* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Poultry Diseases Transmissible to Man
Foodborne illness wikipedia , lookup
Trichinosis wikipedia , lookup
Henipavirus wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Sarcocystis wikipedia , lookup
Neonatal infection wikipedia , lookup
Onchocerciasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Hepatitis C wikipedia , lookup
West Nile fever wikipedia , lookup
Tuberculosis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Hepatitis B wikipedia , lookup
Marburg virus disease wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Leptospirosis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Influenza A virus wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
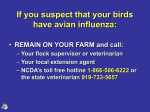
Poultry Diseases Transmissible to Man: Interface of Poultry Health and Public Health P. A. Dunn Animal Diagnostic Laboratory, Pennsylvania State University 2012 Northeastern Conference on Avian Diseases, PA Poultry Sales and Service Meeting Context: Poultry as a Food Animal • Starvation is 100% lethal • Malnutrition is 100% debilitating – Decreased productivity – Increased concurrent disease • Hunger = #1 health problem in the developing world – Deaths from lack of food > deaths from war + malaria + TB + AIDS – 25,000 deaths per day= 9 million per year = population of NYC Context: Poultry as a Food Animal • POULTRY - THE ULTIMATE FOOD ANIMAL – – – – Across nations, cultures, religions “Easy keepers” in subsistence; low inputs; low footprint High quality protein Terminal (meat); Non-terminal (egg) • Socioeconomic, (geopolitical) factors determine – – – – Food security (stabilizing), food insecurity (unstabilizing) Availability of animal protein How people live with / use animals Perception of risk: benefit • Risk (zoonosis) = low : Benefits (food source) = high Zoonosis • “An infection or infestation shared by man and lower vertebrate animals” • People concerned about diseases they might “catch” due to association with non-human “animals” • Diseases of Public Health Significance (DPHS) – Context, perspective is important • Relatively few poultry zoonoses (dismissive vs non-alarmist, realistic) – Human to human >>> mammal to human >>> poultry to human > fish, reptiles, amphibians >>> invertebrates • But important (alarmist vs practical awareness) – human health is paramount – Don’t miss Very Few Poultry Infectious Diseases Transmissible to Humans… • Most not directly transmissible to humans under normal conditions • Most successful pathogens are highly adapted to physiology, anatomy of specific hosts – Major differences between avian and mammalian – Cell receptor types, body temperature, etc. Very Few Poultry Infectious Diseases Transmissible to Humans… • Indirectly much more common – Food-borne: microbes, microbial toxins in / on the product originating from the bird or carcass, or contaminated from external source • • • • Salmonellosis, campylobacteriosis, listeriosis Many are not causing clinical disease in bird, no lesions at processing Food prep hygiene; cooking to proper temps. Inadvertent hand to mouth transfer after handling bird, secretions, excretions – Children handling baby chicks – Hygiene during, after handling of birds – Insect-vectored from infected bird (usually wild bird) to man: arbovirus (WNV - transmitted by mosquito) • Chickens, turkeys relatively resistant to WNV, not important reservoir But, Important to Recognize… Stakes are High • “When you hear hoof beats, don’t look for zebras.” • “Don’t forget to look for zebras.” • Investigate the more common conditions, but keep zoonoses in mind. • One health concept: veterinarians and physicians, animal and medical scientists • Rural vs urban populace, medicine; several generations “off the farm”; includes patients and doctors • “My chickens are sick. Are my kids, pets, etc., safe? Can we eat the eggs, meat?” Diseases of Poultry, 12th edition (2008), Y. M Saif, editor-in chief • 1324 pages; > 9 lbs. • 6 sections; 33 chapters; 93 subchapters (topics) • Public health significance– 8/33 chapters; 12/93 subchapters – Most limited, rare, +/- associated with compromised immune systems • Next edition- separate chapter devoted to DPHS Diseases of Poultry, 12th ed. Disease Newcastle Disease Virus Human Ailment Eye Infection Transmission Lab accident/ Poultry vaccines Avian Influenza Eye, Respiratory, Systemic (HP) Handling infected birds/Aerosols Arbovirus Neurologic, systemic Mosquito bite Pullorum Disease Enteritis Foodborne Paratyphoid/Salmonella Gastrointestinal Foodborne Campylobacteriosis Gastrointestinal Foodborne Necrotic Enteritis/ C. perfringens Types A & C Gastrointestinal Foodborne Staphylococcosis Gastrointestinal Foodborne Erysipelas Local (cutaneous) infection Handling infected birds Avian Intestinal Spirochetosis Gastrointestinal Unhygienic conditions; contaminated drinking water Avian Tuberculosis Pneumonia Handling infected birds/Aerosols Avian Chlamydiosis Pneumonia, systemic Handling infected birds/Aerosols 5 Diseases of Poultry • Avian influenza (orthomyxovirus)- covered by Dr. Perez – Often on ddx list due to regulatory status; routine diagnostics • Newcastle disease (paramyxovirus) – Often on ddx list; routine diagnostics • Chlamydiosis – Not often on ddx list for poultry; lesions overlap with other diseases; often need special diagnostics • Erysipelas – Often (?) on ddx list; lesions of acute septicemia- lesions overlap with other septicemias; routine diagnotics • Tuberculosis – Not often on ddx list; lesions should be suggestive; need special diagnostics to confirm Avian Influenza • Avian Influenza, 2008, D.E. Swayne, editor • 605 pages, 25 chapters: 1 chapter (31 pp) “Public Health Implications of Avian Influenza Viruses” by N. J. Cox and T. M. Uyeki • LPAI- very few cases, very limited illness (conjunctivitis), most linked to direct contact with poultry • HPAI, especially H7N3, H7N7, H5N1- last 15 years; serious illness and deaths General Approach to Control Poultry AI Limits Zoonotic Potential: Several Steps Ahead • Limiting AIV from adapting from waterfowl, shorebird strains to gallinaceous strains – Live Bird Market System control strategies – Periodic complete sell down, C&D, inspection; monitoring supply flocks, dealers, haulers; crate washing… • Block AIV from entering flocks (biosecurity) – If AI enters, most likely LPAI, might be H5, H7 Several Steps Ahead… • Block H5, H7 LPAI from mutating to HPAI by quick detection, containment, elimination of infection (depop. or controlled marketing) +/strategic vaccination • Enhanced biosecurity, comprehensive and strategic monitoring programs at every step • As a few HPAI can and do cause serious human infections, blocking the emergence of these in poultry is effective public health strategy Newcastle Disease (APMV-1) in Avian Spp. • Chickens, turkeys, pigeons, many other species (cormorants, etc.) • Lentogenic (non-exotic) in US, Canada • Mild respiratory signs, secondary E. coli infections, air sacculitis • Egg production drops, shell quality problems • Diagnosed by gross, micro, PCR, VI, serology • Vaccination widely practiced and highly effective: modified live, killed, recombinant Exotic Newcastle Disease (END) Newcastle Disease (APMV-1) in Humans • Risks to people: – Handling, administering live vaccines – Performing post mortem exams on actively infected birds – Working with, isolating, concentrating virus in the lab • Localized infection- conjunctivitis (“pink eye”); 5- 10 days duration; resolves completely • Uncomfortable; cosmetically undesirable • Topical eye drops or ointments to reduce inflammation, discomfort, secondary bacterial infections • Wear gloves, lab goggles/ safety glasses / shields; washing hands after handling virus or vaccine; avoid touching hands to eyes; avoid spraying, splashing solutions into face, eyes. Conjunctivitis Avian Chlamydiosis- Chlamydophila psittaci infection in Avian spp. • Psittacosis, parrot fever, ornithosis • Specialized bacterium- obligate, intracellular • Pet bird species (psittacines = parrot-type)very common- source of most human infections; also wild bird reservoirs esp. pigeons (gulls, ducks, herons, egrets) • Poultry- turkeys; ducks, pheasants (occ.) chickens (rare) Chlamydiosis in Turkeys • Strain differences in C. psittaci • Mild – Decreased feed intake; loose, greenish droppings; 1 -4% mortality • More virulent • Clinical signs as above; weight loss; abrupt egg production drop; 1030% mortality • Lesions: – Fibrinous exudates over heart +/- air sacs; enlarged congested spleen, liver (25% air sac condemns in NC turkey flock associated with chlamydiosis in processing plant workers- 1989) – Similar to E. coli infections, other bacteremias Chlamydiosis in Turkeys • Diagnose by molecular methods (PCR); isolation (cell cultures, eggs); presumptive Dx by histopathology, special stains to reveal elementary bodies, IHC • Reportable disease • Treat with chlortetracycline (400 gms CTC/ ton) very effective at controlling infections; reducing shed of infective particles before processing • Grow-out on range – increased risk of exposure Chlamydiosis Lesions, Organism Chlamydiosis in Humans • Flu-like symptoms: fever, chills, headache, weakness, coughing associated with atypical pneumonia; +/- joint pain, stomach cramps, diarrhea • Incubation period 4- 19 days; mean duration of illness 9 – 10 days • Hospitalizations, (deaths) with some frequency • Tetracycline- class antibiotics Chlamydiosis in Humans • Risk to people: – Workers at turkey processing plant • Aerosolized infectious particles • Kill- pick, evisceration most common +/- other areas including further processing • Over past 60+ years: TX, MO, NE, OH, MN, NC – Workers in infected turkey flocks • Prevent exposure to infected turkeysdiagnose, medicate, controlled processing Erysipelas in Avian Spp. • Erysipelothrix rhusiopathiae infection • Turkeys >>> pheasants, ducks, geese, wild birds >>> chickens (rare) • Market turkeys, breeders • Ranged flocks >>> housed • Infected soil, enters through breaks in skin; pecking and fighting; artificial insemination Erysipelas in Turkeys • Clinical signs – Acute: sudden deaths – Chronic: depression, lameness • Lesions – Whole carcass congestion; enlarged, dark liver, spleen; hemorrhages on heart, other organs; reddened swollen wounds on head, neck, vent – Similar to other acute bacteremias Erysipelas Lesions Erysipelas in Turkeys • • • • • Diagnosis- routine bacteriologic culture Treatment- penicillin Remove sick and dead promptly Vaccines in at-risk flocks Beak-trimming, de-snooding, careful AI technique • Move from infected range (don’t range) Erysipelas in Humans • Risk to people – Large numbers of ER bacteria in dying birds, carcasses – Handling carcasses, performing post mortem exams – Turkey handlers, insemination crew • Usually localized: Erysipeloid = painful, hot swelling with dark center of skin and underlying tissue at site of entry – Resolves completely in a few weeks with treatment • Rarely systemic- arthritis; endocarditis, encephalitis; death • Penicillin, other antibiotics effective against Gram positives • Avoid contact with bare skin (scratches, etc.); gloves, double sets of gloves “Tuberculosis”- Avian TB • Mycobacterium avium sbsp. avium infection • Different from M. tuberculosis, M. bovis = common agents of human TB • No longer present in commercial poultry in US; sporadic in chickens > 2- 3 years; older ducks, geese, game birds, pigeons, pet birds, zoo, aviary spp., wild birds; very rare in turkeys Mycobacteriosis in Poultry • Progressive debilitation, chronic weight loss, decreased egg production; death • Granulomatous lesions in liver, spleen, intestine, bone, lung – Can look like fungal granuloma, coligranuloma, tumor, pullorum disease, histomoniasis • Diagnose by histopathology (acid-fast stain), special culture (slow), PCR • No effective treatment; no vaccine • Control by: modern confinement, all in /all out management; < 2 -3 years of age. Granulomatous Lesions in Liver Gamebird Case • 2 year old chukar partridge breeders • Lethargy, weight loss, increased mortality • Enclosed house, raised wire floors; in use for “many years” • Ventilation “not the best” • Overgrown beaks; unkempt plumage • Decreased body weight • Multiple tan/gray masses in lungs +/- serosa of gizzard, intestines M. avium in Mammals (Non-primate) • Swine, rabbits, mink > sheep, llama • Pets (cat, dog) very resistant • Reactor cattle to tuberculin test – React on caudal skin fold test – Retest by paired cervical method M. avium in Humans • First documented case in U.S.- 1930 • Risk to people: Humans relatively resistant – Increased incidence in immunosuppressed people • HIV/ AIDS; immunosuppressive chemotherapy; leukemia • Opportunistic • Ubiquitous- hard to avoid all contact with the organism • most human isolates are more closely related to pig isolates than bird isolates (using molecular methods) • M. avium serovar 2, the most common chicken serovar, is rarely isolated from people • Most infections more likely to be human- to- human contact than bird- to- human – Although serovar 1 is common in wild birds and in AIDs patients Environmental Sources of M. avium • Aerosolized water • Piped hot water systems (including household and hospital water supplies) • Bathrooms • House dust • Soil • Birds • Farm animals • Cigarette components (eg, tobacco, filters, paper) M. avium in Humans • Primarily pulmonary infection: cough; fever, fatigue, weight loss, diarrhea; disseminated infection to lymph nodes, bone marrow, tendons, liver, spleen, CNS • More resistant (than M. tuberculosis, M. bovis) to commonly used anti tuberculosis drugs • Combination of 2- 3 antimicrobials for 12 months Miscellaneous • Parasites – Internal parasites very host specific • Protozoa, helminths • Most won’t cross into other avian species let alone into mammals – External • Mites, lice, etc. • Don’t colonize humans; but can board, bite, irritate temporarily • Non-infectious- irritants in poultry house environment – Allergies-dander, feathers, litter – Ammonia gas, dust – Masks, respirators Cautions, Trends • Free range systems for poultry (local food, pastured poultry) – May increase some poultry diseases with zoonotic potentialincreasing public health risk • Antibiotic – free, organic production – Ditto as above • Molecular techniques to detect and identify pathogens – Very helpful for better, faster detection – Crucial for modern epidemiology, specific strain identification – But detection does not equate with productive infection, presence of disease; results can be misleading – Context is important; must be medically relevant Public Health Benefits from Controlling Poultry Diseases- Direct and Indirect • Restrictions on poultry workers keeping pet birds – prevents major risk of chlamydiosis in people • Keeping “embryo egg” layer flocks healthy – ensures adequate supply of human flu vaccine – prevents seasonal flu in people • Preventing HPAI in poultry – prevents serious, fatal “bird flu” in people • Correctly & promptly diagnosing potential zoonoses – limits risk, exposure; guides proper medical treatment • Supplying poultry meat and eggs - safe, affordable, high quality protein – provides better nutrition for people Poultry Diseases with Zoonotic Potential ….. • Remain vigilant to the ones we know. • Look out for “new” ones. • When you hear hoof beats, don’t forget to look for zebras. • People should not fear association with poultry as a significant human health risk under most circumstances. Newsweek, September 24, 2012 No Chickens? “When we try to pick out anything by itself, we find it hitched to everything else in the Universe” – John Muir