* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Endocrine Diseases
Survey
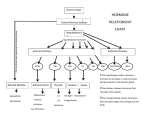
Document related concepts
Hormonal contraception wikipedia , lookup
Adrenal gland wikipedia , lookup
Polycystic ovary syndrome wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Xenoestrogen wikipedia , lookup
Menstrual cycle wikipedia , lookup
Hormone replacement therapy (female-to-male) wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Vasopressin wikipedia , lookup
Breast development wikipedia , lookup
Neuroendocrine tumor wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Transcript
Endocrine Diseases Pituitary Gland University of New England Physician Assistant Program J.B. Handler, M.D. 1 Abbreviations ACTHadrenocorticotropic hormone TSH- thyroid stimulating hormone LH- leutinizing hormone FSH- follicle stimulating hormone hCG-human chorionic gonodatropin ADH- antidiuretic hormone GH- growth hormone CO- cardiac output DI- diabetes insipidus IGF- insulin growth factor OCP- oral contraceptive pill LFT- liver function test AVP- arginine vasopressin DJD- degenerative joint disease SSRI- selective serotonin reuptake inhibitor 2 Pituitary Hormones Anterior Pituitary: Growth Hormone, Prolactin, ACTH, TSH, LH, FSH. Posterior Pituitary: Arginine Vasopressin (ADH, AVP), Oxytocin. Hypothalamus: Release of regulatory hormones, most of which stimulate release of pituitary hormones. Exception: Prolactin-release is inhibited by dopamine. 3 Hypopituitarism Hormone deficiencies may be single or multiple. Etiologies: Genetic defects, tumors (pituitary adenoma), autoimmune, trauma, irradiation, stroke/intracerebral hemorrhage, peri-partum (Sheehan’s syndrome- pituitary infarction following post partum shock or hemorrhage) 4 Hypopituitarism LH/FSH- Sex Hormones- If congenital: hypogonadism- delayed adolescence. If acquired as an adult: loss of secondary sex characteristics (beard, axillary and pubic hair, etc) libido, amenorrhea, infertility; low testosterone/estrogen. TSH- Thyroid Hormone- Hypothyroidism: weakness, cold intolerance, constipation, skin/hair changes, hyperlipidemia, wt. gain. 5 ACTH- Cortisol-Adrenal insufficiency: Weakness, fatigue, weight loss, hypotension. Growth Hormone-In adults: obesity, asthenia, decreased CO. In children-serious growth disturbance. Panhypopituitarism-lack all of the anterior pituitary hormones. 6 Lab, Diagnostics and Treatment Possibilities: ACTHCortisol hyponatremia, hypoglycemia; TSH free T4; LH, FSH Testosterone, Estradiol. MRI- Visualization of Pituitary neoplasms and other CNS pathology. Transphenoidal pituitary surgery (if tumor) followed by endocrine replacement therapy: LThyroxin, Testosterone or Estrogen, Cortisol, hGH. 7 Diabetes Insipidus Central: Deficiency of AVP/ADH Primary: Pituitary intact; familial forms (rare). Secondary: Damage to pituitary or pituitary stalk by tumor, surgery, anoxia. Nephrogenic: Inability of the kidneys to respond to ADH; congenital (lack ADH receptors) and acquired forms (pyelonephritis, post-obstructive, tubular interstitial disease, drug induced (demeclocycline, lithium), hypercalcemia, etc.). 8 Signs, Symptoms & Diagnostics Intense thirst, polyuria (2-20 L/d). Lab: Serum- hypernatremia; urine- low specific gravity. Other pituitary deficiencies may be present. 9 Diagnostics Vasospressin challenge: Desmopressin administered SC or intranasal results in dramatic decrease in urine volume in central DI; no response with nephrogenic DI. Differential Dx of polyuria/polydipsea: DI, Diabetes Mellitus, psychogenic polydypsia. Complications: Severe dehydration, hypernatremia. 10 Treatment Central DI: Partial deficiency may require no treatment other than fluids. Complete deficiency: Desmopressin (SC, IM, oral, intranasal); lowest effective dose to avoid hyponatremia. Nephrogenic DI: May respond to Indomethacin which increases renal sensitivity to AVP by blocking the action of prostaglandin E. 11 Acromegaly and Gigantism Excessive GH release, almost always from a pituitary adenoma. GH effects mediated by increased production of IGF-I in liver. These tumors often produce prolactin in addition to GH additional Sx (see below). 12 Signs and Symptoms Dependent on when the tumor develops. If before closure of epiphyses: Gigantism After epiphyseal closure: Acromegaly. Characterized by enlargement of the hands, jaw, feet; coarse facial features; bones of the skull enlarge; deep voice. 13 Pituitary Gigantism/Acromegaly Images.google.com Acromegaly “She has Man Hands”: J. Seinfeld, late 1990’s Images.google.com Signs and Symptoms Associated findings: Hypertension, cardiomegaly (dilated cardiomyopathy), insulin resistance/diabetes, DJD. If untreated, progressive cardiovascular morbidity and premature death. Hypogonadism reflects co-secretion of prolactin (see below) or pituitary compression with decreased LH/FSH. 16 Lab and Diagnostic Findings Bloodwork (Following an overnight fast): serum IGF-I (5x nl with Acromegaly), prolactin, glucose; all may be elevated. TSH/Thyroxin if low, suggests additional pituitary pathology. Glucose challenge post fast- Elevated GH levels help confirm the diagnosis (should normally be < 1ng/mL). MRI- Usually identifies a pituitary adenoma. 17 Pituitary Tumor Images.google.com 18 Treatment of Acromegaly Transphenoidal microsurgery, which may result in transient or permanent hypopituitarism. Octreotide-a somatostatin (somatotropin releaseinhibiting factor) analog. Suppresses GH secretion; used in patients who continue to have excessive GH release post-op; very expensive; injectedshrinks some tumors – Dopaminergic agents (cabergoline, oral) useful especially if tumor co-secretes prolactin shrinks some tumors. – Pegvisomant- GH receptor antagonist, new. 19 Hyperprolactinemia Prolactin induces lactation during pregnancy (along with estrogen and progesterone). Control of prolactin production is inhibitory, mediated by dopamine. Etiologies: Pituitary microadenoma (may also produce GH), drugs (SSRI’s, thiazides, Cimetidine, Tricyclics, OCP, others); hypothyroidism, renal failure and cirrhosis. 20 Signs and Symptoms High prolactin levels suppress GnRHLH/FSH, resulting in hypogonatropic hypogonadism. Females: Pre-menopausal woman develop galactorrhea, oligo/amenorrhea and infertility, decreased libido, vaginal dryness. Males: Decreased libido, erectile dysfunction, gynecomastia, but no galactorrhea. 21 Lab and Diagnostic Findings Baseline labs should include hCG, TSH, Free Thyroxine, Creatinine and BUN, LFT’s and Prolactin levels. In the absence of pregnancy and renal failure, a Prolactin level >250ng/mL is highly suspicious/diagnostic of Prolactinoma. Imaging- MRI 22 Treatment DC offending drug if present. Correct other possible etiologies. Microprolactinomas grow very slowly and patients with mild symptoms can be followed without intervention. 23 Treatment With symptoms of hypogonadism/infertility or larger tumors: Dopamine agonists (Cabergoline, Bromocriptine) can successfully treat symptoms, correct amenorrhea and galactorrhea, and shrink the tumor. Transphenoidal pituitary surgery reserved for individuals with large macroadenomas that abut/compress the optic chiasm. 24