* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Lecture_05_The mostly spread congenital heart diseases in
Survey
Document related concepts
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Aortic stenosis wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
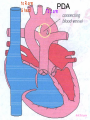
Congenital Heart Disease Prof. Pavlyshyn H.A. Congenital heart disease (CHD) – general points is a defect in the structure of the heart and great vessels which is present at birth • CHD are the main cause of defect-related deaths • Incidence is 8-9/1000 live births • More common in premature infants • May be associated with a significant musculoskeletal defect (e.g. diaphragmatic hernia, exomphalos, tracheo-oesophageal fistula, imperforate anus) Congenital heart disease (CHD) • Causes are multifactorial and include maternal illness (diabetes mellitus, phenylketonuria, and systemic lupus erythematosus), maternal infections (Rubella), drugs (lithium, thalidomide), known teratogens, harmful habits (alcohol, hydantoin) and associations with chromosomal abnormality or other recognized patterns of malformation or syndrome; Trisomy 18 100% have CHD Evaluation of the newborn Recognition of Cyanosis • Cyanosis = blue color of skin and mucous membranes caused by reduced oxygen content • oxygen content of blood depends upon: Hgb level oxygen saturation blood flow • cyanosis usually noted when Sat’s <86% • cyanosis more easily seen in polycythemia • cyanosis more difficult to see in anemia • Acrocyanosis vs. central cyanosis Recognition of Cyanosis Central cyanosis • noted in the trunk, tongue, mucous membranes • due to reduced oxygen saturation Peripheral cyanosis • noted in the hands and feet, around mouth • due to reduced local blood flow Recognition of Cyanosis Differential cyanosis 1. pink upper, blue lower CoA (Coarctation of the aorta), IAA (Interrupted aortic arch), Pulm Htn 2. blue upper, pink lower Transposition of the great vessels d-TGA with pulm Htn dextro-Transposition of the great arteries *indicates serious underlying cardiac or lung disease* Chest Radiograph may be helpful The following lesions present with reduced pulmonary vascular markings • • • • • Tetralogy of Fallot (TOF) • Pulmonary atresia • Tricuspid atresia • Critical pulmonary stenosis The following lesions present with increased pulmonary vascular markings on chest X-ray • • VSD, Transposition of the great arteries (TGA) • • Truncus arteriosus • • Total anomalous pulmonary venous drainage (TAPVD) A 15-year-old girl with short stature, neck webbing, and sexual infantilism is found to have coarctation of the aorta. A chromosomal analysis likely would demonstrate which of the following? • • • • • a. Mutation at chromosome 15q21.1 b. Trisomy 21 c. XO karyotype d. Defect at chromosome 4p16 e. Normal chromosome analysis Acyanotic Congenital Heart Disease ↑ Pulmanary blood flow • • • • Left-to-Right Shunt Lesions Patent Ductus Arteriosus (PDA) Atrial Septal Defect (ASD) Ventricular Septal Defect (VSD) Atrioventricular Septal Defect (AV Canal) Patent Ductus Arteriosus • PDA – Persistence of the normal fetal vessel that joins the PA to the Aorta. • Normally closes in the 1st wk of life. • Female:Male ratio of 2:1 • Often associated w/ coarctation & VSD. to R arm & head To L arm MHMC PDA ligation Patent Ductus Arteriosus Hemodynamics • As a result of higher aortic pressure, blood shunts L to R through the ductus from Aorta to PA. Patent Ductus Arteriosus Clinical Signs & Symptoms • tachycardia • respiratory problems shortness of breath • Poor growth • Differential cyanosis cyanosis of the lower extremities but not of the upper body. Patent Ductus Arteriosus Clinical Signs & Symptoms • Characteristic systolicdiastolic murmur at the base of the heart with maximum in the PA • It localized to the 2nd left intercostal space or radiate down the left sternal border or to the left clavicle. Patent Ductus Arteriosus Clinical Signs & Symptoms • Classic continuous machine-like murmur • It begins soon after onset of the 1st sound, reaches maximal intensity at the end of systole, and wanes in late diastole. • prominent apical impulse enlarged heart, • Left subclavicular thrill • Bounding pulse • Widened pulse pressure Chest X-ray • pulmonary vascularity is increased; • • enlargement of left sided heart Patent Ductus Arteriosus Treatment • Indomethacin - can be used in premature infants (0.2 mg/kg) • Ibuprofen -10-5-5 mg\kg • PDA requires surgical or catheter closure. • Closure is required treatment heart failure & to prevent pulmonary vascular disease. • Mortality is < 1% How can you characterize the PDA? – – – – – Cyanotic CHD with R-to-L shunt Cyanotic CHD with mixed blood flow Acyanotic CHD with R-to-L shunt Acyanotic CHD with L-to-R shunt Cyanotic CHD with ↓ Pulmonary blood flow Ventricular Septal Defect • VSD – is an abnormal opening in the ventricular septum, which allows free communication between the Rt & Lt ventricles. • Accounts for 25% of CHD. Ventricular Septal Defect • During systole some of the blood from the LV leaks into the RV, passes through the lungs and reenters the LV via the pulmonary veins and LA. • Such circuitous route of blood causes volume overload on the LV. • The LV normally has a much higher systolic pressure (~100 mm Hg) than the RV (~85 mm Hg) and through VSD blood leaks into the RV and elevates RV pressure and volume, causing Pulm HTN. • These changes lead to elevated RV & pulmonary pressures & volume hypertrophy of the LA & LV. Ventricular Septal Defect Clinical Signs & Symptoms • Small - moderate VSD, 3-6mm, are usually asymptomatic. Small defects located predominantly in the muscular septum with slight hemodynamic impairment (Tolochinov-Roge disease) • Moderate – large VSD, almost always have symptoms and will require surgical repair. Ventricular Septal Defect Clinical Signs & Symptoms • If the defect is large and pulmonary vascular resistance is not significantly elevated (L-t-R-shunt) – growth failure, CHF, repeated lower respiratory tract infections (begin at 1-2month); • If the defect is large and pulmonary vascular resistance is very high (Eisenmenger’s reaction) – shortness of breath, dyspnea on exertion, chest pain, cyanosis; Ventricular Septal Defect Listen at the back for radiation of murmurs • Pansystolic/holosystolic murmur - loud, harsh, blowing heard best over the LLSB, frequently is accompanied by thrill (depending upon the size of the defect) +/• more prominent with small VSD, may be absent with a very large VSD. Ventricular Septal Defect Chest X-ray: • increased pulmonary vascularity, • enlargement of the LA and LV; CXR: progressive dilatation of heart. • cardiomegaly • increased pulmonary vascularity, • enlargement of the LA and LV; ECG: overload of LV and RV І ІІ ІІІ V1 V2 V3 AVR V4 AVL V5 AVF V6 LA, LV or biventricular hypertrophy. RV hypertrophy predominates when pulmonary vascular resistance is high. Ventricular Septal Defect Treatment • Small VSD - no surgical intervention, no physical restrictions; • Bacterial endocarditis prophylaxis is indicated. • Symptomatic VSD - Medical treatment initially with afterload reducers & diuretics. Atrial Septal Defect - ASD • is a form of CHD that enables blood flow between the left and right atria via the interatrial septum (it is possible for blood to travel from the left side to the right side of the heart). • Seen in 10% of all CHD. There are 3 major types: Sinus Venosus • Secundum ASD • Primum ASD – low in the septum • Sinus Venosus ASD ASD with left-to-right shunt In normal, the chambers of the left side of the heart are higher pressure than of the right side; ASD with left-to-right shunt • In the case of a large ASD (>9mm), may result in left-to-right shunt, blood will shunt from the LA to the RA. • This extra blood may cause a volume overload of both the right atrium and the right ventricle. • Ultimately the RV must push out more blood than the LV due to the L-to-R shunt. This condition can result in eventually RV-failure (dilatation and decreased systolic function) and Pulm Htn. Atrial septal defect with left-to-right shunt • When the pressure in the RA rises to the level in the LA, the left-to-right shunt will diminish or cease. • When the pressure in the RA to be higher than the pressure in the LA and will reverse the shunt → right-to-left shunt will exist (this phenomenon is known as Eisenmenger’s syndrome). Atrial Septal Defect Clinical Signs & Symptoms • Most are asymptomatic, but may have easy fatigability, mild growth failure, frequent lower respiratory tract infection. • Cyanosis does not occur unless Pulm HTN or R-to-L shunt is present. Atrial Septal Defect Physical finding • mild left precordial bulge (hyperactive precordium); • RV heave (RV systolic lift is palpable at the LSB); Feel the precordium for hyperactivity and for thrills Atrial Septal Defect • Loud 1st heart sound, sometimes pulmonic ejection click; • The 2nd heart sound is widely split and fixed in all phases respiration; Listen carefully Systolic ejection murmur – its medium pitched, seldom accompanied by a thrill, and best heard at the LSB (left middle and upper sternal border); Short, rumbling mid-diastolic murmur produced by the increased volume of blood flow across the tricuspid valve is often audible at the LLSB (lower left sternal border) . Atrial Septal Defect Diagnosis • X-ray chest: pulmonary vascularity is increased • ECG: right-axis deviation; • Echo-CG: RV is enlarged, defect is visualized; І ІІ V1 ECG: V2 right-axis deviation, hypertrophy RV, RA ІІІ AVR V3 V4 V5 AVL V6 AVF Atrial Septal Defect Treatment: • Surgical or catheterization laboratory closure is generally recommended for secundum ASD. • Closure is performed electively between ages 2 & 5 yrs to avoid late complications. • • Mortality is < 1%. Acyanotic Congenital Heart Disease Obstruction to blood flow from ventricles • Coarctation of the Aorta • Pulmonary Stenosis • Aortic Stenosis Coarctation of the Aorta • Coarctation- is narrowing of the aorta at varying points anywhere from the transverse arch to the iliac bifurcation. • Male: Female ratio 3:1. • Accounts for 7 % of all CHD. Coarctation of the Aorta Hemodynamics • Obstruction of left ventricular outflow LV afterload increases pressure hypertrophy of the LV. Coarctation of the Aorta Clinical Signs & Symptoms • Higher BP in the upper extremities as compared to the lower extremities. • 90% have systolic hypertension of the upper extremities. Coarctation of the Aorta Clinical Signs & Symptoms • Classic signs of coarctation are diminution or absence of femoral pulses. • Pulse discrepancy between rt & lt arms. Feel the pulses especially brachial and femoral Coarctation of the Aorta Clinical Signs & Symptoms • Sings of low cardiac output, poor peripheral perfusion LE hypoperfusion, acidosis, HF and shock. • Decreased and delayed pulses in lower extremities. • Systolic ejection murmur @ LSB. • Cardiomegaly, rib notching on X-ray. Coarctation of the Aorta rib notching Coarctation of the Aorta Treatment • With severe coarctation maintaining the ductus with prostaglandin E is essential. • Surgical intervention, to prevent LV dysfunction. • Angioplasty is used by some centers. • Balloon angioplasty is the procedure of choice. Pulmonary Stenosis • Pulmonary Stenosis is obstruction in the region of either the pulmonary valve or the subpulmonary ventricular outflow tract. • Accounts for 7-10% of all CHD. • Most cases are isolated lesions Pulmonary Stenosis Hemodynamics RV pressure hypertrophy RV failure. RV pressures maybe > systemic pressure. Post-stenotic dilation of main PA. W/intact septum & severe stenosis R-L shunt through FO cyanosis. • Cyanosis is indicative of Critical PS. • • • • Pulmonary Stenosis Clinical Signs & Symptoms • • • • • • • • Depends on the severity of obstruction. Asymptomatic w/ mild PS < 30mmHg. Mod-severe: 30-60mmHg, > 60mmHg Prominent jugular a-wave RV lift, RV heave Split 2nd hrt sound Ejection click, followed by systolic murmur. Heart failure & cyanosis not relieved by inhaled oxygen seen in severe cases. Pulmonary Stenosis Treatment • Balloon valvuloplasty, treatment of choice. • Surgical valvotomy is also a consideration. Cyanotic Congenital Heart Disease •Severe Cyanosis PaO2 ≤ 40 mmHg • Obstruction to RV outflow causes intracardiac R-to-L shunting • Complex anatomic defects cause an admixture of pulmonary and systemic venous return in the heart • Decreased pulmonary blood flow – Tricuspid atresia, intact ventricular septum – Critical pulmonary stenosis – Ebstein’s anomaly – Tetralogy of Fallot* • Chest X-Ray Decreased pulmonary vascular markings “Boot-shaped heart” in Tetralogy of Fallot Right sided obstruction 1. Obstruction of RV outflow (Pulmonary stenosis); 2. VSD; 3. Dextroposition of the aorta with override of the ventricular septum; 4. RV hypertrophy Tetralogy of Fallot Assessment Findings with Tetralogy of Fallot Symptoms are variable depending of degree of obstruction • Cyanosis – is variable (isn’t present at the birth, occurs later in the 1st yr of life) • Digital clubbing and hyperpnea at rest are directly related to the degree of cyanosis • Tachycardia • Mental retardation • Retarded growth and development • RV heave • Systolic ejection murmur is heard along the left sternal border Assessment Findings with Tetralogy of Fallot • Paroxymal dyspnea • Severe dyspnea on exertion • Squatting position for the relief of dyspnea caused physical effort, • “Blue” spells, “tet” spells, paroxysmal hypercyanotic attacks – infant becomes hyperpnea, restless, cyanosis increases, gasping respirations, syncope Hypercyanotic Spells/Blue Spells/Tet Spells Clinical Manifestations ٭Most often occurs in morning after feedings, defecation, or crying ٭Acute cyanosis ٭Hyperpnea ٭Inconsolable crying ٭Hypoxia which leads to acidosis Chest X-Ray • Decreased pulmonary vascular marking • “Boot-shaped heart” Treatment of the Child with TOF • • • • Decrease cardiac workload Prevention of intercurrent infection Prevention of hemoconcentration Surgical repair – palliative or corrective surgery Balloon Dilatation of Pulmonic Valve d-Transposition of the Great Arteries d-Transposition of the Great Arteries • Pathophysiology – Cyanosis due to failure of delivery of pulmonary venous blood to the systemic circulation – Two parallel circulations with no mixing – Open atrial septum (fossa ovalis) allows some left-toright shunt, enhanced by a left-to-right ductus arteriosus shunt – Presence of ventricular septal defect facilitates mixing Transposition of the Great Arteries • Aorta from right ventricle, pulmonary artery from left ventricle. • Cyanosis from birth, hypoxic spells sometimes present. • Heart failure often present. • Cardiac enlargement and diminished pulmonary artery segment on x-ray. Transposition of the Great Arteries • Anatomic communication must exist between pulmonary and systemic circulation, VSD, ASD, or PDA. • Untreated, the vast majority of these infants would not survive the neonatal period. Transposition of the Great Arteries Clinical Manifestations • Cyanosis, tachypnea are most often recognized within the 1st hrs or days of life. • Hypoxemia is usually moderate to severe, depending on the degree of atrial level shunting and whether the ductus is partially open or totally closed. • Physical findings, other than cyanosis, may be remarkably nonspecific. • Murmurs may be absent, or a soft systolic ejection murmur may be noted at the midleft sternal border. d-Transposition of the Great Arteries • Chest film – Oval-shaped heart – Narrow mediastinum – Normal or increased pulmonary vascular markings D-Transposition of the Great Arteries This condition is a medical emergency, and only early diagnosis and appropriate intervention can avert the development of prolonged severe hypoxemia and acidosis, which lead to death Treatment When transposition is suspected, an infusion of prostaglandin E1 should be initiated immediately to maintain patency of the ductus arteriosus and improve oxygenation. Endotracheal intubation Infants who remain severely hypoxic or acidotic despite prostaglandin infusion should undergo Rashkind balloon atrial septostomy A Rashkind atrial septostomy is also usually performed in all patients in whom any significant delay in surgery is necessary. Preventing Birth Defects • • • • Stop smoking Avoid drinking alcohol while pregnant Take a daily vitamin containing folic acid Check with your doctor to make sure any medication (over-the-counter or prescription) is safe to take during pregnancy • Stop use of any illegal or "street" drugs Thank you for attention!