* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Epilepsy 101: Getting Started
Survey
Document related concepts
Drug design wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
Theralizumab wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Transcript
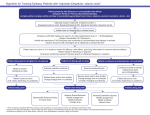
+ Module Three: Treatment of Epilepsy + Module Three: Objectives Upon completion of Module Three the participant will: Describe epilepsy the main treatment options for Identify factors essential in the selection of appropriate medications for epilepsy Review the indications for epilepsy surgery Discuss the benefits of dietary therapy for epilepsy + Treatment of Epilepsy Individuals with epilepsy have a variety of treatment options Medications are the first option and the mainstay of treatment for most people AEDs treat the symptoms, not the underlying disease Surgical procedures and implantable devices are also options that are considered if seizures persist Dietary therapies provide another treatment option in some patients when medicines don’t work + Decision to Treat with Medications Most patients with first time seizures are not placed on medications Medications to treat seizures are usually called antiepileptic drugs or AEDs Patients are treated if: two or more seizures abnormal imaging abnormal neurological exam abnormal EEG family history of seizures Treatment begins with one drug + Antiepileptic Drugs (AEDs) More accurately called ‘Anti-Seizure Drugs’ Goals of medication therapy: No seizures No side effects – tailor side effect profile to patient-specific factors Improvement in quality of life + Antiepileptic Medications (AED) Good oral absorption and bioavailability Most metabolized in liver but some excreted unchanged in kidneys 1st generation AEDs generally have more severe CNS sedation than newer drugs Drugs chosen based on mechanism of action, side effect profile, and impact on comorbid conditions, ie. migraine, depression Add-on therapy is used when a single drug does not completely control seizures + Ideal Characteristics for AEDs Few adverse effects High CNS penetrance Rapid onset of action No or few drug-drug interactions Long half-life for daily or twice a day dosing Intravenous route available Oral liquid preparations important for children and people with impaired swallowing Available strengths in different dosage Affordable, covered health insurance by + Things to keep in mind… Treatment with medication is successful for a large percentage of individuals, but at least 30 to 40% don’t respond to current AEDs Multiple dosing times for medications may lessen adherence Certain types of medications work best for certain forms of epilepsy + Medication Adherence The extent to which a person takes medication as prescribed Also referred to as compliance Using a self-management model, adherence is one aspect of medication-taking behaviors Missed AEDs are one of the most common reasons for breakthrough seizures Complex medication regimes, poor memory, and cost are barriers to adherence + Pharmacokinetics Absorption: How long it takes for medicine to be absorbed into the bloodstream Determined by route of intake, may be affected by food Absorption rate can vary for different medicines Meds that may affect rate of absorption should not be given at same time as AEDs, i.e. antacids Distribution: How the drug is distributed through the body AEDs with a high degree of protein binding tend to have more drug interactions + Pharmacokinetics Metabolism and Elimination: Drugs may be broken down in the liver and excreted through the kidneys AEDs metabolized by the liver tend to have more drug interactions Bioavailability: How much drug gets into the brain to work as intended. The net result of the absorption, distribution, metabolism, and elimination process + Drug Concentration: Establishing AED Doses Some drugs require a large initial dose to achieve a desired concentration in the body, called a ‘loading dose’ Some AEDs are tolerated better when started at slowly at low doses The dose necessary to MAINTAIN a desired concentration over time is called the ‘maintenance dose’ and may vary according to patient and drug specific factors + Laboratory Monitoring Serum drug levels serve as a guideline in determining therapeutic dosing Serum levels of newer drugs may not be as important since the therapeutic window for dosing is much larger Additional monitoring (i.e. liver function tests, CBC, or renal function) may be needed, depending on specific drug + Considerations for AED Choice Ability to give alone (monotherapy) or together with other AEDs (polytherapy) Side-effect Need for laboratory monitoring Drug-drug Cost profile and drug-food interactions and availability Patient’s ability to manage the medication(s) + General Instructions Patients must take medications as prescribed on a daily basis to maintain a therapeutic blood level to prevent seizures Patients should not abruptly stop medications – raises risk for seizure emergencies Factors that can influence how the drug gets into the body, works in the body, and is metabolized and eliminated can interfere with the serum blood drug levels and interact with other medications + 1st and 2nd Generation AED’s The oldest drugs used in the treatment of epilepsy include phenobarbital, introduced in 1912, and phenytoin (Dilantin), in use since 1938-these drugs are considered as 1st generation 2nd generation AED’s have been in place since the early 1990’s + 1st Generation AEDs 1857- Bromides 1912-Phenobarbital 1938-Phenytoin (Dilantin) 1954 1960- Primidone Ethosuximide (Zarontin) 1974-Carbamazepine (Tegretol) 1975 Clonazepam (Klonopin) 1978- Valproate (Depakote) + 2nd Generation AEDs 1993- Felbamate (Felbatol) 2000- Zonisamide (Zonegran) 1993- Gabapentin (Neurontin) 2005- Pregabalin (Lyrica) 1995-Lamotrigine (Lamictal) 2009- Lacosamide (Vimpat) 1997-Topiramate (Topamax) 2009- Rufinamide (Banzel) 2010-ACTH (Acthar) 2011- Clobazam (Onfi) 2012 – Ezogabine (Potiga) Tiagabine (Gabitril) 1999- Levetiracetam (Keppra) 2000- Oxcarbazepine (Trileptal + Generic Drugs Generic versions are available for many epilepsy medications While FDA states that generic medications are comparable to brand name AEDs, people have reported differences in seizure control and/or side effects during switches between generic to brand, or between different generic formulations Patients should discuss the use of generics with their provider For more information: AES consensus statement on generic drug substitution http://www.aesnet.org/go/press-room/consensusstatements/drug-substitution + Medication Side Effects Awareness of common side effects is important Side effects can be unpredictable What works well for one person, may not work well for the next Side effects can be dose dependent Often depends on person's chemistry and metabolism, height, weight, etc. Most common dose dependent side effects affect the CNS + Types of Side Effects • Dose-related: the higher the dose, the more • Idiosyncratic: Occurs irrespective of dose likely the effect • Common: drowsiness, irritability, nausea, clumsiness, imbalance, blurry or double vision • • Changes in appetite or weight change, osteopenia or osteoporosis, cosmetic effects, tremors, fatigue, cognitive effects, mood changes Allergic: i.e. rash, anaphylaxis + Serious Side Effects Prolonged fever Pinpoint bleeding Rash Weakness Nausea/vomiting Fatigue Severe sore throat Swollen glands Mouth ulcers Lack of appetite Easy bruising Abdominal pain + Drug Interactions How well an AED works may be affected by other medications a person is taking Interactions may occur between AEDs or between AEDs and other prescription or over-the-counter medications, for example, warfarin, antibiotics, and other commonly used medications + Rescue Treatments Used to stop prolonged or clusters of seizures Rectal diazepam gel (Diastat™) approved by FDA for out of hospital use by non-medical people PRN benzodiazepines are first line treatment and can be given in the home, community, ambulance or hospital. Autoinjectors and intranasal forms are being tested. Vagus nerve stimulator magnets - non-drug intervention for seizure first aid Rescue Treatments do not replace routine seizure first aid + Rescue Treatments General Instructions Rescue AEDs can be given by mouth, bucally, rectally or intravenously, depending on the setting and who is giving the AED. Patients should have specific instructions on when to use rescue AEDs or VNS magnet Include when to seek medical care and emergency services in seizure plans and protocols. Resources from Epilepsy Foundation: Seizure Action Plans for School Settings My Seizure Response Plans My Epilepsy Diary + When Seizures Do Not Respond to AEDs Patients whose seizures are not controlled after 2 or more trials of appropriate medications should be referred to the next level of care for appropriate evaluation and treatment. For example, Refer to a neurologist if seizures persist after 3 months of care by a primary care provider Refer to an epilepsy specialist if seizures persist despite treatment with general neurologist for 12 months + Epilepsy Surgery Indications Failure of AEDs to control seizures – refractory epilepsy Ability to identify focus of seizure generation in the brain Able to remove focus or operate safely Seizures are ‘disabling’ – consider impact of seizures on quality of life Benefits versus risks of surgery and of refractory epilepsy + Epilepsy Surgery Presurgical Evaluation Determine that seizures are refractory to AEDs Video EEG telemetry to localize seizures Scans to identify possible causes and location of seizure focus (CT, MRI, PET, SPECT, MEG) Multidisciplinary evaluations – medicine, nursing, psychiatry, social work, psychology Neuropsychological testing to evaluate cognitive function, assist in localizing seizure focus Wada test – to identify location of language and memory functions + Epilepsy Surgery Most common type of epilepsy surgery is resection in temporal or frontal lobe Outcomes of surgery depend on the type and location of surgery, whether all or most of the epileptogenic area was removed and other patient-specific factors + 30 Vagus Nerve Stimulation (VNS) Therapy Used as adjunctive therapy A programmable pulse generator implanted subcutaneously in upper left chest Electrode wrapped around the left vagus nerve Exact mechanism of action not known Stimulation-related side effects may include hoarseness, coughing and shortness of breath + VNS Therapy- Use of Magnet Stop side effects: Magnet temporarily stops stimulation Hold magnet over generator in chest for at least 6 seconds. Stimulation will not be delivered as long as the magnet is over the generator. To restart stimulation, remove the magnet. Seizure first aid: Magnet may activate additional burst of stimulation Swipe magnet over generator in chest for one second (“one one-thousand one”) Wait 60 seconds, then repeat, or as recommended in seizure action plan + Dietary Therapies for Epilepsy Ketogenic Modified Low Diet (KD) Atkins Diet (MAD) Glycemic Index Treatment (LGIT) + Dietary Therapies Indications and General Tips For people with refractory epilepsy, when medications don’t work or are not tolerable May allow reduction in AEDs if seizures can be controlled. Ketogenic diet is the most restrictive, may require a hospitalization and few days of fasting to start it. Difficult for older children and adults to tolerate Modified Atkins and Low Glycemic diets are less restrictive and easier to tolerate by many people