* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 4th Lecture Updated - Home - KSU Faculty Member websites
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Discovery and development of tubulin inhibitors wikipedia , lookup
Discovery and development of direct Xa inhibitors wikipedia , lookup
Psychopharmacology wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Theralizumab wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Plateau principle wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Neuropharmacology wikipedia , lookup
Drug design wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
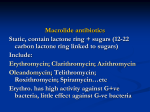
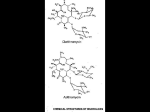
PHL 424 Antimicrobials 4th Lecture By Abdelkader Ashour, Ph.D. Phone: 4677212 Email: [email protected] Inhibitors of bacterial protein synthesis, Macrolides The macrolides are a group of closely related compounds characterized by a macrocyclic lactone ring to which deoxy sugars are attached The prototype drug, erythromycin was obtained in 1952 from Streptomyces erythreus It was the first of these drugs to find clinical application, both as a drug of first choice and as an alternative to penicillin in individuals who are allergic to penicillin The newer members, clarithromycin, azithromycin & telithromycin are semisynthetic derivatives of erythromycin Telithromycin is the first ketolide antimicrobial agent that has been approved and is now in clinical use Ketolides and macrolides have very similar antimicrobial coverage. However, the ketolides are active against many macrolide resistant G+ve strains The structural modifications in these drugs aimed at: improved acid stability Enhanced absorption & tissue penetration broadened the spectrum of activity Inhibitors of bacterial protein synthesis, Macrolides, contd. MOA: Macrolides are bacteriostatic agents that inhibit protein synthesis by binding reversibly to 50S ribosomal subunits of sensitive microorganisms They then inhibit the translocation step wherein a newly synthesized peptidyl tRNA molecule moves from the A site on the ribosome to the P site They may also interfere at other steps, such as transpeptidation This leads to inhibition of bacterial protein synthesis Generally considered to be bacteriostatic. They may be bactericidal at higher doses Their binding site is either identical or in close proximity to that for clindamycin and chloramphenicol Macrolides and clindamycin Inhibitors of bacterial protein synthesis, Macrolides Antimicrobial actions: Erythromycin usually is bacteriostatic, but may be bactericidal in high concentrations against very susceptible organisms G+ve bacteria accumulate about 100 times more erythromycin than do G-ve bacteria It is most active in vitro against aerobic G+ve cocci and bacilli Erythromycin is inactive against most aerobic enteric G-ve bacilli. It has modest activity in vitro against other G-ve organisms (e.g., H. influenzae, N. meningitidis and N. gonorrhoeae) Clarithromycin is slightly more potent than erythromycin against sensitive strains of streptococci and staphylococci Azithromycin is less active than erythromycin against G+ve organisms and slightly more active than either erythromycin or clarithromycin against H. influenzae and N. gonorrhoeae Azithromycin and clarithromycin are activity against some protozoa (e.g., Toxoplasma gondii and Plasmodium spp.). Clarithromycin has good activity against Mycobacterium leprae Inhibitors of bacterial protein synthesis, Macrolides, contd. Resistance mechanisms: Resistance to macrolides usually results from one of four mechanisms: 1. The inability of the organism to take up the antibiotic or the presence of an efflux pump, both of which limit the amount of intracellular drug 2. Ribosomal protection by inducible or constitutive production of methylase enzymes which modify the ribosomal target and decrease drug binding This results in decreased affinity of the 50S ribosomal subunit for the antibiotic 3. Macrolide hydrolysis by esterases 4. Chromosomal mutations that alter 50S ribosomal protein Because the mechanisms producing resistance to erythromycin affect all macrolides, cross-resistance among them is complete Inhibitors of bacterial protein synthesis, Macrolides, contd. Pharmacokinetics Erythromycin base is incompletely but adequately absorbed from the upper small intestine. Because it is inactivated by gastric acid, the drug is administered with enteric coating that dissolves in the duodenum, or as an ester (Clarithromycin, azithromycin, and telithromycin are stable to stomach acid and are readily absorbed) Food, which increases gastric acidity, may delay absorption erythromycin (and azithromycin but can increase that of clarithromycin) Erythromycin diffuses readily into intracellular fluids, achieving antibacterial activity in essentially all sites except the brain and CSF Erythromycin (and telithromycin) are extensively metabolized and are known to inhibit the oxidation of a number of drugs through their interaction with the cytochrome P450 system Interference with the metabolism of drugs such as theophylline and carbamazepine has been reported Large amounts of an administered dose are excreted in the bile and lost in feces, and only 5% is excreted in the urine. Partial reabsorption occurs through the enterohepatic circulation Inhibitors of bacterial protein synthesis, Macrolides, contd. Pharmacokinetics, contd.: Clarithromycin is absorbed rapidly from the GIT after oral administration, but 1st-pass metabolism reduces its bioavailability to ~ 50%. It may be given with or without food The extended-release form, typically given once-daily as a 1-g dose, should be administered with food to improve bioavailability It distributes widely and achieve high intracellular concentrations equal to or exceeding serum concentrations throughout the body Clarithromycin and its metabolites are eliminated by renal and nonrenal mechanisms. It is metabolized in the liver to several metabolites, the active 14-hydroxy metabolite being the most significant. It is recommended that the dosage of this drug be adjusted in patients with compromised renal function Azithromycin's unique pharmacokinetic properties include extensive tissue distribution and high drug concentrations within cells, resulting in much greater concentrations of drugs in tissue compared to simultaneous serum concentrations Tissue fibroblasts act as the natural reservoir for the drug in vivo The drug is slowly released from tissues (tissue half-life of 2–4 days) to produce an elimination half-life approaching 3 days. These unique properties permit once-daily dosing and shortening of the duration of treatment in many cases It undergoes some hepatic metabolism to inactive metabolites, but biliary excretion is the major route of elimination. Only 12% of drug is excreted unchanged in the urine Inhibitors of bacterial protein synthesis, Macrolides, contd. Therapeutic Uses: Erythromycin is the drug of choice for treating persons with B. pertussis disease and for postexposure prophylaxis of household members and close contacts Erythromycin is very effective in corynebacterial infections Erythromycin is useful as a penicillin substitute in penicillin-allergic individuals with infections caused by streptococci or pneumococci Chlamydial infections can be treated effectively with any of the macrolides During pregnancy, erythromycin is recommended as first-line therapy for chlamydial urogenital infections A macrolide or tetracycline is the drug of choice for mycoplasma infections Clarithromycin 500 mg, in combination with omeprazole, 20 mg, and amoxicillin, 1 g, each administered twice daily for 10 to 14 days, is effective for treatment of peptic ulcer disease caused by H. pylori Penicillin is the drug of choice for the prophylaxis of recurrences of rheumatic fever. Erythromycin is an effective alternative for individuals who are allergic to penicillin Inhibitors of bacterial protein synthesis, Macrolides, contd. Side effects: Serious untoward effects are rarely caused by erythromycin. Among the allergic reactions observed are fever, eosinophilia and skin eruptions, which may occur alone or in combination; each disappears shortly after therapy is stopped Cholestatic hepatitis is the most striking side effect (fever, jaundice, impaired liver function), probably as a hypersensitivity reaction Anorexia, nausea, vomiting, and diarrhea occasionally accompany oral administration (due to a direct stimulation of gut motility) Epigastric distress is common for erythromycin. Clarithromycin and azithromycin seem to be better tolerated by the patient Ototoxicity: Transient deafness has been associated with erythromycin, especially at high dosages Drug interactions: Erythromycin and clarithromycin can inhibit cytochrome P450 enzymes and thus increase the serum concentrations of numerous drugs, including theophylline, warfarin, cyclosporine, corticosteroids and digoxin This can lead to toxic accumulations of these drugs Azithromycin appears to be free of these drug interactions Inhibitors of bacterial protein synthesis, Macrolides, contd. Contraindications: Patients with hepatic dysfunction should be treated cautiously with erythromycin, telithromycin, or azithromycin, because these drugs accumulate in the liver. Similar situation with patients who are renally compromised Telithromycin has the potential to prolong the QTc interval in some patients. Therefore, it should be avoided in patients with congenital prolongation of the QTc interval and in those patients with proarrhythmic conditions