* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Circulatory System
Survey
Document related concepts
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Artificial heart valve wikipedia , lookup
Jatene procedure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Congenital heart defect wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
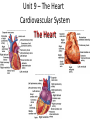
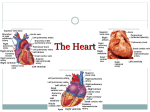
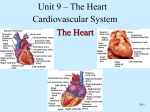
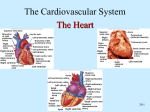
Collins I- 4 lines Describe three things you know about the heart Agenda—5/6/13 • Circulatory notes • Heart diagram The Circulatory System The Heart, Blood Vessels, Blood Types The Closed Circulatory System •Humans have a closed circulatory system, typical of all vertebrates, in which blood is confined to vessels and is distinct from the interstitial fluid. –The heart pumps blood into large vessels that branch into smaller ones leading into the organs. –Materials are exchanged by diffusion between the blood and the interstitial fluid bathing the cells. The Cardiovascular System •Three Major Elements – Heart, Blood Vessels, & Blood –1. The Heart- cardiac muscle tissue –highly interconnected cells –four chambers •Right atrium •Right ventricle •Left atrium •Left ventricle •Superior Vena Cava •Right Atrium •Tricuspid Valve •Right Ventricle •Pulmonary Semilunar Valve •Lungs •Pulmonary Vein •Left Atrium •Bicuspid Valve •Left Ventricle •Aortic Semilunar Valve •Aorta •To the bodies organs & cells Pathway of the blood Circuits •Pulmonary circuit –The blood pathway between the right side of the heart, to the lungs, and back to the left side of the heart. •Systemic circuit –The pathway between the heart and the body cells The Cardiovascular System 2. Blood Vessels -A network of tubes –Arteriesarterioles move away from the heart •Elastic Fibers •Circular Smooth Muscle –Capillaries – where gas exchange takes place. •One cell thick •Serves the Respiratory System –VeinsVenules moves towards the heart •Skeletal Muscles contract to force blood back from legs •One way valves •When they break - varicose veins form The Cardiovascular System 3. The Blood A. Plasma Liquid portion of the blood. Contains clotting factors, hormones, antibodies, dissolved gases, nutrients and waste The Cardiovascular System •The Blood B. Erythrocytes - Red Blood Cells –Carry hemoglobin and oxygen. Do not have a nucleus and live only about 120 days. –Can not repair themselves. The Cardiovascular System •The Blood C. Leukocytes – White Blood cells –Fight infection and are formed in by the bone marrow –Five types – neutrophils, lymphocytes, eosinophils, basophils, and monocytes. The Cardiovascular System The Blood D. Thrombocytes – Platelets. –These are cell fragment that are formed in the bone marrow –Clot Blood by sticking together – via protein fibers called fibrin. Disorders theblood, Circulatory System • Anemia - lack of ironof in the low RBC count • Leukemia - white blood cells proliferate wildly, causing anemia • Hemophilia - bleeder’s disease, due to lack of fibrinogen in thrombocytes • Heart Murmur - abnormal heart beat, caused by valve problems • Heart attack - blood vessels around the heart become blocked with plaque, also called myocardial infarction Unit 9 – The Heart Cardiovascular System The Heart Functions of the Heart • Generating blood pressure • Routing blood – Heart separates pulmonary and systemic circulations • Ensuring one-way blood flow – Heart valves ensure one-way flow • Regulating blood supply – Changes in contraction rate and force match blood delivery to changing metabolic needs Size, Shape, Location of the Heart •Size of a closed fist •Shape –Apex: Blunt rounded point of cone –Base: Flat part at opposite of end of cone •Located in thoracic cavity in mediastinum Heart Cross Section Pericardium Heart Wall • Three layers of tissue – Epicardium: A serous membrane, smooth outer surface of heart – Myocardium: Middle layer composed of cardiac muscle cells and is responsible for heart contracting – Endocardium: Smooth inner surface of heart chambers Heart Wall External Anatomy •Four chambers –2 atria –2 ventricles •Auricles •Major veins –Superior vena cava–Pulmonary veins- •Major arteries –Aorta –Pulmonary trunk External Anatomy Coronary Circulation Heart Valves •Atrioventricular –Tricuspid –Bicuspid or mitral •Semilunar –Aortic –Pulmonary •Prevent blood from flowing back Heart Valves Function of the Heart Valves Blood Flow Through Heart Systemic and Pulmonary Circulation Heart Skeleton •Consists of plate of fibrous connective tissue between atria and ventricles •Fibrous rings around valves to support •Serves as electrical insulation between atria and ventricles •Provides site for muscle attachment Cardiac Muscle • • • • • Elongated, branching cells containing 1-2 centrally located nuclei Contains actin and myosin myofilaments Intercalated disks: Specialized cell-cell contacts Desmosomes hold cells together and gap junctions allow action potentials Electrically, cardiac muscle behaves as single unit Conducting System of Heart Electrical Properties • Resting membrane potential (RMP) present • Action potentials – Rapid depolarization followed by rapid, partial early repolarization. Prolonged period of slow repolarization which is plateau phase and a rapid final repolarization phase – Voltage-gated channels Action Potentials in Skeletal and Cardiac Muscle SA Node Action Potential Refractory Period • Absolute: Cardiac muscle cell completely insensitive to further stimulation • Relative: Cell exhibits reduced sensitivity to additional stimulation • Long refractory period prevents tetanic contractions Electrocardiogram • Action potentials through myocardium during cardiac cycle produces electric currents than can be measured • Pattern – P wave • Atria depolarization – QRS complex • Ventricle depolarization • Atria repolarization – T wave: • Ventricle repolarization Cardiac Arrhythmias • Tachycardia: Heart rate in excess of 100bpm • Bradycardia: Heart rate less than 60 bpm • Sinus arrhythmia: Heart rate varies 5% during respiratory cycle and up to 30% during deep respiration • Premature atrial contractions: Occasional shortened intervals between one contraction and succeeding, frequently occurs in healthy people Alterations in Electrocardiogram Agenda 4/30/12---Day 2 • Hand in projects • Cardiac Cycle Notes and interactive lesson Collins I 6 lines • Explain the path the blood takes through the heart starting with the Superior and Inferior vena cava… Cardiac Cycle • Heart is two pumps that work together, right and left half • Repetitive contraction (systole) and relaxation (diastole) of heart chambers • Blood moves through circulatory system from areas of higher to lower pressure. – Contraction of heart produces the pressure Cardiac Cycle SSR • First 10 minutes Events during Cardiac Cycle Heart Sounds • First heart sound or “lubb” – Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole • Second heart sound or “dupp” – Results from closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole, lasts longer • Third heart sound (occasional) – Caused by turbulent blood flow into ventricles and detected near end of first one-third of diastole Location of Heart Valves Mean Arterial Pressure (MAP) • Average blood pressure in aorta • MAP=CO x PR – CO is amount of blood pumped by heart per minute • CO=SV x HR – SV: Stroke volume of blood pumped during each heart beat – HR: Heart rate or number of times heart beats per minute • Cardiac reserve: Difference between CO at rest and maximum CO – PR is total resistance against which blood must be pumped Factors Affecting MAP Regulation of the Heart • Intrinsic regulation: Results from normal functional characteristics, not on neural or hormonal regulation – Starling’s law of the heart • Extrinsic regulation: Involves neural and hormonal control – Parasympathetic stimulation • Supplied by vagus nerve, decreases heart rate, acetylcholine secreted – Sympathetic stimulation • Supplied by cardiac nerves, increases heart rate and force of contraction, epinephrine and norepinephrine released Heart Homeostasis • Effect of blood pressure – Baroreceptors monitor blood pressure • Effect of pH, carbon dioxide, oxygen – Chemoreceptors monitor • Effect of extracellular ion concentration – Increase or decrease in extracellular K+ decreases heart rate • Effect of body temperature – Heart rate increases when body temperature increases, heart rate decreases when body temperature decreases Baroreceptor and Chemoreceptor Reflexes Baroreceptor Reflex Chemoreceptor Reflex-pH Effects of Aging on the Heart • Gradual changes in heart function, minor under resting condition, more significant during exercise • Hypertrophy of left ventricle • Maximum heart rate decreases • Increased tendency for valves to function abnormally and arrhythmias to occur • Increased oxygen consumption required to pump same amount of blood