* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 1- Functional anatomy and mechanical properties of heart
Survey
Document related concepts
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
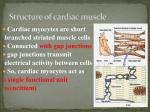
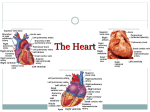
Babylon University College of Medicine Department of physiology Dr. Ghafil Saihood Hassan 2016 - 2017 1- Functional anatomy of heart. Objectives: 1. Explain the functions of the heart. 2. Describe the flow of blood through the heart. 3. Explain the functions of the heart valves. Heart chambers and function of valves: The heart acts as two separate pumps, right and left sides. There are four valves in the heart; two are called atrioventricular valves (mitral and tricuspid valves). These valves open during ventricular diastole to allow blood to fill the ventricles and close during ventricular systole. Other two valves are called semilunar valves (aortic and pulmonary valves). These valves open during systole to allow eject blood from the ventricles into the aorta or pulmonary artery and close during diastole. See figure 1. Figure (1): Structure of heart. (Hall, 2016). Papillary muscles that attach to the vanes of the A-V valves by the chordae tendinae, contract when the ventricular walls contract. They pull the valves inward toward the ventricles to prevent their bulging too far backward toward the atria during ventricular contraction. If chordae tendinea becomes ruptured or paralyzed the valve bulges far backward. See figure 2. 1 Figure (2): Heart valve (Hall, 2016). Both ventricles pump the same volume of blood to systemic and pulmonary circulation. The right ventricle pumps blood to pulmonary circulation at low pressure. While the left ventricle pumps blood through the systemic circulation at high pressure. The left ventricle has a thicker wall than the right ventricle because of the higher pressure in the systemic circulation. About 75% of the blood flow directly through the atria into the ventricles even before the atria contract. The atrial contraction causes an additional 25% filling the ventricles that increase the ventricular pumping effectiveness as much as 25%. The heart can continue to operate even without this extra blood in resting. Blood supply of the heart: The heart is supplied by two coronary arteries (right and left) distal to the aortic valve. Coronary veins drain into a single large vein, then coronary sinus, which drain into the right atrium. Nerve supply of the heart: The heart is innervated by both sympathetic and parasympathetic fibers. The sympathetic fibers innervate the SA node, AV node and muscle fibers in the atria and ventricles. Sympathetic stimulation through B1 increases heart rate (positive chronotropic effect) by formation of cyclic adenosine mono-phosphate (cAMP) that opens Na channels. It increases the force of contractility (positive inotropic effect) of muscle fibers in the atriums and ventricles Parasympathetic fibers innervate the heart through vagus nerve. The right vagus nerve enervates SA node while left vagus nerve enervates AV node. It causes lowering the heart rate through M2 receptors (negative chronotropic effect) by decrease cAMP. See figure3. 2 Figure (3): Nerve supply of heart (Hall, 2016) The cardiac cycle: The cardiac events that occur from the beginning of one heartbeat to the beginning of the next are called cardiac cycle. If the heart rate is 75 beats/minute, the duration of cardiac cycle is 0.8 second (0.5 s for diastole, 0.3 s for systole). Increased heart rate leads to decrease in cardiac cycle time (systole and diastole), but a decrease in diastolic time is more. It is not beneficial to body to increase heart rate above 200 beats / minute, because lowering diastolic time will not leave sufficient time to fill the ventricle, so this will decrease stroke volume. The cardiac cycle starts by atrial systole followed by ventricular systole then by diastole of the whole heart. Effect of changes in the ionic composition of blood on heart: Effect of potassium ions: The normal concentration of potassium (K+) in extracellular fluid is 3.5 – 5.5 meq /L. Excess potassium causes the heart to become flaccid and dilated, and slows the heart rate. Large quantities can block conduction of the cardiac impulse from the atria to the ventricles through AV node. Chronic hyperkalaemia which arise during renal failure, acidosis, potassium overloading or during RBC haemolysis produce sever cardiac abnormal rhythm that can cause death. Conversely a decrease in the plasma K levels (Hypokalemia) is serious condition but it is not as rapidly fatal as hyperkalemia. The rest- membrane potential of muscle fibers decreases as the extra cellular K concentration increase. The fiber becomes unexcitable, heart stops in diastole. Effect of sodium ions: Low plasma level of Na ions may be associated with low voltage in ECG. Plasma sodium concentration range is normally regulated with in close limit of 140 to 145 mEq/L. Effect of calcium ions: The normal concentration of calcium ions in the extracellular fluid is remains constant level is 10.0 mg/dl with range (8.5 – 10.5 mg/dl). Increase in extracellular Ca2+ concentration enhances myocardial 3 contractility. Conversely, deficiency of calcium ions causes cardiac flaccidity, similar to high potassium. Fortunately, calcium ion levels in the blood normally are regulated within a very narrow range. Properties of cardiac muscle: Figure 4 shows a typical histological picture of cardiac muscle. The cardiac muscle fibers are striated, branching, interdigitating, and cardiac cell contains large elongated mitochondria. Cardiac muscle fibers are approximately 15µm in diameter and 100 µm in length. They contain intercalated disks that separate individual cardiac muscle cells from one another. The heart is composed of three major types of cardiac muscle cells: 1- Excitatory muscle cells. 2- Contractive muscle cells. 3- Conductive muscle cells. Cardiac muscle junctions: 1- Desmosomes junction; which provides strong union between muscle cells. 2- Gap junction; which provides low resistance bridge for the spread of excitation from one cell to another that allow free diffusion of ions. So that action potentials travel from cardiac cell to the next. The heart is composed of two syncytiums: the atrial syncytium and the ventricular syncytium. This allows the atria to contract a short time before ventricular contraction, which is important for effectiveness of heart pumping. The atrium is separated from the ventricle by fibrous tissue except the atriaventricular opening which is called AV node to prevent spread of excitation, Figure (4): Structure of cardiac muscle (Guyton & Hall 2006). Spread of cardiac excitation: Figure 4 shows the structures of conducting system, they are: 1-The sino-atrial node (SA node) with speed (0.05 m/s). 2- The internodes atrial pathway with speed (1 m/s). 3- The atrio-ventricular node (AV node) with speed (0.05 m/s). 4-The bundle of His and its branches with speed (1 m/s). 4 5- Purkinje fibers, with speed (4 m/s), see figure 5. Figure (5): The structures of conducting system. (Hall, 2016). The SA node is the normal cardiac pace maker. Impulses generated in the SA node pass through atrial pathway to AV node, through this node to the bundle of His. The bundle divides to right and left branches. Each branch ends with purkinje fibers which spread downward toward the apex of the ventricle then turn around each ventricular chamber and back toward the base of the heart to supply the ventricular muscle fibers. The atrial depolarization is completed in about 0.1 second. The conduction in AV node is slow about 0.1 second due to small size of muscle fibers and diminished numbers of gap junctions. This delay is shortened by stimulation of sympathetic nerves to heart and lengthened by stimulation of vague nerve. See figure 6. Figure (6): AV node structure. Correlation between muscle fiber length and tension: The initial length of the fibers is determined by the degree of diastolic filling of the heart, and the pressure developed in the ventricle. It is proportional to the 5 volume of the ventricle at end of the filling phase (Starling' law of the heart). The force of contraction of cardiac muscle can be also increased by catecholamine and this increase occurs without a change in muscle length. This positive inotropic effect of catecholamine is mediated via innervated β1-adrenergic receptors. Excitation-contraction coupling: The mechanism of excitation-contraction coupling is the same as that for skeletal muscle, but there is a second effect that is quite different. In addition to the sarcoplasmic reticulum calcium, a large quantity of extra calcium ions diffuse into the sarcoplasm through the T tubule which has a volume 25 times as great in skeletal muscle. Calcium ions diffuse to the interior of the cardiac cells when the action potential occurs. The wall T tubule contains dihydropyridine (DHP) receptors, which open calcium channels. Calcium ions enter ICF. The strength of contraction is hardly affected by change in extracellular fluid calcium concentration. At the end of the cardiac action potential, the calcium ions in the interior of the muscle fiber are suddenly pumped back out of the muscle fibers into sarcoplasmic reticulum and the T tubes. As a result the contraction then ceases until a new action potential occurs The basic unit of contraction is the sarcomere (2 µm in length) which giving a striated appearance due to the Z lines. During contraction, the shorting of the sarcomere results from the interdigitation of the actin and myosin molecules. The mechanical properties of the heart was studied in 1895 by two physiologists; Otto Frank (German, on isolated frog heart) and Ernest Starling (English, dog isolated heart-lung), both have reached the same results, they created the Frank-Starling law Energy of contraction is proportional to the initial length of the cardiac muscle fibers. 6