* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download THE DISTURBANCES OF ABSORPTION
Survey
Document related concepts
Pharmaceutical marketing wikipedia , lookup
Specialty drugs in the United States wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Compounding wikipedia , lookup
Orphan drug wikipedia , lookup
Plateau principle wikipedia , lookup
Drug design wikipedia , lookup
Psychopharmacology wikipedia , lookup
Drug discovery wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Transcript
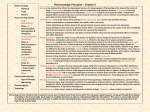
PATHOPHARMACOKINETICS Pharmacokinetic the action of the body on the drug, including: Liberation Absorption Distribution Metabolism Excretion Metabolism + Excretion = Elimination ABSORPTION process of drug movement from the administration site to the systemic circulation. Bioavailability of a drug According to the European Medicines Evaluation Agency (EMEA): bioavailability means the rate and extent (amount) to which the active substance or active moiety is absorbed from a pharmaceutical form, and becomes available at the site of action (in the general circulation). Bioavailability is defined as the fraction of an administered dose that reaches the systemic circulation. By definition, when a medication is administered intravenously, its bioavailability is 100%. When a medication is administered via other routes (such as orally), its bioavailability decreases (due to incomplete absorption and first-pass metabolism ). . disturbances of absorption Diseases can change: a) pH chyme -diseases with lack or deficiency of HCL b) motor activity of gut ( speed of stomach emptying and intestinal passage ) - patients with slow stomach emptying and patients with pylorostenosis - patients with slow stomach emptying and patients with slow intestinal passage → ↑ first pass effect - ↑ intestinal passage ( enteritis, gastritis and diarrhoea ) → ↓ absorpition c) surface of absorption ( quantitative and qualitative changes ) - patients after partial gastrectomy, ileostomy and colon resection - ↓ permeability of cell membrane- diabetes, adrenocotrtical failure - ↑permeability of cell membrane – jaundice, allergic diseases d) vascularity of absorption place cardiogenic shock, myocardial infarction, heart failure →↓ visceral blood flow → ↓ absorption of drugs administered orally and parenterally e) contents of substances conditioned drug absorption - enteropathy and hepatopathy – disturbanes of bile secretion and bile transport ↓ absorption of lipid-soluble drugs DISTRIBUTION Transfer of drug between regions of the body Disribution between blood/plasma, tissues, organ and body fluids pharmacokinetic parameter - volume of distribution - Vd The ratio of the amount of the drug in body to its concentration in the plasma or blood Amount of drug in the body Vd = --------------------------------------Plasma drug concentration ( Units = volume ) Vd ≈ 5 l – drug in blood Vd > 40 l – drug in all body fluids disturbances of distribution - cardiogenic shock - ↓blood supply of muscles and fatty tissue → ↓drugs distribution to these tissues - changes of compartment volume - ↑extracellular fluid ( edema ) – changes of Vd - disturbances of acid-base equilibrium - interferences of tissue drug uptake - deficiency of transport activator through cell membrane - quantitative and qualitative changes of plasma protein composition in hepatic and renal diseases → changes of binding of drugs by plasma proteins METABOLISM ( BIOTRANSFORMATION ) Biochemical modification or degradation of drug, usually through specialized enzymatic systems. Drug metabolism often converts lipophilic chemical compounds into more readily excreted polar products. Drug metabolism can result in toxication or detoxication - the activation or deactivation of the chemical. disturbances of biotransformation ( metabolism ) Metabolism of drugs can be disturbed by: - hepatic cirrhosis - chronic active hepatitis - hepatocellular damage ( toxic factors and starvation ) - acute virus hepatitis - mechanical jaundice These pathological states can altered the drugs metabolism by: - change of hepatic blood flow - quantitative and qualitative changes of plasma proteins - presence of joints between portal and systemic circulation - impairment of hepatocyte ability to drugs uptake from blood, drugs biotransformation by enzymatic system and their excretion to bile first-pass effect the elimination of drug that occurs after administration buy before it reaches the systematic circulation, eg, during passage through the gut wall, portal blood, and liver for orally administered drug - cardiovascular drugs: acebutolol, alprenolol, diltiazem, labetolol, lidocaine, metoprolol, nifedipine, nitroglycerine, propranolol, prazosine, tymolol, verapamil - drugs acting on CNS: amitryptyline, chlorpromazine, doxepine, imipramine, morphine, nortryptyline, pethidine - NSAID acetaminophen, acetylosalicylic acid, Drugs required reduction of dose or elongation of dosage interval in hepatic diseases - cardiovascular drugs: acebutolol, alprenolol, clofibrate, digitoxin, furosemide, heparine, labetolol, lidocaine, metildigoxin metoprolol, propranolol, tymolol, verapamil - NSAIDs: aminophenazone, acetylsalicylic acid, acetaminophen, naproxen, phenazone, phenacetin, phenylbutazone, - OPIOID ANALGESIC: fentanyl, pethidine, pentazocine DRUGS ACTING ON C.N.S.: alprazolam, chlordiazepoxide, diazepam, lorazepam, nitrazepam, pentobarbital, phenobarbital, valproic acid EXCRETION Process by which the drug/nutrient or metabolites are removed from the body primarily by the kidneys. Other routes of excretion from the body can include in bile, saliva, sweat, tears, faeces, milk and exhaled air. The disturbances of excretion The drugs excreted in bile: ampicillin, rifampicin, tetracycline, daunorubicin, doxorucicin, vinblastine, vincristine, can be cumulated in the body in: -hepatic cholestasia - mechanical jaundice In renal failure – changes of: 1) glomerular filtration 2) tubular secretion 3) tubule reabsorption Drugs exacting reduction of dose or elongation of interval dosage in renal failure ANTIBACTERIALS DRUGS: - Aminoglycosides - Penicilillines: azlocilin, amoxicilin, carbenicilin, methicillin - Cephalosporines: cefazolin, cefaclor, cephalotin, cefamandole, cefotaxime, cephradine, ceftriaxone, cefuroxime - Amphotericin B - Lincomycin, - Tetracyclines - Vancomycin NSAIDs CARDIOVASCULAR DRUGS: ACE-inhibitors: captopril, enalapril Ca-blockers: nicardipine, nifedipine diuretics: acetazolamide, etacrynic acid, spironolactone, triamterene, thiazides - digoxin - methyldopa DRUGS ACTING ON C.N.S.: chlordiazepoxide, phenobarbital DRUGS USED FOR GOUT: allopurinol, probenecid ANTITHYROID DRUGS: metylthiouracyl, propyltiouracyl ELIMINATION - pharmacokinetic parameters CLEARANCE – CL The ratio of the rate of elimination of a drug to its concentration in plasma or blood Rate of elimination of drug CL = -------------------------------------Plasma drug concentration ( Units = volume per unit time ) CLEARENCE – is a measure of the capacity of the body to remove a drug Types of clearances: - renal - hepatic - pulmonary - dermal ( cutaneous ) BIOLOGICAL HALF-LIFE TIME – t1/2, t0,5 The time it takes for the blood concentration of the drug to fall to 50 % 0.693 x Vd t1/2= -----------------CL 0.603 t1/2= ----------------kel ( Units = time ) After 4 half lives, elimination is 94% complete.