* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
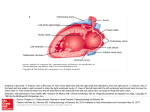
Download 17- interior of heart
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Aortic stenosis wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Borders of the heart The right border: It is formed by right atrium The left border: It is formed by the L. ventricle & L. auricle. The lower border : It is formed mainly by the R. ventricle & by R. atrium. The apex is formed by the left ventricle. The walls of the heart are composed of cardiac muscle ( myocardium ) which is covered externally by the visceral layer of the serous pericardium ( epicardium ) The heart is lined internally with a layer of endothelium ( endocardium ). Chambers It has 2 atria & 2 ventricles. The superior atria are receiving chambers. They are not important in pumping activity. Blood flow into them under low pressure from the veins of the body then to the ventricles. The longitudinal septum which divides the heart is called the interventricular or the interatrial septum. The left ventricle’s walls are thicker than the right & more powerful pump. It is the systemic pump. Right Atrium It consists of a main cavity & outpouching ( the auricle ). Externally at their junction, there is a vertical groove ( the sulcus terminalis ) which on the inside forms a ridge ( the crista terminalis ). The main part of the atrium that lies posterior to the ridge is smooth walled which is derived from the sinus venosus. The part in front of the ridge is roughened or trabeculated by bundles of muscle fibers ( the musculi pectinati ) which is derived from the primitive atrium. Openings into the Right Atrium 1-The Superior Vena Cava opens into the upper part. It has no valve. It returns blood from the upper half of the body. 2- The inferior vena cava opens into the lower part. It guarded by a rudimentary, nonfunctioning valve. It returns the blood from the lower half of the body. 3- The coronary Sinus. It drains most of the blood from the heart wall. It opens between the I.V.C. and the atrioventricular orifice. It is guarded by a rudimentary, nonfunctioning valve. 4- The right atrioventricular orifice. It lies anterior to the I.V.C. opening and is guarded by the tricuspid valve. 5- Many small orifices of small veins which drain the wall of the heart, open directly into the right atrium. Right Ventricle As the cavity approaches the pulmonary orifice it becomes funnel shaped ( infundibulum) The trabeculae carneae are the projecting ridges that gives the ventricular wall a sponge like appearance. They are composed of 3 types. The 1st comprises the papillary muscles which project inward, being attached by their bases to the ventricular wall & their apices are connected by fibrous cords ( chordae tendineae ) to the cusps of the tricuspid valve. The 2nd are attached at their ends to the ventricular wall being free in the middle. One of these ( moderator band ). It crosses the ventricular cavity from the septal to the anterior wall. It conveys the right branch of the atrioventricular bundle. The 3rd type is composed of prominent ridges. Tricuspid valve Guards the right atrioventricular orifice and consists of 3 cusps formed by a fold of endocardium with some connective tissue enclosed. The anterior cusp lies anteriorly – The septal cusp lies against the ventricular septum – the posterior or the inferior lies inferiorly. The bases of the cusps are attached to the fibrous ring of the skeleton of the heart, whereas their free edges and ventricular surfaces are attached to the chordae tendineae which connect the cusps to the papillary muscles. The chordae tendineae of one papillary muscle are connected to the adjacent parts of the 2 cusps. When the ventricle contracts, the papillary muscles contract to prevent the cusps from being forced into the atrium. Pulmonary Valve It guards the pulmonary orifice. It consists of 3 semilunar cusps formed by folds of endocardium with connective tissue enclosed. The curved lower margins and the sides of each cusp are attached to the arterial wall to prevent The cusps from prolapsing into ventricle.The open mouths of the cusps are directed upward into the pulmonary trunk. At the root of the pulmonary trunk are 3 dilatations called sinuses. The 3 semilunar cusps are arranged with one posterior and 2 anterior. During ventricular systole ( 1 ). During ventricular diastole ( 2 ). N.B. No chordae or papillary muscles are 1-1 2- Left atrium It consists of a main cavity and a left auricle. It is situated behind the right atrium and forms the greater pert of the base or posterior surface. Behind it lies the oblique sinus of the serous pericardium and the fibrous pericardium separates it from the esophagus. Its interior is smooth but the auricle have muscular ridges. The 4 pulmonary veins, 2 from each lung open through its posterior wall and have no valves. The left atrioventricular orifice is guarded by the mitral valve. left ventricle Its walls are 3 times thicker than those of the right ventricle. The left ventricular blood pressure is 6 times higher than that inside the right ventricle. In cross section, the left ventricle is circular, the right is crescentic because of the bulging of the ventricular septum into the cavity of the right ventricle. There are well - developed trabeculae carneae, 2 large papillary muscles, but no moderator band. The part below the aortic orifice is called the aortic vestibule. The mitral valve consists of 2 cusps, one anterior & one posterior. The anterior is the larger and intervenes between the atrioventricular & aortic orifices. The aortic valve has one cusp is situated on the anterior wall ( right ) and 2 cusps are located on the posterior wall ( left & posterior ). Behind each cusp the aortic wall bulges to form an aortic sinus. The anterior aortic sinus gives origin to the right coronary artery, the left posterior sinus gives origin to the left coronary artery. Structure of the Heart The atria has thin wall and is divided by the atrial septum. The septum runs from the anterior wall of the heart backward and to the right. The interventricular septum is placed obliquely with one surface facing forward and to the right and the other facing backward and to the left. Its position is indicated on the surface of the heart by the anterior & posterior intervetricular grooves. The lower part of the septum is thick and formed of muscle. The smaller part of the septum is thin and membranous and attached to the fibrous skeleton. The skeleton of the Heart It consists of fibrous rings that surround the 1-atrioventricular orifices 2-pulmonary orifice 3- Aortic orifice and are continuous with the membranous upper part of the ventricular septum. The fibrous rings around the atrioventricular orifices separate the muscular walls of the atria from those of the ventricle but provide attachment for the muscle fibers. The fibrous rings support the bases of the valve cusps and prevent the valves from stretching and becoming incompetent. Conducting system The heart contract at about 70 to 90 beats per minute in the resting adult. The atria contract first and together, to be followed later by the contractions of both ventricles together. It consists of specialized cardiac muscle pressent in the: 1- Sinuatrial node:It located in the wall of the right atrium in the upper part of the sulcus terminalis just to the right of the opening of the S.V.C. The node spontaneously gives origin to rhythmical electrical impulses that spread in all directions through the cardiac muscle of the atria and cause the muscle to contract. 2- Atrioventricular node: It is placed on the lower part of the atrial septum just above the attachment of the septal cusp of the tricuspid valve. From it, the cardiac impulse is conducted to the ventricles by atrioventricular bundle. Conducting system The speed of conduction of the cardiac impulse through the atrioventricular node (0.11 second ) allows sufficient time for atria to empty their blood into the ventricles before the ventricles start to contract. 3- Atrioventricular Bundle ( of His It is the only pathway of cardiac muscle that connects the myocardium of the atria and the myocardium of the ventricles. The bundle descends through the fibrous skeleton of the heart It then descends behind the septal cusp of the tricuspid valve to reach the inferior border of the membranous part of the ventricular septum. At the upper border of the muscular part of the septum it divides into 2 branches, one for each ventricle. The right bundle branch (RBB) passes down on the right side of the ventricular septum to reach the moderator band, where it crosses to the anterior wall of the right ventricle. Here it becomes continuous with the fibers of the Purkinje plexus. Conducting system The left bundle branch (LBB) pierces the septum and passes down on its left side beneath the endocardium. It divides into 2 branches ( anterior & posterior) which become continuous with the fibers of the Purkinje plexus of the left ventricle. Internodal Conduction Paths Impulses from the sinuatrial node have been shown to travel to the atrioventricular node more rapidly than they can travel by passing along the ordinary myocardium. The anterior internodal pathway leaves the anterior end of the sinuatrial node and passes anterior to the SVC opening. It descends on the atrial septum and ends in the atrioventricular node. The middle internodal pathway leaves the posterior end of the sinuatrial node and passes posterior to the SVC opening. It descends on the atrial septum to the atrioventricular node. The posterior internodal pathway leaves the posterior part of the sinuatrial node and descends through the crista terminalis and valve of the inferior vena cava to the atrioventricular node. Arterial supply to the Conducting System It is supplied by the right but sometimes by the left coronary artery. The atrioventricular node and the atrioventricular bundle are supplied by the right coronary artery. The RBB of the atrioventricular bundle is supplied by the left coronary artery. The LBB is supplied by the right & left coronary arteries. Surface Anatomy of the Heart Valves 1- The tricuspid valve lies behind the right half of the sternum opposite the 4th intercostal space. 2- The mitral valve lies behind the left half of the sternum opposite the 4th intercostal space. 3- The pulmonary valve lies behind the medial end of the 3rd left costal cartilage and the adjoining part of the sternum. 4- The aortic valve lies behind the left half of the sternum opposite the 3rd intercostal space. Auscultation of the Heart Valves On listening to the heart with a stethoscope, one can hear 2 sounds: lub- dup. the first sound is produced by the contraction of the ventricles and the closure of the tricuspid and mitral valves. The second sound is produced by the sharp closure of the aortic and pulmonary valves. 1- The tricuspid valve is best heard over the right half of the lower end of the body of the sternum. 2- The mitral valve is best heard over the apex beat, that is at the level of the 5th left intercostal space, 3.5 inch (9 cm ) from the midline. 3- The pulmonary valve is heard over the medial end of the 2nd left intercostal space. 4- The aortic valve is heard over the medial end of the 2nd right intercostal space. Innervation of the Heart Postganglionic fibers reach the heart by way of the superior , middle, and inferior cardiac branches of the cervical portion of the sympathetic trunk and a number of cardiac branches from the thoracic portion of the sympathetic trunk. The efferent preganglionic fibers arise in the upper 4 or 5 thoracic segments of the spinal cord ; pass by white rami communicantes to synapse about cells in the upper thoracic ganglia or travel up the trunk to synapse in the cervical ganglia. The postganglionic fibers pass through the cardiac plexuses and terminate on the sinoatrial and atrioventricular nodes, on cardiac muscle fibers and on coronary arteries. Activation of these nerves results in cardiac acceleration, increased force of contraction of the cardiac muscle and dilatation of the coronary arteries. So, more oxygen and nutrients supply to myocardium. The coronary dilatation is mainly produced in response to local metabolic needs rather than by direct nerve stimulation of the coronary arteries. The parasympathetic preganglionic fibers originate in the dorsal nucleus of the vagus and from cells near the nucleus ambiguus and descend into the thorax in the cardiac branches of the vagus nerves . The fibers terminate by synapsing with postganglionic neurone in the cardiac plexuses and in the walls of the atria. Postganglionic fibers terminate on the sinoatrial and atrioventricular nodes and on the coronary arteries. Activation pf these nerve results in a reduction in the rate and force of contraction of the myocardium and a constriction of the coronary arteries. Also, the coronary constriction is mainly produced by the reduction in local metabolic needs rather than by neural effects. Ischemia and accumulation of metabolic products stimulate pain ending in the myocardium. Afferent fibers running with the vagus nerves take place in cardiovascular reflexes. Cardiac Pain Pain originating in the heart is assumed to be caused by oxygen deficiency and the accumulation of metabolites, which stimulate the sensory nerve endings in the myocardium. The afferent nerve fibers ascend to the central nervous system through the cardiac branches of the sympathetic trunk and enter the spinal cord through the posterior roots of the upper 4 thoracic nerves . The pain is not felt in the heart but is referred to the skin areas supplied by the corresponding spinal nerves. The axons of the primary sensory neurons enter spinal cord segments T1 toT4 or T5 on the left side. The pain varies from a severe crushing pain to a mild discomfort. The skin areas supplied by the upper 4 intercostal nerves and by the intercostobrachial nerve ( T2 ) are therefore affected. The intercostobrachial nerve communicates with the medial cutaneous nerve of the arm and is distributed to skin on the medial side of the upper part of the arm. The pain radiates from the substernal region and left pectoral to the left shoulder and medial aspect of the left arm. The pain is sometimes felt in the neck and jaw. Myocardial infarction involving the inferior wall or diaphragmatic surface of the heart often gives rise to discomfort in the epigastrium. The afferent pain fibers from the heart ascend in the sympathetic nerves and enter the spinal cord in the posterior roots of the 7th ; 8th and 9th thoracic spinal nerves dermatomes in the epigastrium. The heart and the thoracic part of the esophagus have similar afferent pain pathway. So, painful acute esophagitis can mimic the pain of myocardial infarction. The heart is insensitive to touch, cutting, cold and heat. N.B. Synaptic contacts may also be made with commissural neurons ( connector neurons ) that conduct impulses to neurons on the right side of comparable areas of the cord. This is the cause of radiating pain to the right side or both sides.