* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CDHO Factsheet Human Papillomavirus
Neglected tropical diseases wikipedia , lookup
Neonatal infection wikipedia , lookup
Kawasaki disease wikipedia , lookup
Common cold wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Schistosomiasis wikipedia , lookup
Germ theory of disease wikipedia , lookup
Periodontal disease wikipedia , lookup
Behçet's disease wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Globalization and disease wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Human papillomavirus infection wikipedia , lookup
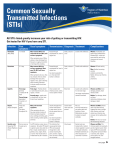
Disease/Medical Condition HUMAN PAPILLOMAVIRUS Date of Publication: May 19, 2015 (also known as “HPV infection” or warts; various wart forms also known as common or “verruca vulgaris”, flat, filiform, periungal, mosaic, and plantar; STI-related/genital warts also known as “condylomata acuminata” or “papilloma venereum”; caused by 100+ types of human papillomavirus [HPV]; sexually transmitted form also known generically as a “sexually transmitted infection” [STI], “sexually transmitted disease”, “STD”, “venereal disease”, and “VD”) Additional information on oropharyngeal human papillomavirus (HPV) infection is addressed in the Oral Cancer Fact Sheet. Is the initiation of non-invasive dental hygiene procedures* contra-indicated? Potentially ■ Is medical consult advised? ......................................... Yes, if active infectious oral disease is suspected on the basis of history and/or examination. ■ If patient/client has oral and/or reproductive/systemic manifestations suggestive of an STI, refer to primary care provider (e.g., physician or nurse practitioner) for follow-up and diagnosis (e.g., visual inspection, biopsy, etc., for HPV infection). In the case of oral condylomata acuminata, lesions may require surgical excision, chemical treatment, or laser ablation. Instruct patient/client to reschedule dental hygiene appointment when oropharyngeal HPV infection has been appropriately treated. Is the initiation of invasive dental hygiene procedures contra-indicated?** Potentially ■ Is medical consult advised? .......................................... See above. ■ Is medical clearance required? ..................................... Yes, if active infectious oral disease is suspected on the basis of history and/or examination. ■ Is antibiotic prophylaxis required? ................................. No. ■ Is postponing treatment advised? .................................. Yes, if active infectious oral disease is suspected on the basis of history and/or examination. Oral management implications ■ Mode of transmission: Usually through direct contact with infected skin or mucous membranes. Warts may be autoinoculated (e.g., by razors in shaving), and contaminated floors are often implicated in plantar warts. STI-related warts result from intimate interpersonal contact (oral-oral; oral-penile; oral-anal; oral-vulvar/vaginal; penile-vaginal; penile-anal), some of which can result in oral manifestations. The risk of transmission during oral sex (fellatio, cunnilingus, and anilingus) is increased if there are small cuts in the mouth (e.g., from dental work; brushing or flossing before/after oral sex; gum disease; or sharp foods). Risk during oral sex is also increased if there are sores on the mouth or genitals caused by rough or prolonged oral sex or an STI such as herpes or syphilis; if the person receiving oral sex is menstruating; and if there is holding of semen, vaginal fluid, or menstrual blood in the mouth for a long time or if it is swallowed. ■ Sex partners of patients/clients with STIs should be assessed by an appropriate healthcare professional (e.g., physician) and treated as appropriate. The presence of oral warts should prompt referral to a physician to rule out genital lesions in the patient/client and his/her sexual partners. ■ To reduce acquisition and spread of oral cavity STIs, condoms or dental dams should be used for all oral-genital and oral-anal contact. Brushing or flossing of teeth should be avoided within 30 minutes of giving oral sex. ■ Oral condylomata identified in children raises suspicion of sexual child abuse when nonsexual contact, autoinoculation from other sites, and maternal-fetal transmission have been ruled out; dental hygienists should be familiar with their professional reporting obligations to the Children’s Aid Society. Additionally, palatal petechiae in children could be a sign of forced oral sex. ■ While the presence of genital or other non-oral warts in a patient/client does not affect dental hygiene management, oral warts are infectious. Standard precautions apply during oral dental hygiene procedures, which is important to avoid finger/ periungal (fingernail area) wart acquisition by the dental hygienist. cont’d on next page... Disease/Medical Condition HUMAN PAPILLOMAVIRUS (also known as “HPV infection” or warts; various wart forms also known as common or “verruca vulgaris”, flat, filiform, periungal, mosaic, and plantar; STI-related/genital warts also known as “condylomata acuminata” or “papilloma venereum”; caused by 100+ types of human papillomavirus [HPV]; sexually transmitted form also known generically as a “sexually transmitted infection” [STI], “sexually transmitted disease”, “STD”, “venereal disease”, and “VD”) Oral management implications (cont’d) ■ Dental hygienists with periungal or other warts on their hands should seek medical treatment to accelerate resolution and decrease viral transmission potential. ■ Laser ablation of oral condylomata acuminata should involve high-speed evacuation to avoid inhalation of the virus-laden plume, which can lead to laryngeal condylomata. ■ High-risk types of HPV are implicated in oropharyngeal cancers. These HPV-related cancers are usually found in the lingual and palatine tonsils, the soft palate, and the base of the tongue. ■ HPV immunization greatly reduces rates of oropharyngeal infection by high-risk types, and this will likely translate into reduced incidence of HPV-related oropharyngeal cancers in the future. In order to prevent HPV-related oral cancer, dental hygienists can play a role in suggesting that unvaccinated patients/clients — both male and female, particularly those aged 9 to 26 years — speak with their primary care physician regarding possible immunization. Currently in Ontario, HPV vaccine is publicly funded for all female Grade 8 students. Oral manifestations ■ Condylomata acuminata (STI-related warts, often associated with HPV types 2, 6, and 11) occur on the ventral tongue, gingiva, labial mucosa, and palate. These lesions have small, finger-like projections, resulting in an exophytic lesion with a rough or cauliflower-like verrucous surface. They tend to be larger, more clustered, more diffuse, and more deeply rooted than HPV-associated squamous papilloma lesions; they tend to be pinker than, and generally not as well keratinized as, the verruca vulgaris. ■ Verruca vulgaris, or the common wart, can be found in the oral cavity. It is usually white and most commonly found on the keratinized surfaces of the gingiva and palate. ■ Filiform warts can manifest on the lips. They are elongated, pointed, and delicate lesions that may reach 1 cm in length. ■ Although oral warts can occur in any individual regardless of HIV status, recurrence after treatment is uncommon except in the case of HIV-infected persons. HIV-associated oral warts can be large and multi-focal, resulting in aesthetic and functional problems. Related signs and symptoms ■ HPV infection manifests as diverse skin and mucous membrane lesions. The common wart is a circumscribed, hyperkeratotic, rough-textured painless papule, which varies in size from a pinhead to large masses. Filiform warts are usually found on the eyelids, face, and neck, in addition to the lips. Laryngeal papillomas occur on the vocal cords and epiglottis of children (likely transmitted during passage of the infant in the birth canal) and adults, and occasionally become malignant. Flat warts are smooth and slightly elevated, usually occurring in multiple lesions varying from 1 mm to 1 cm. Plantar warts are flat, hyperkeratotic, and sometimes painful lesions on the soles of the feet. ■ More than 70% of sexually active Canadians (both men and women) are estimated to have a sexually transmitted HPV infection at some time during their lives. Many infected persons never develop overt signs/symptoms, but they still carry the virus and can infect their sexual partners. If genital warts are visible, they may manifest as small, cauliflower-like bumps, alone or in clusters, on the vulva, cervix, anus, penis, or thighs. cont’d on next page... 2 Disease/Medical Condition HUMAN PAPILLOMAVIRUS (also known as “HPV infection” or warts; various wart forms also known as common or “verruca vulgaris”, flat, filiform, periungal, mosaic, and plantar; STI-related/genital warts also known as “condylomata acuminata” or “papilloma venereum”; caused by 100+ types of human papillomavirus [HPV]; sexually transmitted form also known generically as a “sexually transmitted infection” [STI], “sexually transmitted disease”, “STD”, “venereal disease”, and “VD”) Related signs and symptoms (cont’d) ■ In women, HPV infection of the cervix can be detected by the Papanicolaou (Pap) test, by examining cervical cells under a microscope. Oncogenic (potentially cancer-causing) types of HPV are the cause of most cervical and anal cancers. ■ Warts usually regress spontaneously within months to years. Treatment of the affected person decreases the amount of wart virus available for transmission. References and sources of more detailed information ■ Middlesex-London Health Unit www.healthunit.com/human-papilloma-virus www.healthunit.com/oral-sex www.healthunit.com/sexually-transmitted-infections ■ AW Weiss and H Dym. Oral lesions caused by human papillomavirus. The Clinical Advisor (January 10, 2011). www.clinicaladvisor.com/oral-lesions-caused-by-human-papillomavirus/article/193918 ■ EW Harville, J Zhang, and MC Hatch. Oral sex and gum disease (letter). Sex Transm Infect 2004;80:418-419. www.sti.bmj.com/content/80/5/418.full ■ The Chief Public Health Officer’s Report on the State of Public Health in Canada, 2013. Sexually Transmitted Disease — A Continued Public Health Concern. http://www.phac-aspc.gc.ca/cphorsphc-respcacsp/2013/sti-its-eng.php ■ U.S. Centers for Disease Control and Prevention http://www.cdc.gov/std/hpv/stdfact-hpvandoralcancer.htm ■ WebMD http://www.webmd.com/skin-problems-and-treatments/tc/warts-and-plantar-warts-topic-overview ■ Update on Human Papillomavirus (HPV) Vaccines — An Advisory Committee Statement of the National Advisory Committee on Immunization. Canada Communicable Disease Report 2012;38:ACS-1. ■ JW Little, DA Falace, CS Miller and NL Rhodus. Dental Management of the Medically Compromised Patient (8 th edition). St. Louis: Elsevier; 2013. ■ D. Heymann (ed.). Control of Communicable Disease Manual (18th edition). Baltimore: American Public Health Association; 2004. ■ M. Darby (ed.) and M. Walsh (ed.). Dental Hygiene: Theory and Practice (3rd edition). St. Louis: Saunders Elsevier; 2010. ■ OAC Ibsen and J Andersen Phelan. Oral Pathology For The Dental Hygienist (6th edition). St. Louis: Saunders Elsevier; 2014. * Includes oral hygiene instruction, fitting a mouth guard, taking an impression, etc. ** Ontario Regulation 501/07 made under the Dental Hygiene Act, 1991. Invasive dental hygiene procedures are scaling teeth and root planing, including curetting surrounding tissue. Date: December 23, 2014 69 Bloor St. E, Suite 300, Toronto, ON M4W 1A9 t: 416-961-6234 ● tf: 1-800-268-2346 ● f: 416-961-6028 ● www.cdho.org 3