* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Biosafety Level 2 - University of Guelph Physics
Survey
Document related concepts
Eradication of infectious diseases wikipedia , lookup
Hepatitis C wikipedia , lookup
History of biological warfare wikipedia , lookup
Cross-species transmission wikipedia , lookup
2015–16 Zika virus epidemic wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Ebola virus disease wikipedia , lookup
Influenza A virus wikipedia , lookup
Hepatitis B wikipedia , lookup
Antiviral drug wikipedia , lookup
Biological warfare wikipedia , lookup
Orthohantavirus wikipedia , lookup
United States biological defense program wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Marburg virus disease wikipedia , lookup
West Nile fever wikipedia , lookup
Transcript
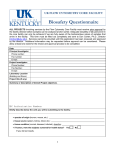
Department of Physics Biosafety Level 2 Standard Operating Procedure Contents 1.0 Purpose 2.0 Hazards 3.0 Responsibilities 4.0 Basic Biosafety Procedures (SOP) 5.0 Biohazards Handling Equipment 6.0 References 7.0 Appendix : Definitions, Risk Groups, Containment Laboratory, Containment Levels, Organisms Lists, Agents Classification, Biosafety Level 2 Criteria, UoG Biosafety Policy & Biosafety Procedures, Biological Safety Cabinets, Dept. of Microbiology Safety Rules and Procedures, Decontamination and Disposal, Biosafety Training Checklist Department of Physics Standard Operating Procedure # SOP-BL2 Task/Process: Prepared by: Approved by: Biosafety Level 2 David Atkinson JHSC: Reggi Vallillee, Steve Wilson Issue Date: Feb 6, 2007 Revision: draft only Page: 2 1.0 Purpose The purpose of this procedure is to ensure that persons working with biohazardous agents or substances (bacterial, fungal, parasitic, viral, etc.) follow safe working practices in a Biosafety Level 2 laboratory. 2.0 Hazards • Contact with infectious substances may cause laboratory acquired infections (LAIs) • Infectious substance may enter the body through ingestion, inhalation, contact with mucous membranes, eyes, or non-intact skin (wounds, scrapes, bites, etc.) • Risk of exposure may occur through infectious aerosols, spills, splashes, needlestick injury, broken glass, pipet tips, centrifuge accidents, scalpel blades, sharp objects, etc. • Secondary transmission of disease to the public may occur by workers carrying infectious agents outside the laboratory • Children, pregnant women, the elderly, immunocompromised or immunosuppressed individuals are especially vulnerable to transmission of infectious substances • Accidental release or transmission of pathogens into the environment may cause disease, sickness, deleterious effect, or even mortality to human and nonhuman recipients • Unlike chemical and physical agents, there is NO “safe” level of non-contained pathogenic organisms • Biosecurity of biohazardous materials is a growing concern for scientific institutions 2 Department of Physics Standard Operating Procedure # SOP-BL2 Task/Process: Prepared by: Approved by: Biosafety Level 2 David Atkinson JHSC: Reggi Vallillee, Steve Wilson Issue Date: Feb 6, 2007 Revision: draft only Page: 3 3.0 Responsibilities (prior to commencing work in a Level 2 laboratory) • All workers must be WHMIS trained and attend the Department Safety course • First time users must review University of Guelph Safety Policy 851.11.01 Biosafety Policy - Section 9: Worker Responsibilities (see appendix) • First time users must be trained by qualified personnel in biosafety procedures and sign a Biosafety Training Checklist form • A worker must report any illness, injury or medical condition that may be aggravated or compromised by exposure to biohazardous materials • A worker must understand that containment and safe handling of known and potentially biohazardous materials requires strict adherence to prudent microbiological practices • Eye and skin protection must be worn at all times during handling of any biohazardous or potentially biohazardous substance • A worker must be trained in the dissemination and containment of contaminants • Users must be receive adequate instruction and training in appropriate aseptic technique (see appendix for Decontamination and Disposal from Biohazards Reference Manual) • Only approved containers may be used for disposal of biohazardous wastes • Users must be trained and knowledgeable in spills cleanup and emergency procedures • When in doubt always seek guidance from supervisory personnel • All users must review Biosafety Level 2 Criteria (section 7.7 in appendix) including: Standard Microbiological Practices, Special Practices, Safety Equipment and Laboratory Facilities (Primary/Seconday barriers) Biological Safety Cabinets 3 Department of Physics Standard Operating Procedure # SOP-BL2 Task/Process: Prepared by: Approved by: Biosafety Level 2 David Atkinson JHSC: Reggi Vallillee, Steve Wilson Issue Date: Feb 6, 2007 Revision: draft only Page: 4 4.0 Basic Biosafety Procedures (for any laboratory dealing with infectious agents) • KEEP THE LABORATORY NEAT, ORDERLY AND CLEAN • KEEP LABORATORY DOORS CLOSED - ACCESS TO A LEVEL 2 LABORATORY IS LIMITED • DO NOT EAT, DRINK OR STORE FOOD STUFF IN THE LABORATORY • WASH HANDS WITH SOAP BEFORE LEAVING THE LABORATORY AND AFTER HANDLING ANY CONTAMINATED MATERIALS • PROTECT OPEN WOUNDS, CUTS, SCRATCHES WITH WATERPROOF DRESSINGS • USE APPROPRIATE PERSONAL PROTECTIVE GEAR WHEN HANDLING CONTAMINATED, INFECTIOUS OR POTENTIALLY INFECTIOUS MATERIALS • WEAR A LAB COAT, DISPOSABLE GLOVES AND EYE PROTECTION IN THE LABORATORY • DISINFECT WORK SURFACES BEFORE AND AFTER EACH WORK PERIOD • AVOID PROCEDURES THAT CREATE AEROSOLS AND USE CONTAINMENT DEVICES • DECONTAMINATE ALL CONTAMINATED OR INFECTIOUS MATERIALS PRIOR TO DISPOSAL • PLACE BIO-WASTE IN ORANGE BIOHAZARD BAGS INSIDE A LEAK PROOF CONTAINER WITH COVER FOR TRANSPORT TO AUTOCLAVE • DISPOSE OF ALL SHARPS, SYRINGES, BROKEN GLASS IN PROPER CONTAINERS • CLEAN-UP SPILLS IMMEDIATELY AND DISINFECT THE AREA • REPORT ALL INCIDENTS, INJURIES OR SPILLS TO YOUR SUPERVISOR 4 5.0 Biohazards Handling Equipment WHMIS Class D – Division 3 Biohazardous Infectious signage Post Biosafety Level 2 signage on laboratory door Syringes, sharps, scalpels dispose in SHARPS container Sharps collector container for biohazardous materials Yellow waste bag used for decontaminated glass only Transport all biohazardous waste inside a leak proof container with cover 5 5.0 Biohazards Handling Equipment (cont) Sharps and biohazard waste station Standard autoclaving biohazard bag Autoclave in New Science Complex Biological safety cabinet Containment devices Personal protection for eye, skin, lung 6 6.0 References Risk Group Classification for Infectious Agents American Biological Safety Association http://www.absa.org/XriskgroupsX/index.html Biohazards Reference Manual American Industrial Hygiene Association 1985 (Reprinted 1986), Prepared by AIHA Biohazards Committee Laboratory Biosafety Level Criteria CDC Department of Health and Human Services Centers for Disease Control and Prevention Office of Health and Safety http://www.cdc.gov/od/ohs/biosfty/bmbl4/bmbl4s3.htm Human Pathogens and Organisms List Public Health Agency of Canada http://www.phac-aspc.gc.ca/ols-bsl/pathogen/organism_e.html The Laboratory Biosafety Guidelines, 3rd Edition 2004 Minister of Health, Public Health Agency of Canada Office of Laboratory Security Microbiology Teaching Laboratories Safety Rules and Procedures University of Guelph, Dept. of Molecular and Cellular Biology Biosafety Policy 851.11.01 Biosafety Procedures 851.11.02 University of Guelph Safety Policy Manual http://www.uoguelph.ca/ehs/policies/Subject_Index.htm#BIOSAFETY University of Guelph, EHS Department Biosafety Videotape Catalogue http://www.uoguelph.ca/ehs/videos.pdf Protecting Yourself from Hantavirus Related Illness 17 min Effective Use of the Laminar Flow Biological Safety Cabinet 16 min Preventing Employee Exposure to Infectious Disease 19 min Using the Gravity Displacement Steam Autoclave 29 min Safe Use of Biological Safety Cabinets or The case of Contaminated Cultures 22 min Biological Containment - Microbiological Safety Cabinets 25 min Introduction to Biological Safety Cabinets - Part I 15 min Introduction to Biological Safety Cabinets - Part 2 21 min Controlling Your Risks: HIV in Research Laboratory 28 min Mammalian Cell Culture Hazards 8:22 min Bloodborne Pathogens 11 min Biosafety 20 min Germinology: An Introduction to Infection Control 20 min 7 7.0 Appendix 7.1 Definitions Biohazard A biohazardous agent is one that is biological in nature, capable of self-replication and has the capacity to produce deleterious effects upon other biological organisms, particularly humans. A biological agent or substance present in or arising from the work environment which present or may present a hazard to the health or well being of the worker or community. Biological agents or substances which could be biohazards include: infectious or parasitic agents; non infection microorganisms such as some fungi, yeasts and algae; plants and plant products, animal and animal products which cause occupational disease. Categories of Biohazardous Agents A. B. C. D. E. F. G. H. I. J. K. L. M. Bacteria Fungi Viruses Rickettsiae Chlamydiae Parasites Recombinant products Allergens Cultured animal cells and the potentially infectious agents these cells may contain Infected clinical specimens (tissues, fluids, etc.) Tissues from experimental animals (including animal dander) Plant viruses, bacteria and fungi Toxins (bacterial, plant, etc.) 7.2 Risk Group and Biosafety Level Definitions Canadian Laboratory Safety Guidelines (2004; list not available) Inherent risks of a pathogen made on basis of factors such as severity of disease caused, routes of infection, virulence and infectivity takes into account existence of effective therapies, possibilities for immunization, presence of vectors, quantity of agent and whether agent is indigenous to Canada, possible effects on other species, including plants, or possible economic environmental effects. Risk Group 1 (low individual and community risk). Any biological agent that is unlikely to cause disease in healthy workers or animals. Risk Group 2 (moderate individual risk, limited community risk). Any pathogen that can cause human disease, but under normal circumstances is unlikely to be a serious hazard to laboratory 8 7.2 Risk Group and Biosafety Level Definitions (cont) workers, the community, livestock or the environment. Laboratory exposures rarely cause infection leading to serious disease, effective treatment and preventive measures are available and the risk of spread is limited. Risk Group 3 (high individual risk, low community risk). Any pathogen that usually causes serious human disease, or can result in serious economic consequences but does not ordinarily spread by casual contact from one individual to another, or that causes disease treatable by antimicrobial or antiparasitic agents. Risk Group 4 (high individual and community risk). Any pathogen that usually produces very serious human disease, often untreatable, and may be readily transmitted from one individual to another, or from animal to human or vice-versa, directly or indirectly, or by casual contact. CDC/NIH Guidelines (1999) "Biosafety in Microbiological and Biomedical Laboratories" 4th Edition, 1999. Section III gives criteria for placing work into a biosafety containment level; not yet translated into Risk groups. Biosafety Level 1 (BSL 1): well characterized agents not consistently known to cause disease in healthy adult humans of minimal potential hazard to laboratory personnel and the environment Biosafety Level 2 (BSL 2): agents of moderate potential hazard to personnel and the environment Biosafety Level 3 (BSL 3): indigenous or exotic agents which may cause serious or potentially lethal disease as a result of exposure by the inhalation route (applicable to clinical, diagnostic, teaching, research or production facilities) Biosafety Level 4 (BSL 4): dangerous and exotic agents which pose a high individual risk of aerosol-transmitted laboratory infections and life-threatening disease 7.3 The Containment Laboratory This laboratory provides general space appropriate for work with infectious agents or potentially infectious materials when the hazard levels are low and laboratory personnel can be adequately protected by standard laboratory practice. Work is commonly conducted on the open bench with certain operations confined to biological safety cabinets. Conventional laboratory designs are adequate. Areas known to be sources of general contamination such as waste staging areas should not be adjacent to media processing areas, tissue culture laboratories. Public areas and general offices to which nonlaboratory staff require frequent access should be separated from space which primarily supports laboratory functions. 9 7.4 Containment Levels The Public Health Agency of Canada is moving away from classifying organisms according to risk group towards a classification system based on containment level. Containment levels are more appropriate and give the end-user an indication of the containment required for handling the organism safely in a laboratory setting. The containment level required for work with a particular agent is based on the manipulations generally associated with laboratory-scale research and clinical procedures. Containment Level 1 (CL1) This level applies to the basic laboratory handling agents requiring containment level 1. CL1 requires no special design features beyond those suitable for a well-designed and functional laboratory. Biological safety cabinets are not required. Work may be done on an open bench top, and containment is achieved through the use of practices normally employed in a basic microbiology laboratory Containment Level 2 (CL2) This level applies to the laboratory handling agents requiring containment level 2. The primary exposure hazards associated with organisms requiring CL2 are through the ingestion, inoculation, and mucous membrane route. Agents requiring CL2 facilities are not generally transmitted by the airborne route, but care must be taken to avoid the generation of aerosols (aerosols can settle on bench tops and become an ingestion hazard by contamination of the hands) or splashes. Primary containment devices such as biological safety cabinets and centrifuges with sealed rotors or safety cups are to be used, as well as personal protective equipment (gloves, laboratory coats, protective eyewear). Environmental contamination must also be minimized by the use of hand washing sinks and decontamination facilities (autoclaves). Containment Level 3 (CL3) This level applies to diagnostic, research and clinical laboratories, production facilities, or teaching laboratories handling agents requiring containment level 3. These agents may be transmitted by the airborne route, often have a low infectious dose to produce effects, and can cause serious or life-threatening disease. CL3 emphasizes additional primary and secondary barriers to minimize the release of infectious organisms into the immediate laboratory and the environment. Additional features to prevent transmission of CL3 organisms are appropriate respiratory protection, HEPA filtration of exhausted laboratory air, and strictly controlled laboratory access. Containment Level 4 (CL4) This is the maximum containment available and is suitable for facilities manipulating agents requiring containment level 4. These agents have the potential for aerosol transmission, often have a low infectious dose, and produce very serious and often fatal disease; there is generally no 10 7.4 Containment Levels (cont) treatment or vaccine available. This level of containment represents an isolated unit, functionally and, when necessary, structurally independent of other areas. CL4 emphasizes maximum containment of the infectious agent through complete sealing of the facility and testing to pressure decay; isolating the researcher from the pathogen by containing the individual in a positive pressure suit (most common) or containing the pathogen in a Class III biological safety cabinet line (rare); and decontaminating air and other effluents produced in the facility. http://www.phac-aspc.gc.ca/ols-bsl/pathogen/organism_e.html 7.5 Organism Lists The Human Pathogens Importation Regulations (SOR/94-558) are the regulatory authority for facilities wishing to import human pathogens into and transfer of specimens within Canada. Any facility wishing to import human pathogens requiring containment levels 2, 3, or 4 must have a valid Public Health Agency of Canada permit prior to importation. Pathogens requiring containment level 1 facilities are not regulated by the HPIR, and therefore a permit is not required for their importation. The accompanying list of human pathogens (Bacteria, Viruses and Fungi) is a dynamic list detailing required containment levels for manipulation. This list is regularly updated, and the required containment levels are continually reassessed as new information becomes available. It must also be understood that the accompanying list of human pathogens is not complete. The containment level for unlisted organisms must be verified in consultation with the Office of Laboratory Security, Public Health Agency of Canada. Among the listed human pathogens, those classified as potentially harmful to animals have also been indicated. Animal pathogens are regulated by the Canadian Food Inspection Agency (CFIA). For importation of pathogens common to both humans and animals, an import permit is required from the CFIA as well as the Public Health Agency of Canada. Non-Pathogenic Organisms 35 KB Adobe Downloadable Document The "Human Pathogens: Bacteria" list is currently being clarified. The "Human Pathogens: Viruses" list is currently being clarified. The "Human Pathogens: Fungi" lists is currently being clarified. If you require assistance with classification of any of these agents into the appropriate containment level please contact the Office of Laboratory Security (613) 957-1779 [email protected] 11 7.6 Classification of Agents (American Biological Safety Association) Class 1 Agents of no or minimal hazard under ordinary conditions of handling (biosafety level 1 standards of practice). Class 2 Agents of moderate potential hazard to personnel and the environment This class includes agents which may produce disease of varying degrees of severity from accidental inoculation or injection or other means of cutaneous penetration but which are contained by ordinary laboratory techniques (biosafety level 2 standards of practice and facility). Class 3 Agents which may cause serious or potentially lethal disease as a result from exposure by the inhalation route. Class 3 agents include those derived from outside the United States which require a federal permit for importation unless they are specified for higher classification. This class also includes pathogens which require special conditions for containment (biosafety level 3 standards of practice and facility). Class 4 Agents that require the most stringent conditions for their containment because they are extremely hazardous to laboratory personnel or may cause serious epidemic disease. Class 5 Foreign animal pathogens that are excluded from the United States by law or whose entry is restricted by USDA administrative policy. CLASS 1 AGENTS (Class 1 includes all agents which have been assessed for risk and do not belong in higher classes. Call the SHEA at 277-2753 to verify any unknown agent status). • • • • • • • • • Bacillus cereus Canine distemper virus (Snyder-Hill strain) Influenza virus reference strains A/PR8/34, A/WS/33 or commonly used neurotropic variants Newcastle virus strains licensed for vaccine use in US. Lactobacillus acidophilus Lactobacillus bulgaricus Lactobacillus casei Newcastle virus - strains licensed for vaccine use in US. Parainfluenza virus 3, SF4 strain Agents listed in Appendix C of "NIH Guidelines for Research Involving Recombinant DNA Molecules" 12 7.6 Classification of Agents (cont) CLASS 2 AGENTS 2B Bacterial Agents • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • Acinetobacter baumannii (formerly A. calcoaceticus) Actinobacillus (all species) Actinomyces pyogenes (formerly Corynebacterium pyogenes) Aeromonas hydrophila Amycolata autotrophica Arachnia propionica Archanobacterium haemolyticum (formerly Corynebacterium haemolyticum) Arizona hinshawii (all serotypes) Bacillus anthracis Bacillus subtillis Bacteroides (all species) Bartonella henselae Bartonella quintana Bartonella vinsonii Bordetella (all species) Borrelia recurrentis Borrelia vincenti Borrelia burgdorferi Campylobacter coli Campylobacter fetus ssp. Fetus Campylobacter jejuni Chlamydia pneomoniae Chlamydia psittaci Chlamydia trachomatis Clostridium botulinum Clostridium chauvoei Clostridium dificile Clostridium haemolyticum Clostridium histolyticum Clostridium novyi Clostridium perfringens Clostridium septicum Clostridium sordellii Clostridium tetani Corynebacterium bovis Corynebacterium diptheriae Corynebacterium equi Corynebacterium ovis / pseudotuberculosis Corynebacterium renale Dermatophilus congolensis Edwardsiella tarda Enterbacter aerogenes Erysipelothrix insidiosa Erysipelothrix rhusiopathiae 13 7.6 Classification of Agents (cont) • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • Escherichia coli (all enteropathogenic, enterotoxigenic, enteroinvasive and strains bearing K-1 antigen, including E. coli O157:H7) Francisella novicida Fusobacterium necrophorum Haemophilus ducreyi Haemophilus gallinarum Haemophilus haemolyticus Haemophilus influenzae Haemophilus parahaemolyticus Haemophilus parainfluenzae Helicobacter pylori Klebsiella (all species except oxytoca which is in class 1) Legionella (including L. pneumophila) Leptospira interrogans (all serotypes) Listeria (all species) Mixa polymorpha Moraxella (all species) Mycobacteria (all species except those listed in Class 3) Mycobacterium africanum Mycobacterium asiaticum Mycobacterium avium Mycobacterium bovis BCG vaccine strain Mycobacterium chelonei Mycobacterium fortuitum Mycobacterium kansasii Mycobacterium leprae Mycobacterium malmoense Mycobacterium marinum Mycobacterium paratuberculosis Mycobacterium scrofulaceum Mycobacterium simiae Mycobacterium szulgai Mycobacterium ulcerans Mycobacterium xenopi Mycoplasma (all species except Mycoplasma mycoides and Mycoplasma agalctiae which are in Class 5) Neisseria gonorrhoea Neisseria meningitidis Nocardia asteroides Nocardia brasiliensis Nocardia otitidiscaviarum Nocardia transvalensis Pasteurella (all species except those listed in class 3) Plesiomonas shigelloides Rhodococcus equi Rochalimaea vinsonii Salmonella (all species and all serotypes) Serratia marcescens Shigella (all species and all serotypes) 14 7.6 Classification of Agents (cont) • • • • • • • • • • • • • • • Sphaerophorus necrophorus Staphylococcus aureus Staphylococcus epidermidis Streptobacillus moniliformis Streptococcus agalactiae Streptococcus pneumoniae Streptococcus pyogenes Treponema carateum Treponema pallidum Treponema pertenue Vibrio cholerae (including biotype El Tor) Vibrio parahemolyticus Vibrio vulnificus Yersinia enterocolitica Yersinia pseudotuberculosis 2F Fungal Agents • • • • • • • • • • • • • • • • • • • • • • Absidia (all species) Actinomyces (including Nocardia species and Actinomyces species and Arachnia propionica) Aspergillus (all species) Blastomyces dematitidis Candida (all species) Cladosporium bantianum Cladosporium (xylohypha) trichoides Crytococcus neoformans Dactylaria galopava (Ochroconis gallopavum) Epidermophyton (all species) Exophiala (Wangiella) dermatitidis Fonsecaea pedrosoi Geotrichum (al species) Loboa loboi Madurella mycetomi Microsporum (all species) Mucor (all species) Penicillium marneffei Rhizopus (all species) Sporothrix schenckii Trichophyton (all species) Trichosporon (all species) 2P Parasitic Agents • • • • • Acanthocheilonema (all species) Acanthamoeba (all species) Ancylostoma (all species) Angiostrongylus (all species) Ascaris (all species) 15 7.6 Classification of Agents (cont) • • • • • • • • • • • • • • • • Babesia (all species) Balantidium (all species) Brugia (all species) Caprillaria (all species) Clonorchis (all species) Coccidia (all species) Crytosporidium (all species) Dicrocoelium (all species) Dipetalonema (all species) Diphyllobothrium (all species) Dipylidium (all species) Dracunculus (all species) Echinococcus granulosus Echinococcus multiocularis Echinococcus vogeli Entamoeba histolytica • 2P Parasitic Agents (cont’d) • • • • • • • • • • • • • • • • • • • • • • • • • • Enterobius (all species) Fasciola (all species) Giardia (all species) Heterophyes (all species) Hymenolepis (all species) Isospora (all species) Leishmania (all species) Linguatula (all species) Loa (all species) Macracanthrohynchus (all species) Microsporidia Naegleria fowleri Naegleria gruberi Necator (all species) Onchocerca (all species) Opisthorchis (all species) Paragonimus (all species) Plasmodium (all species) Pneumocystis carinii Sarcocystis Schistosoma (all species) Strongyloides (all species) Taenia solium Toxascaris (all species) Toxocara (including T. canis) Toxoplasma (all species) 16 7.6 Classification of Agents (cont) • • • • • • Trichinella spiralis Trichomonas vaginalis Trichostrongylus (all species) Trichuris trichiura Trypanosoma (all species) Wuchereria (all species) 2V Viral Agents (* denotes oncogenic viruses) • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • Adv-Sv40, Ad2-SV40* Adenoviruses (human - all types)* Avian leukosis* Avain Sarcoma virus B-K virus Bebaru virus Bluetongue-indigenous Bovine leukemia* Bovine papilloma* Buffalopox virus Bunyamwera virus Cache Valley virus Calciviruses California Encephalititis virus Camelpox virus CELO* Chikkungunya vaccine strain 131/25 Coronaviruses Cowpox virus Coxpox virus Coxsackie A and B viruses Cytomegalovirus Dengue virus serotypes 1,2,3,&4 Dog Sarcoma * Eastern Equine Encephalomyelitis virus Echoviruses (all types) Encephalomyocarditis virus (EMC) Epstein-Barr virus (EBV)* FeLV/FeSV* Fifth disease agent Flanders viruses Bibbon leukemia virus* Guinea pig herpes* Hamster leukemia* Hart Park virus Hepatitis viruses A,B,C,D,&E (associated antigen material) Herpes Simplex virus* other Herpes viruses (except Herpes virus simiae - Monkey B virus which is Class 4) Human papilloma viruses 17 7.6 Classification of Agents (cont) • • • • • • • • • • • • • • • • • • • • • Human parvovirus (B19) Influenza viruses (all types except A/PR8/34 which is in Class 1) Junin, vaccine strain candidate #1 Kunjin Langat virus Lucke (frog)* Lymphocytic choriomeningitis virus (LCM) (viscerotrophic strains) Lymphogranuloma venereum agent Marek’s Disease virus* Mason-Pfizer monkey virus* Measles virus Milker’s Node virus Molluscum contagiosum virus Mopeia virus Mouse mammary tumor* Mumps virus Murine leukemia* Murine sarcoma* Myxo-Paramyoviruses (all types except Canine distemper virus which is in class 1) Newcastle disease virus Norwalk virus 2V Viral Agents (cont) • • • • • O’nyong-nyong virus Orf virus Papovaviruses Parainfluenza viruses (all types except Parainfluenza virus 3, SF4 strain which is in Class 1) Paravaccina virus CLASS 3 AGENTS 3B Bacterial Agents • • • • • • • • • • • • • • • • Bartonella (all species) Brucella (all species) Burkholderia mallei (formerlyPseudomonas mallei) (determined on a case by case basis) Burkholderia pseudmallei (formerly Pseudomonas pseudomallei) (determined on a case by case basis) Coxiella burnetii Francisella tularensis Mycobacterium bovis (except BCG strain which is in class 2) Mycobacterium tuberculosis Pasteurella multocida type B ("buffalo" and other foreign virulent strains) Rickettsia akari Rickettsia australias Rickettsia canada Rickettsia conorii Rickettsia montana Rickettsia prowazekii Rickettsia rickettsii 18 7.6 Classification of Agents (cont) • • • • • • Rickettsia sennetsu Rickettsia siberica Rickettsia tsutsugamushi Rickettsia typhi (R. mooseri) Rochalima quintana (determined on a case by case basis) Yersinia pestis 3F Fungal Agents • • • • Coccidiodes immitis Histoplasma capsulatum Histoplasma capsulatum var. duboisii Histoplasma farciminosum 3V Viral Agents • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • Arboviruses (all strains except those in Class 2 and 4. Arboviruses indigenous to the United states are in Class 3, except those listed in Class 2. West Nile and Semliki Forest viruses may be classified up or down, depending on the conditions of use and geographic location of the laboratory.) Creutzfeldt-Jakob disease agent (BSE agent, a prion) Dengue virus, when used for transmission or animal inoculation experiments Hantaviruses HIV types 1&2, HTLV types 1&2, and SIV (all determined on a case by case basis) Japanese encephalitis virus Kuru disease agent Lymphocytic choriomeningitis virus (LCM) (Neurotrophic strains) Monkeypox virus, when used in vitro Rabies street virus Rift Valley fever virus St. Louis encephalitis virus Venezuelan equine encephalomyelitis virus (except strain TC-83 which is in class 2) Vesicular stomatitis virus (VSV) (classification depends on strain and experimental design) Vole rickettsia Yellow fever virus (wild, when used in vitro) Paracoccidioides brasilensis (determined on a case by case basis) Bovine infectious petechial fever Brucella melitensis Camel pox virus Cochliomyia hominvoraz (screw worm) Ephemeral fever virus Fowl plague virus Goat pox virus Histoplasma (Zymonema) farciminosum Hog cholera virus Louping ill virus Lumpy skin disease virus Mycoplasma agalactiae (contagious agalactia of sheep) Mycoplasma mycoides (contagious bovine pleuropneumonia) Nairobi sheep disease virus Newcastle disease virus (Asiatic strains) 19 7.6 Classification of Agents (cont) • • • • • • • • • • • • • • • • • Peste des petits ruminants (pest of small ruminants) Pseudomonas ruinatium (heart water) Rift valley fever virus Rinderpest virus Sheep pox virus Swine vesicular disease virus Teschen disease virus Theileria parva (East Coast Fever) Theileria Annulata Theileria bovis Theileria hirci Theileria lawrencei Trypanosoma vivax (Nagana) Trypansoma evansi Vesicular exanthema virus Wesselsbron disease virus Zyonema 3P Parasitic Agents None CLASS 4 AGENTS 4B Bacterial Agents None 4F Fungal Agents None 4P Parasitic Agents None 4V Viral Agents • • • • • • • Ebola fever virus Guanarito Hemorrhagic fever agents, including Crimean hemorrhgic fever,Congo, Junin, and Machupo viruses, and others as yet undefined Herpesvirus simiae (Monkey B virus) Lassa virus Marburg virus Monkeypox virus, when used for transmission or animal inoculation experiments 20 7.6 Classification of Agents (cont) • • • • Tick-borne encephalitis virus complex, including Absettarov, Central European encephalitis viruses, Hanzalova, Hypr, Kumlinge, Kyasanur forest disease, Omsk hemorrhagic fever, and Russian springsummer encephalitis Venezuelan equine encephalitis virus, epidemic strains, when used for transmission or animal inoculation experiments Yellow fever virus (wild, when used for transmission or animal inoculation experiments) Yellow fever virus (wild, when used for transmission or animal inoculation experiments) CLASS 5 AGENTS A. Animal Disease Organisms and Vectors which are Forbidden Entry into the United States by Law • Foot and Mouth disease virus B. Animal Disease Organisms and Vectors which are Forbidden Entry into the United States by USDA Policy • • • • • • • • • • • • • • • • • • • • • • • • • • • • African horse sickness virus African Swine fever virus Akabane virus Besnoitia besnoiti Borna disease virus Poliomyelitis viruses (wild and attenuated) Polioviruses (all types, wild and attenuated) Polyoma* Poxviruses (all types except Alastrim, Smallpox, and Whitepox which are in Class 5, and Monkeypox which, depending on experiment, is in Class 3 or 4) Pseudo-rabies virus Rabbitpox virus Rabies virus (all strains except Rabies "street" virus - fresh isolate which should be in Class 3) Rat leukemia* Rat mammary tumor* Reoviruses (all types) Respiratory syncytial virus Rhinoviruses (all types) Rift Valley Fever vaccine strain MP-12 Ross River virus Rotaviruses Rous sarcoma* Rubella virus (Rubivirus) Semliki Forest virus Sendai virus Shope fibroma* Shope papilloma* Simian viruses* (all types except Herpesvirus simiae - Monkey B virus, Class 4, and Marbug virus which is a Class 4 hemorrhagic fever virus) Sindbis virus 21 7.6 Classification of Agents (cont) • • • • • • • • • • • • • • • Subsclerosing panencephalitis virus SV 40 virus Tacaribe complex Tanapox complex Tensaw virus Transmissible Spongiform encephalopathies Turlock virus Vaccinia virus Varicella virus Venezuelan Equine Encephalomyelitis vaccine strain TC-83 Vescular stomatitus virus (laboratory adapted strains including VSV-Indiana, San Juan, and Glasgow) Western Equine Encephalomyelitis virus Yaba* Yabapox virus Yellow fever virus, 17D vaccine strain C. Studied in the United States Organisms which may not be except at Specified Facilities • • • Alastrim Small pox White pox 22 7.7 Biosafety Level 2 Criteria Biosafety Level 2 practices, equipment and facilities are those which are applicable to clinical, diagnostic, teaching and other facilities working with the broad spectrum of indigenous moderate-risk agents present in the community and associated with human disease of carrying severity. Activities with low aerosol potential with these agents can be conducted on the open bench using good microbiological techniques. Primary hazards to personnel working with these agents relate to accidental auto-innoculation or ingestion of infectious materials. Procedures with high aerosol potential may predictably and significantly increase the risk of exposure of personnel to infectious aerosols and must be conducted in primary containment equipment or devices. Biosafety Level 2 (BSL-2) is suitable for work involving agents of moderate potential hazard to personnel and the environment. Laboratory personnel have specific training in handling pathogenic agents and are directed by competent scientists; access to the laboratory is limited when work is being conducted; extreme precautions are taken with contaminated sharp items; certain procedures in which infectious aerosols or splashes may be created are conducted in biological safety cabinets or other physical containment equipment. The following standard and special practices apply to agents assigned to Biosafety Level 2. (note: see appendix for list of Class 2 agents) A. Standard Microbiological Practices 1. Access to the laboratory is limited or restricted at the discretion of the laboratory director when experiments are in progress. Doors are kept closed when experiments are in progress. 2. Persons wash their hands after they handle viable materials, after removing gloves, and before leaving the laboratory. 3. Eating, drinking, smoking, handling contact lenses, and applying cosmetics are not permitted in the work areas. Food is stored outside the work area in cabinets or refrigerators designated for this purpose only. 4. Mouth pipetting is prohibited; mechanical pipetting devices are used. 5. Policies for the safe handling of sharps are instituted. 6. All procedures are performed carefully to minimize the creation of splashes or aerosols. 7. Work surfaces are decontaminated on completion of work or at the end of the day and after any spill or splash of viable material with disinfectants that are effective against the agents of concern. 23 7.7 Biosafety Level 2 Criteria (cont) 8. All cultures, stocks, and other regulated wastes are decontaminated before disposal by an approved decontamination method such as autoclaving. Materials to be decontaminated outside of the immediate laboratory are placed in a durable, leak proof container and closed for transport from the laboratory. Materials to be decontaminated off-site from the facility are packaged in accordance with applicable local, state, and federal regulations, before removal from the facility. 9. An insect and rodent control program is in effect. B. Special Practices 1. Access to the laboratory is limited or restricted by the laboratory director when work with infectious agents is in progress. In general, persons who are at increased risk of acquiring infection, or for whom infection may have serious consequences, are not allowed in the laboratory. For example, persons who are immunocompromised or immunosuppressed may be at increased risk of acquiring infections, as well as children and pregnant women. The laboratory director has the final responsibility for assessing each circumstance and determining who may enter or work in the laboratory. 2. The laboratory director establishes policies and procedures whereby only persons who have been advised of the potential hazards and meet specific entry requirements (e.g., immunization) may enter the laboratory. 3. A biohazard sign must be posted on the entrance to the laboratory to indicate the use or presence of any infectious agents. Appropriate information to be posted includes the agent(s) in use, the biosafety level, the required immunizations, the investigator's name and telephone number, any personal protective equipment that must be worn in the laboratory, and any special requirements for entering or exiting the laboratory. 4. Laboratory personnel receive appropriate immunizations or tests for the agents handled or potentially present in the laboratory (e.g., hepatitis B vaccine or TB skin testing). 5. When appropriate, considering the agent(s) handled, baseline serum samples for laboratory and other at-risk personnel are collected and stored. Additional serum specimens may be collected periodically, depending on the agents handled or the function of the facility. 6. Biosafety procedures are incorporated into standard operating procedures or in a biosafety manual adopted or prepared specifically for the laboratory by the laboratory director. Personnel are advised of special hazards and are required to read and follow instructions on practices and procedures. 7. The laboratory director ensures that laboratory and support personnel receive appropriate training on the potential hazards associated with the work involved, the necessary precautions to prevent exposures, and the exposure evaluation procedures. Personnel receive annual updates or additional training as necessary for procedural or policy changes. 24 7.7 Biosafety Level 2 Criteria (cont) 8. A high degree of precaution must always be taken with any contaminated sharp items, including needles and syringes, slides, pipettes, capillary tubes, and scalpels. a. Needles and syringes or other sharp instruments should be restricted in the laboratory for use only when there is no alternative. Plasticware should be substituted for glassware whenever possible. b. Only needle-locking syringes or disposable syringe needle units (i.e., needle is integral to the syringe) are used for injection or aspiration of infectious materials. Used disposable needles must not be bent, sheared, broken, recapped, removed from disposable syringes, or otherwise manipulated by hand before disposal; rather, they must be carefully placed in conveniently located puncture-resistant containers used for sharps disposal. Non-disposable sharps must be placed in a hard-walled container for transport to a processing area for decontamination, preferably by autoclaving. c. Syringes which re-sheathe the needle, needleless systems, and other safety devices are used when appropriate. d. Broken glassware must not be handled directly by hand, but must be removed by mechanical means such as a brush and dustpan, tongs, or forceps. Containers of contaminated needles, sharp equipment, and broken glass are decontaminated before disposal, according to any local, state, or federal regulations. 9. Cultures, tissues, specimens of body fluids, or potentially infectious wastes are placed in a leakproof container with cover that prevents leakage during collection, handling, processing, storage, transport, or shipping. Note: waste collected in biohazard bags must be transported in leakproof container to the autoclave. The leakproof container must be periodically disinfected but need not be autoclaved. 10. Laboratory equipment and work surfaces should be decontaminated with an effective disinfectant on a routine basis, after work with infectious materials is finished, and especially after overt spills, splashes, or other contamination by infectious materials. Contaminated equipment must be decontaminated according to any local, state, or federal regulations before it is sent for repair or maintenance or packaged for transport in accordance with applicable local, state, or federal regulations, before removal from the facility. (See UofG Biosafety Policy). 11. Spills and accidents that result in overt exposures to infectious materials are immediately reported to the laboratory director. Medical evaluation, surveillance, and treatment are provided as appropriate and written records are maintained. 12. Animals not involved in the work being performed are not permitted in the lab. 25 7.7 Biosafety Level 2 Criteria (cont) C. Safety Equipment (Primary Barriers) 1. Properly maintained biological safety cabinets, preferably Class II, or other appropriate personal protective equipment or physical containment devices are used whenever: a. Procedures with a potential for creating infectious aerosols or splashes are conducted. These may include centrifuging, grinding, blending, vigorous shaking or mixing, sonic disruption, opening containers of infectious materials whose internal pressures may be different from ambient pressures, inoculating animals intranasally, and harvesting infected tissues from animals or embryonate eggs. b. High concentrations or large volumes of infectious agents are used. Such materials may be centrifuged in the open laboratory if sealed rotor heads or centrifuge safety cups are used, and if these rotors or safety cups are opened only in a biological safety cabinet. 2. Face protection (goggles, mask, face shield or other splatter guard) is used for anticipated splashes or sprays of infectious or other hazardous materials to the face when the microorganisms must be manipulated outside the BSC. 3. Protective laboratory coats, gowns, smocks, or uniforms designated for lab use are worn while in the laboratory. This protective clothing is removed and left in the laboratory before leaving for non-laboratory areas (e.g., cafeteria, library, administrative offices). All protective clothing is either disposed of in the laboratory or laundered by the institution; it should never be taken home by personnel. 4. Gloves are worn when hands may contact potentially infectious materials, contaminated surfaces or equipment. Wearing two pairs of gloves may be appropriate. Gloves are disposed of when overtly contaminated, and removed when work with infectious materials is completed or when the integrity of the glove is compromised. Disposable gloves are not washed, reused, or used for touching "clean" surfaces (keyboards, telephones, etc.), and they should not be worn outside the lab. Alternatives to powdered latex gloves should be available. Hands are washed following removal of gloves. D. Laboratory Facilities (Secondary Barriers) 1. Provide lockable doors for facilities that house restricted agents. 2. Consider locating new laboratories away from public areas. 3. Each laboratory contains a sink for hand washing. 4. The laboratory is designed so that it can be easily cleaned. Carpets and rugs in laboratories are inappropriate. 26 7.7 Biosafety Level 2 Criteria (cont) 5. Bench tops are impervious to water and are resistant to moderate heat and the organic solvents, acids, alkalis, and chemicals used to decontaminate the work surfaces and equipment. 6. Laboratory furniture is capable of supporting anticipated loading and uses. Spaces between benches, cabinets, and equipment are accessible for cleaning. Chairs and other furniture used in laboratory work should be covered with a non-fabric material that can be easily decontaminated. 7. Install biological safety cabinets in such a manner that fluctuations of the room supply and exhaust air do not cause the biological safety cabinets to operate outside their parameters for containment. Locate biological safety cabinets away from doors, from windows that can be opened, from heavily traveled laboratory areas, and from other potentially disruptive equipment so as to maintain the biological safety cabinets' air flow parameters for containment. 8. An eyewash station is readily available. 9. Illumination is adequate for all activities, avoiding reflections and glare that could impede vision. 10. There are no specific ventilation requirements. 27 7.8 Biological Safety Cabinets Biological safety cabinets (BSCs) are among the most effective, as well as the most commonly used primary containment devices in laboratories working with infectious agents. The three general types available (Class I, II, III) have various performance characteristics and applications Class I Biological safety cabinet is designed for general microbiological research with low and moderate risk agents, and is useful for containment of mixers, blenders, and other equipment. These cabinets are not appropriate for handling research materials that are vulnerable to airborne contamination, since the inward flow of unfiltered air from the laboratory can carry microbial contaminants into the cabinet. Class II Biological safety cabinets, (also called tissue culture hoods and biosafety cabinets), provide personnel, environmental and product protection. As the diagram of the biosafety cabinet shows, room air is drawn around the operator into the front grille of the cabinet. This provides personnel protection by preventing contaminated air from spilling out. In addition, the downward laminar flow of HEPA-filtered air provides a sterile environment for tissue cultures by minimizing the chance of cross-contamination along the work surface of the cabinet. Room air passes through the front grille and then flows upward through a plenum at each side of the cabinet, and through the supply HEPA filter and then downward to the work area through a back-pressure plate. Because air leaving the cabinet through the top of the unit has passed through a HEPA filter, it is particle-free. 28 7.8 Biological Safety Cabinets (cont) The Class II Biological safety cabinet is designed with inward air flow at a velocity to protect personnel (75-100 lfpm), HEPA-filtered vertical laminar airflow for product protection, and HEPA-filtered exhaust air for environmental protection. Class II BSCs are classified into two types (A and B) based on construction, air flow velocities and patterns, and exhaust systems. Basically, Type A cabinets are suitable for work with microbiological research in the absence of volatile or toxic chemicals and radionuclides, since air is recirculated within the work area. Type A cabinets may be exhausted through HEPA filters into the laboratory, or to the outside via a 'thimble' connection to the exhaust ductwork. Type B cabinets are further sub-typed into types B1 , B2, and B3. Type B cabinets are hardducted to the exhaust system, and contain negative pressure planes. These features, plus an increased face velocity of 100 lfpm, allow work to be done with toxic chemical or radionuclides. 29 7.8 Biological Safety Cabinets (cont) Class III Biological safety cabinet all operations in the work area of the cabinet are performed through the attached rubber gloves. The Class III cabinet is operated under negative pressure. Air supply is HEPA-filtered, and the cabinet exhaust air is filtered by two HEPA filters in series, or HEPA filtration followed by incineration, before discharge outside the facility . The Class III Biological safety cabinet is a totally enclosed, ventilated cabinet of gas-tight construction and offers the highest degree of personnel and environmental protection from infectious aerosols, as well as protection of research materials from microbiological contaminants. Class III cabinets are most suitable for work with hazardous agents that require Biosafety Level 3 or 4 containment. Horizontal Laminar Flow "Clean Bench" Horizontal Laminar flow clean air benches are not BSCs. They discharge HEPA-filtered air across the work surface and toward the user. These devices only provide product protection. They can be used for certain clean activities, such as the dust-free assembly of sterile equipment or electronic devices. These benches should never be used when handling cell culture materials or drug formulations, or when manipulating potentially infectious materials. The worker can be exposed to materials (including proteinaceous antigens) being manipulated on the clean bench, which may cause hypersensitivity. Horizontal clean air benches should never be used as a substitute for a biological safety cabinet in research, biomedical or veterinary laboratories and/or applications. Vertical Laminar Flow "Clean Bench" Vertical Laminar flow clean benches are also not BSCs. They may be useful, for example, in hospital pharmacies when a clean area is needed for preparation of intravenous drugs. While these units generally have a sash, the air is usually discharged into the room under the sash, resulting in the same potential problems as the horizontal laminar flow clean benches. 30 7.8 Biological Safety Cabinets (cont) Utility Services in biological safety cabinet Utility services needed within a BSC must be planned carefully. The protection of vacuum systems must be addressed. Electrical outlets inside the cabinet must be protected by ground fault circuit interrupters and should be supplied by an independent circuit. When propane gas is provided, a clearly marked emergency gas shut-off valve outside the cabinet must be installed for fire safety. All non-electrical utility services should have exposed, accessible shut-off valves. As a rule, propane gas burners should not be operated in a BSC. They disrupt the air flow pattern and may pose fire hazards. Ultraviolet Lamps in biological safety cabinet Ultraviolet (UV) lamps are not required in BSCs. If installed, UV lamps must be cleaned weekly to remove any dust and dirt that may block the germicidal effectiveness of the ultraviolet light. The lamps should be checked periodically with a meter to ensure that the appropriate intensity of UV light is being emitted. A sign must be placed on the entrance door when a UV lamp is operating. UV lamps must be turned off when the room is occupied to protect eyes and skin from UV exposure, which can burn the cornea and cause skin cancer. Biosafety Cabinet Work Practices 1. Plan procedures carefully. 2. Start-up the biosafety cabinet and let it run at least 5-10 minutes before beginning to work. 3. Do not overload cabinet. Separate clean from contaminated items (work from clean to dirty). 4. Wear gloves and long sleeved lab coats. 5. Decontaminate the cabinet with disinfectant before and after work is completed. 6. Protect vacuum system by trap. 7. Avoid disruption of airflow (turbulence); extra items storage and movement in and around the cabinet. 8. Perform work 10-15 cm. back from the front intake grille. 9. Equipment that causes turbulence should be placed in back 1/3 of work surface. Do not block the back grille. 10. Avoid use of flame. Turbulence and filter damage may occur. 11. Avoid use of UV light. 12. Check the periodical test performance sticker affixed on the cabinet. 31