* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Grade 2008-2010 final exam-B
Survey
Document related concepts
Psychedelic therapy wikipedia , lookup
Specialty drugs in the United States wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Drug discovery wikipedia , lookup
Orphan drug wikipedia , lookup
Discovery and development of beta-blockers wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Transcript
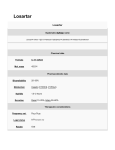
Pharmacology Exam for Grade 2008 Pakistan Students (Exam 2) — Part Ⅰ Single Choice Questions (50 points) 1. Which one of the following aggravates a digitalis induced arrhythmia? A. Decreased serum calcium B. Decreasing heart rate with propranolol C. Decreased serum sodium D. Decreased serum potassium E. Decreased serum angiotensin Ⅱ 2. Which one of the following is the most serious main side effect of statins and this effect would be increased if a statin is taken with ciclosporin, gemfibrozil or nicotinic acid. A. Gastrointestinal problems B. Rhabdomyolysis C. Elevated blood pressure D. Migraine headaches E. palpitations 3. The mechanism of anti-hypertensive effect of losartan is: A. decrement of renin activity B. inhibition of angiotensin converting enzyme C. blockade of the angiotensin Ⅱ receptors D. increment of bradykinin synthesis E. causing vasodilation directly 4. Captopril can do all of the following EXCEPT A. inhibiting ACE B. causing dry cough C. inhibit the formation of angiotensin Ⅱ D. promote the excretion potassium E. increase bradykinin concentration in the blood 5. Which of the following drugs is not suitable to treat the patient with angina pectoris accompanied with asthma? A. Nifedipine B. Propranolol C. Nitroglycerin D. Verapamil E. Isosorbide dinitrate 6. Which of the following statements about the treatment of chronic heart failure is wrong? A. Patients with evidence of fluid retention should receive a diuretic. B. Treatment with an ACE inhibitor and a β-R blocker should be initiated and maintained unless specifically contraindicated. C. Digoxin may be added if needed to reduce symptoms or to slow the ventricular repsonse in patients with rapid atrial fibrillation. D. Patients with severe heart failure should also receive a β-R blocker E. Spironolactone may reduce mortality in patients with severe heart failure 7. The therapeutic action of β-adrenergic receptor blockers such as propranolol in angina pectoris is believed to be primarily the result of A. Reduced production of catecholamines B. Dilation of the coronary vasculature C. Decreased requirement for myocardial oxygen D. Increased peripheral resistance E. Increased sensitivity to catecholamines 8. A 58-year-old patient with a history of hypertension and congestive heart failure administrating some drugs, now he complains of nausea, blurred vision and bradycardia, intoxication of glycoside is suspected, then digoxin is stopped, which of the following drugs also must be stopped? A. nifedipine B. diazoxide C. hydrochlorothiazide D. prazosin E. clonidine 9. All of the following measures can be used in the treatment of digoxin-induced arrhythmias except A. stopping digoxin administration B. diuretic agents such an furosemide is used to improve excretion C. phenytoin administration D. atropine administration E. lidocaine administration 10. Which of the following is not the adverse reaction of cardiac glucosides A. anorexia, nausea, vomiting, diarrhea B. blurred vision C. tachycardia D. bradycardia E. hyperkalemia 11.Which of the following symptoms is a withdrawal syndrome of glucocorticoids? A. Induction and aggravation of infections B. Iatrogenic adrenocortical insufficiency C. central obesity D. Hypertension E. Osteoporosis 12. Among the following anti-inflammatory mechanisms of glucocorticoids, which one can commonly be observed ? A. Increased influx of leukocytes to the site of inflammation B. Reduced expression of ACEI C. Reduced capillary permeability and edema at the inflammatory site D. Increased prostaglandin formation E. Enhanced formation of pro-inflammatory interleukins 13. A 60-year-old diabetic male is treated with insulin plus pioglitazone, what is the mechanism of the latter? A. Increased release of endogenous insulin B. Decreased plasma glucagon levels C. Increased hepatic gluconeogenesis D. Increased target tissue sensitivity to insulin E. Decreased intestinal absorption of glucose 14. Which of the following hypoglycemic drugs can inhibit α-glycosidase? A. insulin B. glyburide C. pioglitazone D. acarbose E. metformin 15. All of the following drugs can be used in peptic ulcer except A. Sodium bicarbonate B. Aluminium hydroxide C. Cimetidine D. aminophylline E. Sucralfate 16. Glucocorticoids can be used to treat severe bacterial infections the reason is A. they can act as good antimicrobials B. they are able to enhance the immunity C. the phagocytic ability of neutrophils can be promoted by these drugs D. they possess anti-inflammatory and antitoxic action E. they produce a synergistic action with antibacterisl drugs 17. Which of the following drugs CANNOT inhibit platelet aggregation A. Dipyridamole B. Aspirin C. Ticlopidine D. Streptokinase E. Ticlopidine 18. The best drug used in treating iron deficiency anemia is A. Epo B. Vitamin B12 C. Iron D. Folic acid E. GCS 19. The drug which is useful in treatment of peptic ulcer caused by aspirin is A. Al(OH)3 B. Misoprostol C. Omeprazole D. Pirenzepine E. Cimetidine 20. The anti-asthmatic effect of Salbutamol is attributed to A. inhibition of intracellular cGMP B. blockade of M-receptor C. activation of adenylate cyclane D. stimulation of β2 receptor E. inhibition of phosphodiesterase 21. The most serious adverse effect of chloramphenicol is A. allergic reaction B. GI tract reaction C. aplastic anemia D. hepatic necrosis E. renal toxicity 22. Which of the following drugs may cause superinfections? A. penicillin G B. streptomycin C. erythromycin D. tetracycline E. neomycin 23. Which of following drugs prevents synthesis of cell-wall, but does not belong to β-lactam antibiotics A. penicillin G B. vancomycin C. carbenicillin D. cefaclor E. amoxycillin 24. All of the following antibiotics act by interfering with protein synthesis except A. tetracycline B. streptomycin C. chloramphenicol D. penicillin G E. clindamycin 25. Which drug can treat pseudomembranous enterocolitis caused by lincomycin A. penicillin G B. carbenicillin C. chloramphenicol D. vancomycin E. ciprofloxacin PART Ⅱ Please explain the following pharmacological terms(20 points,4/item) 1. Post antibiotic effect 2. Chemotherapeutic index 3. Superinfection 4. Resistance 5. Antimicrobial activity PART ⅢAssay Questions (30 points, 10/item) 1.Please describe the clinical uses of β-receptor antagonists. 2. Please tell the probable adverse reactions after long-time and high-dose use of glucocorticoids? 3. Please describe the common adverse reactions of aminoglycosides. Answers: Part Ⅰ 1.D 14.D 2.B 15.D 3.C 4.D 16.D 5.B 17.D 6.D 18.C 7.C 8.C 19.B 20.D 9.B 10.E 21.C 22.D 11.B 12.C 23.B 13.D 24.D 25. D Part Ⅱ 1.Postantibiotic effect (PAE): Persistent suppression of bacterial growth after limited exposure to an antimicrobial agent 2. CI=LD50/ED50, used to judge the value and safety of a chemotherapeutic drug 3. Superinfection: modify the normal flora , living in vagina or enteron or oral cavity, with suppression susceptible microorganiams, overgrowth of unsusceptible microorganiams can cause various new infections. 4.Drug resistance is the phenomenon that susceptibility of pathogenic microorganisms to drugs becomes lower or even loses after the microorganisms contact with drugs for many times. As a result, the antimicrobial effect of the drugs will decrease or even disappear. 5. Antimicrobial activity:is the ability that an antimicrobial agent kills or suppresses the growth of microorganisms Part Ⅲ 1. Please describe the clinical uses of β-receptor antagonists. (1) hypertension (2) CHF (3) Angina pectoris (4) Arrhythmia (5) Others: hyperthyroidism 2. Please tell the probable adverse reactions after long-time and high-dose use of glucocorticoids? (1)Iatrogenic Cushing’s syndrome: mainly caused by metabolism disorder of lipid, protein, glucose and water-electrolyte. The symptoms include sodium retention, hypokalemia, hypertension, moon face, bump back, diabetes, muscle wasting. (2)Induction and aggravation of infection (3)Possible risk of peptic ulcers (4)Cardiovascular complications: such as hypertension and arteriolosclerosis (5)Osteoporosis (6)Other complications: acute psychosis, hypomania, growth retardation and so on. 3. Please describe the common adverse reactions of aminoglycosides. (1) Ototoxicity:Cochlear damage;Vestibular damage (2) Nephrotoxicity (3) Neuromuscular junction blockade (4)Allergic reactions