to consider the risk of a transmissible organism Consider isolating patient until diagnosis is known Critical if considering a viral haemorrhagic fever Signs that should trigger full resuscitation and precautions Bleeding symptoms, respiratory symptoms Hypotension Signs of meningitis or raised intracranial pressure Evaluation Thick and Thin smears for malaria FBC: Look for raised white cells Renal profile: Dehydration, renal failure Liver profile: hepatitis Coagulation screen CXR if respiratory symptoms Top 5 diagnoses (Geosentinel) 1. 2. 3. 4. 5. Malaria Dengue Fever EBV/CMV mononucleosis Rickettsia Typhoid Clinical Case 1 26yr IVDA from Dublin Self discharged twice before from hospital having been admitted with fever Reports to have had fever and night sweats for about 4 weeks. Has lost 2 stone in 3 months Some visible skin sores and needle marks Pulse 110bpm, Temp 36C, BP 100/60 Differential diagnosis History Examination Lab tests at 3am Lab tests the following day Infection Control Management Public Health Clinical Case 2 Returning GOAL worker. 28 yr male. Worked for 12 months in rural clinic in Rwanda 2 episodes of infectious diarrhoea while there Presented to ED three days after coming home Looks very unwell. Non blanching skin rash Differential diagnosis History Examination Lab tests at 3am Lab tests the following day Infection Control Management Public Health