* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Staphylococci and Streptococci
Survey
Document related concepts
Gastroenteritis wikipedia , lookup
Human microbiota wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Infection control wikipedia , lookup
Urinary tract infection wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Antibiotics wikipedia , lookup
Anaerobic infection wikipedia , lookup
Triclocarban wikipedia , lookup
Neonatal infection wikipedia , lookup
Transcript
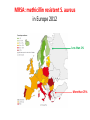
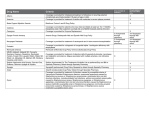
Semmelweis University Institute of Medical Microbiology Staphylococci and Streptococci Dr. Béla Kocsis 2014.10.14 Gram-positiv cocci Staphylococci and Streptococci Katalase-reaction microscopic view positive negative Streptococcaceae Family Micrococcaceae Family Nitrofurantoin Susceptibility Streptococcus genus Positiv (susceptible) Negativ (Resistant) Staphylococcus genus Micrococcus genus Gram-positiv cocci Staphylococci Micrococcaceae Family Micrococcus genus: apathogen Coagulase test Staphylococcus genus: coagulase positiv: S. aureus coagulase negativ: S. epidermidis, S. haemolyticus, S. saprophiticus, S. hominis Staphylococcus aureus 1) Microscopic morphology: Gram positive, 1 µm cocci arranged in grape-like clusters Staphylococcus aureus 2) Cultivation • facultative anaerob • In bouillon: homogenous turbidity • agar plate: 2-3 mm in diameter, circular, golden yellow colonies • pigment in non diffusable, fat soluble stains only the colonies • S. aureus AU referes to gold • On blood agar: -haemolysis • selective cultivation method: 7.5% NaCl Staphylococcus aureus 3) Biochemical feature catalase + coagulase + Exocoagulase (free coagulase): • enzyme produced and released by the S. aureus, • binds to serum factor immunoglobulin, this complex can convert fibrinogen to fibrin • detecting: coagulase tube test Endocoagulase: „clumping factor” (bound coagulase): • on the bacterial surface, • direct convertion of fibrinogen to fibrin • detecting: slide agglutination, latex-agglutination Staphylococcus aureus 3) Biochemical feature coagulase tube test latex-agglutination Staphylococcus aureus 4) Virulence factors Staphylococcus aureus 4) Virulence factors on the bacterial cell surface polysaccharide capsule slime layer (binds bacteria to catheters, grafts) teicholic acid, lipoteicholic acid (mediates the attachment of staphylococci to mucosal surfaces) adhesive proteins (collagene-, laminin-binding protein) clumping factor: endocoagulase mimikry by the fibrin layer macrophages can not reach them protein A (unique affinity for binding to the Fc fragment of immunoglobulin, prevents antibody-mediated immune clearance of S.aureus) Staphylococcus aureus 4) Virulence factors: exoenzymes exocoagulase, fibrinolysin Clot formation and lysis of fibrin DNase, hyalurinidase, phosphatase, lipase Invasivity in different tissues Staphylococcus aureus 4) Virulence factors: exotoxins • Toxic Shock Syndrome Toxin (TSST-1)septic state , high fever, multi organ failer • Staphylococcus enterotoxin (SE) leads to diarrhoeae and vomiting, toxico-infection • exfoliative toxin split the intercellular bridges in the stratum granulosum epidermis Staphylococcus aureus 4) Virulence factors: Superantigen exotoxin Superantigens bind to T helper on the T cell receptor V β site leads to proliferation of T cells and overproduction of cytokins: TNF- β, IFN- γ, IL-2. The patients get into septic state : hypotension, shock, mulit-organ-failer Staphylococcus aureus 4) Virulence factors: cytotoxins -haemolysin - haemolysin - haemolysin -haemolysin Leukocidin lysis of erythrocytes lysis of leukocytes Pore forming on the cell surface Clinial pictures Source of infection : 5-10 % of population carry S. aures in the nose, nasopharynx Way of transmission by respitory droplets or direkt contact Purulent infections on the site of infection of the skin folliculitis, furunculus, carbunculus, woundinfections , otitis media, mastoiditis, mastitis Invasive Infections pneumonia, bakteraemia, sepsis, meningitis, ostitis, osteomyelitis, endocarditis Toxin medaited infections Gastroenteritis, TSS, Pemph. neonat, Scales Skin Syndrom Local skin infections Impetigo Folliculitis Furuncle Carbuncle Deep purulent infections • • • • • Osteomyelitis Mediastinitis Peritonitis Meningitis, Subduralempyema, Abscesse formation in all parenchymal organ Fig. 8.27 – Septic arthritis. Erythema and swelling of the left ankle joint in a young girl with staphylococcal sepsis. By courtesy of Mr. N.St.J.P. Dwyer Septic arthritis Arthrotomia, pus after Gram staining Gram positive cocci in clusters Therapy of Staphylococcus aures infections Antibiotic treatment β-lactam antibiotics with β-lactamase Inhibitors eg.: amoxicillin + clavulanic acid Therapy of Staphylococcus aures infections Penicillin group of antibiotics (as all β-laktams) Inhibit the peptidoglycan synthesis (cellwall synthesis) Target molecula PBP (Pencillin Binding Protein) a transpeptidase, responsible for the cellwall synthesis Peptidoglycan of Cell wall : NAM: N-acetyl-muramin acid : NAG: N-acetyl-glukosamin NAM NAG Ala-Glu-Lys-D-Ala-D-Ala PBP β-lactam antibiotics NAM Ala-Glu-Lys-D-Ala-D-Ala NAG beta-lactamase (penicillinase) production NAM Ala-Glu-Lys-D-Ala-D-Ala Resistence to beta-lactams Beta-lactamase production (penicillinase production) • Resistence only to Penicillin group • • Penicillin-binding Proteine (PBP) – Struktur modifing Resistance to all beta-lactame antibiotics: – Penicillins – Cephalosporins – Karbapenems – monobactams – Beta-laktamase Inhibitors MRSA: Methicillin Resistant S. aureus Therefore the treatment: amoxicillin + clavulanic acid Penicillin derivative Penicillinase inhibitor Therefore the treatment is based on antibiogramm: Antibiotic with different target molecules : Vancomycin Linezolid Mupirocin Clindamycin Daptomycin MRSA = methicillin resistent S. aureus Methicillin belongs Penicillin group of antibiotics (β-laktam) Inhibtion of Peptidoglycan synthesis Target molecula PBP (Pencillin Binding Protein) Target molecule mutation PBP’2a modified target conferes resistance to all β-lactam antibiotics Peptidoglycan of Cell wall NAM NAG NAM Ala-Glu-Lys-D-Ala-D-Ala PBP’2a Ala-Glu-Lys-D-Ala-D-Ala NAG NAM Ala-Glu-Lys-D-Ala-D-Ala Uneffective β-lactam Antibiotics MRSA: methicillin resistent S. aureus in Europe 2012 Less than 1% More than 25% VRSA = vancomycin resistent S. aureus Vancomycin effective agent against MRSA Inhibition of Cell wall synthesis Targetmolecule is D-Alanin in Murein Targer modification (D-Ala-lactate) leads to resistance VRSA Peptidoglycan of Cell wall NAM Ala-Glu-Lys-D-Ala-D-Ala Vancomycin Ala-Glu-Lys-D-Ala-D-Ala Vancomycin Ala-Glu-Lys-D-Ala-D-Ala Vancomycin NAG NAM NAG NAM Coagulase-negativ Staphylococci Coagulase-negativ Staphylococci • Belong to the normalflora of the skin and mucosalayers • Fakultative Pathogens S. epidermidis S. hominis S. hemolyticus S. saprophyticus Staphylococcus epidermidis • Morphology: Gram-positve cocci in grape-like clusters • Cultivation: white pigment without hemolysis • Biochemical features – Katalase + – Koagulase – Mannit - Staphylococcus epidermidis • Belongs to the normalflora of the skin • On the intact skin causes no infection • On plastic instruments biofilm formation – exopolysaccharide – Matrixproteins (Fibrin, Fibrinogen) Attachment , colonisation Bloodstream infection Staphylococcus epidermidis Therapy: plastic devices should be removed Therapy based on antibiogram S. epidermidis resistance to beta-lactams: MRSE : methicillin resistant S. epidermidis Resistance to other group of antibiotics too: vancmomycin, linezolid Staphylococcus saprophyticus 1) Microscopic morphology: Gram-positive cocci grape-like clusters 2) Cultivation: no hemolysis on blood agar 3) Biochemical : coagulase negative, novobiocin resistent, urease positive! Clinical features: Belongs to the skin normalflora mainly on the genitals cystitist („honeymoon cystitis”) in young sexualle active women S. saprophyticus can bind to the uroepithel and by the urease activity NH3 will irritate the mucosalayer Staphylococcus haemolyticus Staphylococcus hominis 1) Microscopic morfology: Gram-positiv cocci grape-like clusters 2) cultivation: white colonies weak or no hemolysis 3) Biochemical features : novobiocin susceptible Belong to the normal flora of the skin : Nosocomial pathogen biofilm production on catheter, canuls, plastic devices, tubes of intubation Mucus layer damages help the invasion to the bloodstream bacteraemia and sepsis Streptococci Gram positive cocci : Streptococcus genus Morphology: Gram positive cocci 1m in diameter arranged in chains Cultivation: demanding bacteria blood agar media (-, -, - haemolysis) 1 mm in diameter roundish, tiny needletip colonies Biochemical feature: catalase negative Classification of the Streptococcus genus 1. Haemolysis: a) - haemolysis: Streptococcus pyogenes, S. agalactiae b) -haemolysis: S. pneumoniae c) non haemolytic: S. lactis, Enterococci 2.Lancefield grouping: according to the polysaccharide “C” in the cell wall serogroups: A, B, C, D, F, G human infections “A” group: S. pyogenes “B” group: S. agalactiae “D” group: Enterococcus faecalis Classification of the Streptococcus genus 3. “M” protein in the cell wall: • serotypes S. pyogenes > 90 serotypes • in certain diseases different serotypes are characteristic: • e.g.: serotype 10 – scarlet fever; • serotype 2, 4, 12, 49 – acut glomerulonephritis • (nephritogen strains) 4. 16 S rRNA sequence coding DNA sequence: • 6 clusters: anginosus, pyogen, mitis, salivarius, bovis, mutans Streptococcus pyogenes 1) Microscopic morphology: Gram positive cocci 1m in diameter arranged in long chains • capsule is composed of hyaluronic acid Streptococcus pyogenes 2) Cultivation: demanding bacteria (vitamin B) blood agar media: -haemolysis 1 mm, circular, tiny needletip colonies S. pyogenes on blood agar Streptococcus pyogenes 3) Biochemical features: Antigen structure: Lancfield group “A” according to M protein it is grouped in serotypes Streptococcus pyogenes 4) Virulance factors I. On the cell surface: lipoteicholic acid, F-protein, capsule II. Exotoxin: erythrogenic toxin – scarlet fever (capillar toxin) Spe A, B, C, F – streptococcal pyrogenic exotoxin III. Streptolysin S and O (haemolysin): anti-streptolysin O titer – confirming rheumatic fever! IV. Exoenzymes: hyaluronidase (,,spreading factor”) DNase streptokinase (cleaves plasminogen to plasmin promoting fibronolysis 5) Clinical pictures by S. pyogenes I. Purulent infections: mediated by S. pyogenes bacterium II. Toxin mediated infections: Scarlate fever, TSST III. Complications: Post-streptococcal diseases: typ2 and typ 3 hypersensitive reactions 5) Clinical pictures I. Pyogenic infections (mediated by the bacterium) • • • • • • • • • • pharyngitis, tonsillitis follicularis, otitis media, sinusitis meningitis, pneumonia, endocarditis puerperal fever (Semmelweis) Impetigo, erysipel myositis necrotising fasciitis (“fleish-eating bacterium”) Streptococcus pyogenes 5) Clinical pictures Impetigo contagiosa Tonsillitis follicularis Childbed fever (puerperal fever) by S. pyogenes Ignaz Ignaz Semmelweis Semmelweis demonstrated that childbed fever (puerperal fever), caused by streptococcal infections, was transmitted to patients by doctor’s hands Pioneer of antisepsis in obstetrics Women giving birth in hospitals by medical students and physicians were 4x more likely to contract puerperal fever compared to those by midwives Handwashing with chlorin water (leach powder) Streptococcus pyogenes 5) Clinical pictures Nekrotising fasciitis Erysipel Streptococcus pyogenes 5) Clinical pictures II. Toxin mediated diseses • Scarlet fever: mediated by erythrogen toxin, which can destroy the endothel cell of capillaries – red rash • Can not be formed into toxoid! NO vaccination • 2 days after the infection exanthems on the skin and throat Scarlet fever Strawberry tongue: papilla hyperthrophy on the tounge Exanthems on the skin III. Poststreptococcal diseases (complications of a S. pyogenes infection) 1.Rheumatic fever: Typ 2 hypersensitive reaction: surface anigen of the heart muscle is similar to the Str. pyogenes antigen(M-protein) antibodies bound to the heart muscle • inflammatory changes in the heart (pancarditis) • endocarditis: damage of heart valves 2. Acute glomerulonephritis (GN): immuncomplex mediated Immunkomplexes in joints: polyarthritis Immunkomplexes in the glomerulus : nephritis • Typ 3 hypersensitive reaction: immuncomplexes bind to the glomerulus basalmembrane glomerulonephritis • Hypertonia and oedema 3. Erythema nodosum: • subcutan nodles, immuncomplex mediated III. Poststreptococcal diseases (complications) Immunity: Antibacterial: you can have tonsillitis follicularis more than once (several serotypes) Antitoxical: you acquire scarlet fever only once (erythrogenic toxin has the same structure in all the strains) Treatment: penicillin (natural susceptible to penicillin), • macrolid (if the patient has penicillin allergy) • complications should be prevented. Streptococcus agalactiae 1) Microscopic morphology: Gram positive cocci 1m in diameter arranged in chains 2) Cultivation: blood agar media: -haemolysis (narrow) 1 mm in diameter circular, tiny needletip colonies diagnostic antibiotic: bacitracin (R) CAMP + 3) Antigen structure: Lancfield group “B” 4) Pathogenicy: colonisation in the vagina 5) Clinical pictures: during pregnancy: abortion during delivery the neonates can be infected: newborn pneumonia, ARDS, meningitis, sepsis (Screening of pregnant women after the 35th week of gestation!) • Treatment and prevention: ampicillin Enterococcus genus 1) Microscopic morphology: Gram postive cocci (elongated) 1m in diameter arranged in short chains Antigen structure: Group D Lancfield type Enterococcus faecalis, Enterococcus faecium 2) Cultivation: on blood agar greyish colonies • (sometimes green court under the colony) • selective culture media – black colonies (E67 culture media) 3) Biochemical feature: esculin (polysaccharid) hydrolysis Enterococcus faecalis, Enterococcus faecium Clinical pictures: enteric cocci : present in the intestine (normal flora) facultative pathogen inflammation of bile tract and urinary tract nosocomial infection after surgery Intestinal trauma /perforation sepsis, peritonitis Treatment: natural resistance cephalosporin and sulfonamid! Th.: synergistic combination: ampicillin + gentamycin Th: vancomycin increased level of resistance to glycopeptid : VRE: vancomycin resistant Enterococci Streptococcus viridans group (S. mutans, S. mitis, S. sanguis, S. salivarius, S. milleri) heterogenous collection of - haemolytic Streptococci ,,viridae” – Latin term for green Member of the normal flora of the oral cavity. • Cultivation on blood and chocolate agar: - haemolysis • Separate from S. pneumoniae S: normal flora optochin R • clinical picture: In oral cavity: colonisation on the teeth dental plaque formation dental caries • If Streptococcus viridans enter the circulation cause subacute endocarditis Peptostreptococci Anaerobic Streptococci! • Normal flora of the oral cavity, gastrointestinal tract. • Polymicrobic, pyogenic infections, abscess formation in the abdominal cavity, lung and brain or in the oral cavity • Treatment: metronidazol, clindamycin Abscess Streptococcus pneumoniae 1) Microscopic morphology: Gram positive diplococci, ,,flame-shaped” or ,,lancet-shaped” Streptococcus pneumoniae Fig. 2.21 Pneumococcal pneumonia. Preparation of sputum showing predominance of pneumococci mostly as lanceolate diplococci. Gram stain. By courtesy of Dr. J.R. Cantey Streptococcus pneumoniae 2) Cultivation: • blood and chocolate agar haemolysis • autolysis: ageing colonies are umbilicated 3) Biochemical features optochin sensitivity (S) separate from the viridans group 4) Virulenc factor Polysaccharide capsule Streptococcus pneumoniae • Can not be grouped with the Lancefield technique! • based on capsule – 91 serotypes • ,,quellung”-reaction (German ,,swelling”): anticapsular antibody plus pneumococci Quellung reaction of greater refractiveness around the bacteria by microscope S. pneumoniae Streptococcus pneumoniae Source of infection: 5-10% of population carry S. pneumoniae in nose, throat Clinical picture: lobar pneumonia sinusitis, otitis media bacteriaemia, meningitis ulcus serpens corneae (eye infection) Streptococcus pneumoniae Treatment: high penicillin resistance decreased affinity of the antibiotic to PBP Therapy: macrolid, fluoroquinolones Prevention: 13-valent polysaccharide vaccine (conjugated) obligatory vaccine for new borns ( in Hungary since 2014 July) recommended: 1. children (born before 2014 July) 2. adults above 65 years of age 3. adults with chronic disease (COPD, heart failure) 4. patient after splenectomy Vaccinations against bacterial infections 1) BCG = against Mycobacterium tuberculosis (living attenuated bacterium) 2) aP = against Bordetella pertussis (acellulare Pertusis vaccination) 3) Diphtheria = against Corynebacterium diphtheriae (toxoid) 4) Tetanus = against Clostridium tetani (toxoid) 5) Hib = against Haemophilus influenzae b capsule antigen 6) Neisseria meningitidis capsule antigen 7) Streptococcus pneumoniae capsule anigen 8) Salmonella typhi killed bacteria (polysaccharide derivative) 9) Vibrio cholerae killed bacteria