* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Sunday 22nd December: PSA1
Survey
Document related concepts
Pharmacokinetics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Pharmacognosy wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Dextropropoxyphene wikipedia , lookup
Drug interaction wikipedia , lookup
Medical prescription wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription costs wikipedia , lookup
Electronic prescribing wikipedia , lookup
Transcript
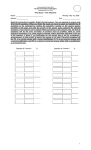
PSA QUESTION EXAMPLES Calculation Case presentation A 79-year-old man is admitted to hospital from a nursing home with congestive cardiac failure. He is taking several medicines, including digoxin (dose 0.125 mg daily according to the referral letter). He is struggling to take his medicines and, where possible, prefers to take these in liquid form. Digoxin is provided as an elixir of strength 50 micrograms/mL. Calculation What volume of elixir should he be given each day according to the information in the referral letter? (Write your answer in the box below) Answer: 2.5 mL Answer box Working The dosage of digoxin is given as 0.125 mg although good practice would dictate that this should have been given as 125 micrograms. Strength of digoxin elixir = 50 micrograms/mL. Volume of elixir to be administered = 125/50 = 2.5 mL Data interpretation Case presentation A 58-year-old woman with a long history of COPD is admitted with type 2 respiratory failure. Investigations Arterial blood gases breathing air PO2 6.4 kPa (11.3–12.6), PCO2 6.6 kPa (4.7–6.0), pH 7.40 (7.35–7.45), H+ 40 nmol/L (35–45). After breathing oxygen 28% via a Venturi mask for 20 minutes, PO2 is 9.1 kPa and PCO2 8.4 kPa, pH 7.28, H+ 53 nmol/L. Question Select the most appropriate decision option with regard to the oxygen prescription based on these data. (mark it with a tick) A DECISION OPTIONS continue oxygen 28% via a Venturi mask B discontinue oxygen therapy C increase oxygen to 35% via a Venturi mask D reduce oxygen to 24% via a Venturi mask E substitute oxygen 2L/min via nasal prongs Answer box Option A Justification These data indicate that although there has been a significant increase in oxygenation she is experiencing a significant increase in CO2 retention while breathing 28% oxygen, which has reduced her hypoxic respiratory drive and might depress her conscious level. Option B Justification She requires some oxygen to treat her hypoxaemia. Option C Justification This would be potentially life-threatening because she is already showing a significant increase in CO2 retention on 28% oxygen. Option D Justification Oxygen concentration should be reduced so that the CO2 retention is reduced while achieving a reasonable increase in arterial PO2. Her blood gas should be repeated soon after changing this. Option E Justification This uncontrolled delivery of oxygen is potentially hazardous in type 2 respiratory failure. Prescription review Case presentation An 82-year-old woman is admitted to the emergency department following a fall that resulted in a significant head injury. She is drowsy, has a persisting headache and has vomited once. PMH. Angina, peripheral vascular disease and irritable bowel syndrome. DH. Her current regular medicines are listed (right). On examination Her Glasgow coma score is 14 and she has no focal neurological signs. She requires stitches to a cut above her right eye. She will be kept in for head injury observations and a CT scan of her head. Question A Select the TWO prescriptions that should be withheld. (mark them with a tick in column A) Question B Select the TWO prescriptions that are most likely to have contributed to her fall. (mark them with a tick in column B) Resource associated with this item: No resource has been associated with this item. Drug bisacodyl CURRENT PRESCRIPTIONS Dose Route Freq. 5 mg ORAL daily clopidogrel A B 75 mg ORAL daily isosorbide mononitrate 20 mg ORAL twice daily mebeverine 135 mg ORAL three times daily paracetamol 1g temazepam 10 mg ORAL nightly as required ORAL 12-hrly Answer box Question A Antiplatelet agents such as clopidogrel should be withdrawn until the CT scan of head excludes bleeding in or around the brain (subdural, contusion, etc). If continued they may worsen bleeding and prohibit neurosurgical intervention. Temazepam may cause sedation, especially if she takes it intermittently, and this could make neurological observations hard to interpret. Question B Sedatives such as temazepam are a risk factor for falls, especially in older people. ISMN may cause postural hypotension and lead to falls. Adverse drug reactions-management Case presentation A 52-year-old woman presents to her GP complaining of a persistent irritating dry cough. PMH. Essential hypertension. DH. Perindopril 4 mg orally daily and simvastatin 40 mg orally nightly. On examination BP 135/85 mmHg. Question Select the most appropriate option for the management of this adverse drug event. (mark it with a tick) Resource associated with this item: No resource has been associated with this item. A MANAGEMENT OPTIONS add codeine phosphate 30 mg orally as required B halve perindopril dose to 2 mg orally daily C stop simvastatin D substitute losartan 50 mg orally daily for perindopril E substitute ramipril 5 mg orally daily for perindopril Answer box Option A Justification The patient should not be treated with a cough suppressant. Option B Justification The adverse effects are caused by the ACE inhibitor, which should be withdrawn and replaced by an angiotensin II receptor antagonist. It is likely the patient will need an antihypertensive. ADR is independent of dosage. Option C Justification Simvastatin does not cause a persistent irritating dry cough. Option D Justification Changing to an angiotensin II receptor antagonist is recommended in patients who have to discontinue an ACE inhibitor because of a dry cough. Option E Justification The adverse effects are caused by all of the ACE inhibitors. Adverse drug reactions Case presentation A 73-year-old woman with chronic back pain visits her GP for a review of her medication. DH. Her current regular medicines, in addition to morphine sulfate (immediate release) 10 mg orally 4-hrly for breakthrough pain, are listed (right). Question Select the prescription that is most likely to interact with morphine sulfate to reduce its analgesic effect. (mark it with a tick) A PRESCRIPTION OPTIONS amitriptyline hydrochloride 20 mg orally nightly B buprenorphine '35' patch (Transtec®) releasing 35 micrograms per hour C ibuprofen 200 mg orally 8-hrly D paracetamol 1g orally 6-hrly E tramadol 50 mg orally 6-hrly Answer box Option A Justification Sedative effects are possibly increased when tricyclics are given with opioid analgesics, but this does not reduce the analgesic effect. Option B Justification Buprenorpine has partial agonist effects that will antagonise the analgesic effect of the morphine. Option C Justification Ibuprofen does not interact with the other drugs. Option D Justification Paracetamol does not interact with the other drugs. Option E Justification Tramadol is a synthetic opioid; although it is illogical to take the two drugs together, tramadol does not antagonise the analgesic effects of morphine Therapeutic monitoring Case presentation A 59-year-old woman returns to her GP for a third measurement of her BP, after it had been found raised on two previous occasions. The reading is 154/92 mmHg and the GP prescribes ramipril 1.25 mg orally daily. Question Select the most appropriate monitoring option required 2 weeks after initiation of this treatment. (mark it with a tick) MONITORING OPTIONS A eGFR B plasma glucose C serum angiotensin-converting enzyme D serum cholesterol E serum sodium Answer box Option A Justification eGFR should be monitored as ACE-I may cause renal impairment. Option B Justification Although ramipril has been reported to cause hypoglycaemia, it is more important to monitor renal function in patients in whom the drug has recently been initiated. Option C Justification Although ramipril is an ACE-inhibitor, drug effect is not usually assessed by measuring serum ACE. Option D Justification Hypercholesterolaemia is is a risk factor for IHD not hypertension, and it is not a guide to the effectiveness of an antihypertensive agent. Option E Justification Although ACE-I treatment should be used with caution in severe hyponatraemia, it would be more important to ensure that renal function has not deteriorated. Management Case presentation A 74-year-old man presents to his GP with a swollen painful and hot right toe for 1 week. This is the third time this has happened in 18 months. PMH. Hypertension, ischaemic heart disease and heart failure DH. Aspirin 75 mg orally daily, ramipril 5 mg orally daily, simvastatin 40 mg orally nightly. On examination Temperature 37.0°C, HR 72/min and regular, BP 138/ 76 mmHg, RR 18/min. Investigations Serum urate 0.52 mmol/L ( 0.23–0.46) Question Select the most appropriate management option at this stage. (mark it with a tick) A MANAGEMENT OPTIONS start allopurinol 100 mg orally daily B start colchicine 500 micrograms orally 8-hrly C start diclofenac 50 mg orally 8-hrly D stop aspirin E stop ramipril Answer box Option A Justification Allopurinol should not be prescribed in acute attacks of gout as it can worsen symptoms. Option B Justification Colchicine is the recommended treatment for gout in patients with heart failure to suppress pain and inflammation. Option C Justification NSAIDs can be used to treat gout but should not be used in patients with heart failure. Diclofenac has a high risk of cardiovascular events. Option D Justification He requires his aspirin for cardiovascular protection and stopping it will have no effect on his gout Option E Justification Ramipril does not cause gout. Communications Case presentation A 24-year-old woman requires malaria prophylaxis for business travel to Papua New Guinea. After checking the latest guidance, her GP recommends doxycycline capsules 100 mg orally daily. Question Select the most appropriate information option that should be communicated to the patient. (mark it with a tick) A INFORMATION OPTIONS doxycycline may discolour her teeth B doxycycline should not be taken if there is any possibility she may be pregnant C she should continue treatment for 1 week after she has left the country D she should take the capsules immediately before going to bed E she will also need to take antacids to reduce irritation of the gullet by doxycycline Answer box Option A Justification This is only a problem in children, and therefore because of this and the risk of dental hypoplasia, tetracyclines should not be given to children under 12 years. Option B Justification Doxycycline is contra-indicated in pregnancy (and breastfeeding) because it may be deposited in fetal teeth and bones. Option C Justification Doxycycline prophylaxis for malaria should be started 1 - 2 days before entering the endemic area, and continued for 4 weeks after leaving. Option D Justification Doxycycline capsules should be swallowed whole with plenty of fluid during meals, while sitting or standing to reduce the risk of oesophageal irritation. Option E Justification Antacids decrease the absorption of doxycycline and the two should not be prescribed together. Prescription Case presentation An 8-year-old girl presents to the emergency department following a seizure. Following a period of continuous muscle contraction, she develops bilateral synchronous limb movements lasting longer than 15 minutes and status epilepticus is diagnosed. PMH. Tonic–clonic seizures for 3 years. DH. Sodium valproate syrup 350 mg orally 12-hrly. She has not missed any doses. Her body weight is 30 kg. Prescribing request Write a prescription for ONE drug that will help to treat this condition. (use the hospital ‘once-only medicines’ prescription chart provided) Scoring drugs: Diazepam, lorazepam, midazolam 4 Clonazepam 3 Phenytoin, fosphenytoin 2 Phenobarbital 1 (These marks are the maximum you can get if you also have the correct route and dose. Remember you will have the BNF throughout.) Prescription Case presentation A 28-year-old woman underwent a laparoscopic cholecystectomy 6 hours ago under general anaesthesia. The anaesthetist has prescribed regular paracetamol 1 g orally 6-hrly. She was given a dose 1 hour ago and is still complaining of abdominal pain. Her intravenous cannula became blocked 2 hours ago and has been removed. PMH. Asthma since childhood and cannot tolerate aspirin. DH. Salbutamol inhaler 200 micrograms 6-hrly and budesonide inhaler 100 micrograms 6-hrly. On examination Temperature 36.8°C, HR 102/min and rhythm regular, BP 134/83 mmHg, RR 18/min, O2 sat 97% (94–98) breathing air. Her pain score is 4/10. Prescribing request Write a prescription for ONE drug that will help to alleviate her pain. (use the hospital 'regular medicines' prescription chart provided) Scoring drugs: Codeine, dihdrocodeine, tramadol, meptazinol 4 Nefopam 3 Buprenorphine, morphine, oxycodone, pethidine 2 Diamophine, fentanyl 1 NSAIDs, co-codamol etc 0 (Puzzled why nefopam is included, no-one uses it! The potent opioids are too strong for this situation. Note that patient is aspirin sensitive, so no NSAIUDs if possible; and is already on paracetamol, so no co- drugs as risk of paracetamol overdose)