* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Mechanism of action
Survey
Document related concepts
Toxicodynamics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Prescription costs wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
Drug interaction wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Transcript
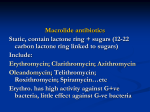
Protein synthesis inhibitors - Are group of broad spectrum antibiotics. They are selectively toxic, since they act on bacterial ribosomes and spare the host cells. Large doses of tetracycline and chloramphenicol are toxic as they interact with mitochondrial ribosomes (which are nearly similar in human and bacteria). Tetracyclines - Reduced usefulness due to resistance. Called so for their 4 (tetra) hydrocarbon rings (cycle) derivation (ine). ). Substitutions on these rings alter the individual pharmacokinetics and spectrum of antimicrobial activity Mechanism of action: Tetracyclines enter susceptible organisms via passive diffusion and also by an energy-dependent transport protein mechanism unique to the bacterial inner cytoplasmic membrane. - Sensitive organisms have high drug uptake than human cells → selective action. - Bacteriostatic effect is due to: The drug binds reversibly to the 30s subunit of bacterial ribosome, blocking the access of aminoacyl-t-RNA to m-RNA ribosome Complex → prevent addition of aminoacyl to the growing peptide → protein synthesis inhibition. Pharmacokinetics: 1. Absorption: all tetracyclines are adequately but incompletely absorbed in upper GIT after oral administration. ++ ++ +3 Diary food, Mg , Ca , iron, Al , antacids and ↑pH → ↓ absorption (less with doxycycline) due to the formation of non absorbablechlates. Doxycycline is preferred for parenteral route, and doxycycline and minocycline are totally absorbed. 2. Distribution: - T.C. concentrate in liver, spleen, kidney, skin and bind to tissue undergoing calcification ++ - - (teeth, bones, tumor, with Ca content e.g. gastric carcinoma). They penetrate into most body fluid even tear and saliva but their levels in CSF are insufficient for therapeutic efficacy except minocycline → CSF even in absence of brain inflammation. All T.C. → placenta → concentrated in fetal bones and dentition. 3. Fate: - metabolized and conjugated in liver → soluble glucuronides → bile. - Subjected to enterohepatic circulation (reabsorbed in the intestine) → ↑ T1/2. - Excreted by the kidney. - Liver disease or renal disease → ↑ T1/2 of the drug. - Doxycycline is eliminated by non renal mechanism (through bile), is safe in renal insufficiency. - T.C. excreted in breast milk. Anti bacterial spectrum and clinical uses - Effective against sensitive gram +ve, gram –ve bacteria. Especially in allergic to β-lactam and macrolides but resistance → less popular use. - Drug of choice against: 1. Chlamydia infection:due to chlamydia trachomatis,the major cause of STD inUS. a. Non gonococcal urethritis. b. Pelvic inflammation e.g. salpingitis. c. Lymphogranulomavenereum. 2. Rocky mountain spotted fever caused by rickettsia rickettsii. 3. Mycoplasma pneumonia → pneumonia in young adult and in people who live in close places → military camps. 4. Anthrax → due to bacillus anthracis, doxycycline is a prophylactic Rx. 5. Rx of acne and Rosacea. 6. Gram –ve rods. a. For Rx of Brucella.(tetracycline + gentamicin). b. Also in cholera Rx: a. Doxycycline. b. Fluid replacement. c. Yersinia pestis → buboric plague. 7. Lyme disease due to spirochetes infection. 8. Demeclocycline → non antibiotic action e.g. Rx of SIADH secretion. 9. In combination regimen for P.U. (peptic ulcer) Rx caused by H-pylori. 10. For Rx of protozoal infection e.g. amaebiasis and malaria (P. falciparum). 11. Minocycline used for eradication of meningococcal carrier but due to side effects and resistance, rifampicin is indicated. - T.C. → tetracyclines (tetracycline, minocycline, doxycycline, demeclocycline). Side effects: Hypersensitivity is uncommon. Most side effects are due to direct toxicity or alteration of microbial flora. 1. GIT→ nausea, vomiting, diarrhea (most common) due to local irritation of GIT → non compliance of patient and alteration of normal flora → ↑ growth of pseudomonas, proteus, candida, clostridia ….. → diarrhea. o Pseudomembranous enterocolitis associated with clostridium difficile Rx with metronidazole. o For Rx of GIT side effect: I. Stop Rx. II. ↓ Dose. III. Give drug with food other than dairy product. 2. Bony structure and teeth: ++ T.C. bound to Ca deposited in newly formed bones and teeth during calcification in growing children, and that lead to: a. Discoloration of teeth and enemal dysplasia. b. Deformity and growth inhibition of bones. Therefore avoid drugs in children under 8-12 years and during pregnancy. 3. Fatal hepatotoxicity: Occurs mainly in pregnant women who received ↑ doses of tetracyclines I.V., or they have preexisting hepatic or renal disease, T.C. → hepatic necrosis. 4. Kidney toxicity: → nitrogen retention. 5. Phototoxicity → mainly in Fair – skinned patients. 6. Vestibular reactions: dizziness, nausea, vomiting, mainly occur with minocycline and doxycycline → concentrated in endolymph of the ear. 7. Local tissue damage → I.V. route → thrombosis, I.M. → local irritation (avoid it). 8. Super infection: → over growth with candida, staph ….. → diarrhea and P.M.C. 9- Pseudotumor cerebri: Benign, intracranial hypertension characterized by headache and blurred vision may occur rarely in adults. Although discontinuation of the drug reverses this condition, it is not clear whether permanent sequelae may occur. Resistance The most commonly encountered naturally occurring resistance to tetracyclines is an efflux pump that expels drug out of the cell, thus preventing intracellular accumulation. Other mechanisms include - enzymatic inactivation of the drug, -and production of bacterial proteins that prevent tetracyclines from binding to the ribosome. Resistance to one tetracycline does not confer universal resistance to all tetracyclines. Contraindications: 1) 2) 3) 4) Pregnant female. Children under 12 years. Renal failure except doxycycline. Liver disease. • • GLYCYLCYCLINES Tigecycline a derivative of minocycline, is the first available member of the glycylcycline antimicrobial class. It is indicated for the treatment of complicated skin and soft tissue infections, as well as complicated intra-abdominal infections. Mechanism of action Tigecycline exhibits bacteriostatic action by reversibly binding to the 30S ribosomal subunit and inhibiting protein synthesis Antibacterial spectrum exhibits broad-spectrum activity that includes methicillin resistant staphylococci (MRSA), multidrug-resistant streptococci, vancomycin-resistant enterococci (VRE), extendedspectrum β-lactamase–producing gram-negative bacteria, Acinetobacter baumannii, and many anaerobic organisms. However, tigecycline is not active against Morganella, Proteus, Providencia, or Pseudomonas species. • • • • • • • • • • • • Resistance Tigecycline was developed to overcome the recent emergence of tetracycline class–resistant organisms that utilize efflux pumps and ribosomal protection to confer resistance. However, resistance is seen and is primarily attributed to overexpression of efflux pumps. Pharmacokinetics Following IV infusion, tigecycline exhibits a large volume of distribution. It penetrates tissues well but has low plasma concentrations. Consequently, tigecycline is a poor option for bloodstream infections. The primary route of elimination is biliary/fecal. No dosage adjustments are necessary for patients with renal impairment. However, a dose reduction is recommended in severe hepatic dysfunction. • Adverse effects • • • • • • significant nausea and vomiting. Acute pancreatitis, including fatality, Elevations in liver enzymes and serum creatinine may also occur. Other adverse effects are similar to those of the tetracyclines and include photosensitivity, pseudotumor cerebri, discoloration of permanent teeth when used during tooth development, and fetal harm when administered in pregnancy. • Tigecycline may decrease the clearance of warfarin and increase prothrombin time. Therefore, the international normalized ratio should be monitored closely when tigecycline is coadministered with warfarin. Macrolides: Erythromycin, clarithromycin, azithromycin and telithromycin( aketolide). - A group of antibiotics with a macrocyclic lactone structure to which deoxy sugar are attached. - Erythromycin was 1 of this group used as 1 choice and ultrenative to penicillin in allergic patient to β-lactam antibiotics. Telithromycin: ketolide drug has an antibacterial spectrum similar to that of azithromycin. Moreover, the structural modification within ketolides neutralizes the most common resistance mechanisms (methylase-mediated and efflux-mediated) that make macrolides ineffective - st st - Mechanism of action: Bacteriostatic, but bactericidal at ↑ doses. Bind irreversibly to 50s subunit of bacteria inhibiting the translocation steps, they may also interfere at other steps e.g. transpeptidation → inhibit protein synthesis. - Pharmacokinetics: 1) Absorption → adequate absorption on oral administration. o Clarithromycin, azithromycin and telithromycin are stable to stomach acid and readily absorbed, while erythromycin base is destroyed by gastric acid must be administered as enteric – coated tab. Or esterified form are used. o Food ↑ absorption of clarithromycin, but interferes with absorption of others. o Azithromycin is available for I.V. infusion. Erythromycin I.V. → thrombophlebitis. 2) Distribution: They have a large volume of distribution (in case of erythromycin toxicity, it will not removed by dialysis). Erythromycin distribution to all body fluid except CSF, diffuses into prostatic fluid, accumulate in macrophages. All concentrate in liver. Azithromycin has longer T1/2 > 40 hours& larger volume of distribution Inflammation allows for greater tissue pentration. 3) Fate: All except azithromycin are cytochrome P450 system inhibitors. All have active metabolites except erythromycin. Erythromycin traverse the placenta → fetus. Erythromycin and telithromycin are extensively metabolized. 4) Excretion: Erythromycin and azithromycin are concentrated&excreted in bile in an active form(95%). Partial re-absorption through enterohepatic circulation. Inactive metabolites are excreted in urine Clarithromycin and its metabolites are eliminated by liver and kidney, therefore dose adjustment is needed in renal failure. Resistance Several mechanisms have been identified: 1) the inability of the organism to take up the antibiotic or the presence of an efflux pump, both of which limit the amount of intracellular drug; 2) a decreased affinity of the 50S ribosomal subunit for the antibiotic,; and 3) the presence of a plasmid-associated erythromycin esterase. Both clarithromycin and azithromycin show cross-resistance with erythromycin, but telithromycin can be effective against macrolide-resistant organisms Clinical use: Most hospital staph.are resistant to erythromycin. Erythromycin is the drug of choice in Rx of diphtheria and erythrasma, also used to Rx diphtheria carrier. Used in Rx of patients allergic to penicillin, (effective against many of the same organism as penicillin G). In chlamydial infection: a. Azithromycin is alternative to tetracycline in→ urethritis, endocervical,rectal, epididymal infection. b. Erythromycin → drug of choice for urogenital infection during pregnancy. Mycoplasma pneumonia infection → erythromycin or tetracycline. Rx of syphilis → erythromycin in allergic patients to penicillin. Legionnaires disease (legionellosis), azithromycin is the drug of choice. Neisseria gonorrhea (gram –vecocci). Pertussis. Eradication of H-pylori → clarithromycin. H. influenzae → azithromycin which is more active against RTI and mycobacterium avium – intracellular complex in AIDs patients with disseminated infection. Telithromycin = azithromycin in its antibacterial spectrum,ketolides are active against many macrolide resistant gram positive strains Adverse effects: 1. GIT disturbance → poor compliance. 2. Cholestatic jaundice → as hypersensitivity reaction to estolate form of erythromycin and other members also recorded. 3. Ototoxicity → transient deafness especially with high doses of erythromycin. 4. Contraindications: o Hepatic dysfunction, especially with erythromycin, telithromycin or azithromycin → accumulated in liver. o In renally compromised patients, give telithromycin with caution. o Telithromycin → may worsen myasthenia gravis , can cause severe hepatotoxicity & has the potential to prolonge QT INTERVAL 5. Interactions: o All except azithromycin inhibit CYP 450, inhibit metabolism of astemizole, carbamazepine, cyclosporine, theophylline, valproate, warfarin, terfinadine and others → toxic accumulation of these drugs. o In some patients they interact with digoxin as they ↓ species of intestinal flora that inactivates digoxin → ↑ re-absorption of drug. o o