* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Transposition of the great arteries with atrial switch versus arterial
Survey
Document related concepts
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Aortic stenosis wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Atrial septal defect wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
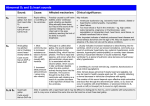
TGA – atrial vs arterial switch what do we need to look for and how to react Folkert Meijboom, MD, PhD, FESC Dept Cardiology University Medical Centre Utrecht The Netherlands www.escardio.org/guidelines TGA + atrial switch: Follow-up ● All patients should be seen at least annually in a specialized GUCH centre. Frequent complications to look for: ● RV dysfunction ● Dilatation of the RV resulting in TR ● Baffle – related problems ● Stenosis ● leakage www.escardio.org/guidelines TGA atrial switch ● routine check-up: – Once a year ● History ● Physical examination ● ECG ● Echo – On indication ● Holter, CMR/CT, cardiac cath www.escardio.org/guidelines TGA atrial switch Physical examination ● Physical examination – Signs of venous congestion ● Either heart failure ● Or obstruction systemic venous return ● baffle obstruction www.escardio.org/guidelines TGA atrial switch Physical examination ● Physical examination – Signs of venous congestion ● Either heart failure ● Or obstruction systemic venous return ● baffle obstruction ● Specific imaging: TTE, TEE, CMR, CT www.escardio.org/guidelines TGA atrial switch Physical examination ● RV impuls – precordial heave ● Auscultation: – Normal first heart sound – Single loud second heart sound – aorta anterior – Usually no murmur ● If murmur appears: development of TR; – sign of worsening systemic ventricle =RV www.escardio.org/guidelines TGA atrial switch Physical examination ● RV impuls – precordial heave ● Auscultation: – Normal first heart sound – Single loud second heart sound – aorta anterior – Usually no murmur ● If murmur appears: development of TR; – sign of worsening systemic ventricle =RV – Imaging – echo, CMR -consider treatment www.escardio.org/guidelines Indications for Intervention in Transposition of the Great Arteries After Atrial Switch (1) Classa Levelb Indications for surgical intervention ● Valve repair or replacement should be performed in patients with severe symptomatic systemic (tricuspid) AV valve regurgitation without significant ventricular dysfunction (RVEF ≥ 45%) ● Significant systemic ventricular dysfunction, with or without TR, should be treated conservatively or eventually with cardiac transplantation ● LVOTO if symptomatic or if LV function deteriorates should be treated surgically ● In symptomatic pulmonary venous obstruction surgical repair (catheter intervention rarely possible) should be performed. ● Symptomatic patients with baffle stenosis not amenable for catheter intervention should be treated surgically ● Symptomatic patients with baffle leaks not amenable for catheter intervention should be treated surgically. ● Valve repair or replacement should be considered for severe asymptomatic systemic (tricuspid) AV valve regurgitation without significant ventricular dysfunction (RVEF ≥ 45%) ● Pulmonary artery banding in adult patients, to create septal shift, or a left ventricular training with subsequent arterial switch, is currently experimental and should be avoided. I C I C I C I C I C I C IIa C III C a = class of recommendation. b = level of evidence. AV = atrioventricular; L-R shunt = left-to-right shunt; LV = Left ventricle; LVOTO = left ventricular outflow tract obstruction; RVEF = right ventricular ejection fraction; TR = tricuspid regurgitation. www.escardio.org/guidelines TGA atrial switch ECG ● sinus rhythm or narrow-QRS escape rhythm and RVH. ● Sinus node dysfunction with slow heart rate can occur ● Atrial flutter with a 2:1 or 3:1 conduction is freequently seen ● all types of arrhythmia can occur www.escardio.org/guidelines TGA atrial switch arrhythmia: how to react ● Sinus node dysfunction with slow heart rate can occur – PM indication as in normal hearts – Transvenous pacing: ● PM lead through baffle in remnant LA with left auricle ● PM lead in left auricle – Good and stable position; easy to reach – AAI pacing often good enough – AV conduction not compromised www.escardio.org/guidelines TGA atrial switch arrhythmia: how to react ● Sinus node dysfunction with slow heart rate can occur – PM indication as in normal hearts – Transvenous pacing: ● PM lead through baffle in remnant LA with left auricle ● PM lead in left auricle – Good and stable psoition; easy to reach – AAI pacing often good enough – AV conduction not compromised Beware baffle narrowing, possibly compromised by PM lead www.escardio.org/guidelines TGA atrial switch arrhythmia: how to react ● Sinus node dysfunction with slow heart rate can occur – PM indication as in normal hearts – Transvenous pacing: ● PM lead through baffle in remnant LA with left auricle ● PM lead in left auricle – Good and stable psoition; easy to reach – AAI pacing often good enough – AV conduction not compromised Visualization baffles before PM placement – CMR or TEE www.escardio.org/guidelines TGA atrial switch arrhythmia: how to react ● Sinus node dysfunction with slow heart rate can occur – PM indication as in normal hearts – Transvenous pacing: ● PM lead through baffle in remnant LA with left auricle ● PM lead in left auricle – Good and stable psoition; easy to reach – AAI pacing often good enough – AV conduction not compromised In case of severe narrowing baffle? www.escardio.org/guidelines Indications for Intervention in Transposition of the Great Arteries After Atrial Switch (2) Classa Levelb Indications for catheter intervention ● Stenting should be performed in symptomatic patients with baffle stenosis I C ● Stenting (covered) or device closure should be performed in symptomatic patients with baffle leaks and substantial cyanosis at rest or during exercice I C ● Stenting (covered) or device closure should be performed in patients with baffle leaks and symptoms due to L-R shunt I C ● Stenting (covered) or device closure should be considered in asymptomatic patients with baffle leaks with substantial ventricular volume overload due to LR shunt I C ● Stenting should be considered in asymptomatic patients with baffle stenosis who require a PM treatment IIa C ● Stenting may be considered in other asymptomatic patients with baffle stenosis IIb C a = class of recommendation. b = level of evidence. AV = atrioventricular; L-R shunt = left-to-right shunt; LV = Left ventricle; LVOTO = left ventricular outflow tract obstruction; PM = pacemaker; RVEF = right ventricular ejection fraction; TR = tricuspid regurgitation. www.escardio.org/guidelines TGA atrial switch PM & conduction disturbances ● AV conduction compromised/questionnable? – Also PM wire in ventricle ● Smooth-walled LV – screw-in electrode ● 2 wires in baffles – beware of narrowing!! www.escardio.org/guidelines TGA atrial switch: echo ● ventricular function www.escardio.org/guidelines Parasternal long axis: RV and LV function www.escardio.org/guidelines Parasternal long axis: RV and LV function www.escardio.org/guidelines Parasternal long axis: M-mode www.escardio.org/guidelines TGA atrial switch: echo – ventricular function L www.escardio.org/guidelines R Indications for Intervention in Transposition of the Great Arteries After Atrial Switch (1) Classa Levelb Indications for surgical intervention ● Valve repair or replacement should be performed in patients with severe symptomatic systemic (tricuspid) AV valve regurgitation without significant ventricular dysfunction (RVEF ≥ 45%) ● Significant systemic ventricular dysfunction, with or without TR, should be treated conservatively or eventually with cardiac transplantation ● LVOTO if symptomatic or if LV function deteriorates should be treated surgically ● In symptomatic pulmonary venous obstruction surgical repair (catheter intervention rarely possible) should be performed. ● Symptomatic patients with baffle stenosis not amenable for catheter intervention should be treated surgically ● Symptomatic patients with baffle leaks not amenable for catheter intervention should be treated surgically. ● Valve repair or replacement should be considered for severe asymptomatic systemic (tricuspid) AV valve regurgitation without significant ventricular dysfunction (RVEF ≥ 45%) ● Pulmonary artery banding in adult patients, to create septal shift, or a left ventricular training with subsequent arterial switch, is currently experimental and should be avoided. I C I C I C I C I C I C IIa C III C a = class of recommendation. b = level of evidence. AV = atrioventricular; L-R shunt = left-to-right shunt; LV = Left ventricle; LVOTO = left ventricular outflow tract obstruction; RVEF = right ventricular ejection fraction; TR = tricuspid regurgitation. www.escardio.org/guidelines TGA atrial switch: echo ● ventricular function ● Baffles: – Patency – Leakages – Indication for intervention? www.escardio.org/guidelines Indications for Intervention in Transposition of the Great Arteries After Atrial Switch (2) Classa Levelb Indications for catheter intervention ● Stenting should be performed in symptomatic patients with baffle stenosis I C ● Stenting (covered) or device closure should be performed in symptomatic patients with baffle leaks and substantial cyanosis at rest or during exercice I C ● Stenting (covered) or device closure should be performed in patients with baffle leaks and symptoms due to L-R shunt I C ● Stenting (covered) or device closure should be considered in asymptomatic patients with baffle leaks with substantial ventricular volume overload due to LR shunt I C ● Stenting should be considered in asymptomatic patients with baffle stenosis who require a PM treatment IIa C ● Stenting may be considered in other asymptomatic patients with baffle stenosis IIb C a = class of recommendation. b = level of evidence. AV = atrioventricular; L-R shunt = left-to-right shunt; LV = Left ventricle; LVOTO = left ventricular outflow tract obstruction; PM = pacemaker; RVEF = right ventricular ejection fraction; TR = tricuspid regurgitation. www.escardio.org/guidelines Indications for Intervention in Transposition of the Great Arteries After Atrial Switch (2) Classa Levelb Indications for catheter intervention ● Stenting should be performed in symptomatic patients with baffle stenosis I C ● Stenting (covered) or device closure should be performed in symptomatic patients with baffle leaks and substantial cyanosis at rest or during exercice I C ● Stenting (covered) or device closure should be performed in patients with baffle leaks and symptoms due to L-R shunt I C ● Stenting (covered) or device closure should be considered in asymptomatic patients with baffle leaks with substantial ventricular volume overload due to LR shunt I C ● Stenting should be considered in asymptomatic patients with baffle stenosis who require a PM treatment IIa C ● Stenting may be considered in other asymptomatic patients with baffle stenosis IIb C a = class of recommendation. b = level of evidence. AV = atrioventricular; L-R shunt = left-to-right shunt; LV = Left ventricle; LVOTO = left ventricular outflow tract obstruction; PM = pacemaker; RVEF = right ventricular ejection fraction; TR = tricuspid regurgitation. www.escardio.org/guidelines TGA atrial switch ● routine check-up: – Once a year ● History ● Physical examination ● ECG ● Echo – On indication ● Holter, CMR/CT, cardiac cath www.escardio.org/guidelines TGA + atrial switch (Mustard/Senning): Diagnostic Work-up ● Echocardiography: first line diagnostic technique providing systemic and sub-pulmonary ventricular size and function, subpulmonary outflow tract obstruction, TR, leakage or obstruction of the atrial baffles and assessment of pulmonary venous return. SVC stenosis is, however, mostly difficult to assess and may require TEE. Contrast echo is helpful for baffle leakage or stenosis. ● CMR (CT): indicated for assessment of systemic RV function and patency of the atrial baffles. ● Holter monitoring, event recorder: required for selected patients (high-risk, investigated for suspected or clinical arrhythmia) ● Cardiac catheterization: indicated when non-invasive assessment is inconclusive or PAH requires evaluation. If something comes out; possible candidate for EP or ablation?? www.escardio.org/guidelines TGA + atrial switch (Mustard/Senning): EP Testing, Ablation and ICD ● These procedures are complicated by the fact that the atria are not normally accessible for catheters and “normal” EP procedures because of the course of the baffles and should only be done in specialised centres with specific expertise. ● Patients are at increased risk of SCD. Atrial tachyarrhythmia, impaired systemic RV function and QRS duration ≥ 140msec have been reported to be risk factors. See general recommendations for ICD implantation. www.escardio.org/guidelines TGA atrial switch ● Did not cover everything – Just some soundbites www.escardio.org/guidelines TGA arterial switch www.escardio.org/guidelines TGA + arterial switch: Follow-up ● All patients should be seen at least annually in a specialized GUCH centre. Frequent complications to look for: ● LV dysfunction and arrhythmias: both may be related to coronary artery problems (re-implanted ostia) ● Dilatation of the proximal part of the ascending aorta resulting in AR ● Supravalvular PS, pulmonary branch stenosis (unilaterally or bilaterally). www.escardio.org/guidelines TGA + arterial switch: Diagnostic Work-up (1) ● Echocardiography: key diagnostic technique providing LV function (global and regional), stenosis at the arterial anastomotic sites, most commonly PS, neoaortic valve regurgitation, dimension of the ascending aorta and the acute angulation of the aortic arch. The pulmonary trunk, the bifurcation and both branches should be evaluated for the presence, localisation and severity of stenoses. RV function should be judged and systolic pressures should be estimated (TR velocity). Stress echo can unmask LV dysfunction and detect provocable myocardial ischemia. ● CMR: evaluation of the aorta, pulmonary branch stenosis and flow distribution between left and right lung. ● CT: might be used for non-invasive imaging of coronary arteries, including the ostia, in case of suspicion of stenosis and as an alternative for CMR. www.escardio.org/guidelines PA branches after Lecomte R www.escardio.org/guidelines L Lecomte: pulmonary bifurcation anterior from ascending aorta www.escardio.org/guidelines Echo Doppler often adequate to diagnose presence of elevated RV pressure, often not the exact substrate www.escardio.org/guidelines CMR or CT often necessary for imaging of pulmonary trunk and branches www.escardio.org/guidelines Indications for Intervention in Transposition of the Great Arteries After Arterial Switch Operation Classa Levelb • Stenting or surgery (depending on substrate) should be performed for coronary artery stenosis causing ischaemia I C • Surgical repair of RVOTO should be performed in symptomatic patients with RV systolic pressure > 60 mmHg (TR velocity > 3.5 m/sec) I C • Surgical repair of RVOTO should be performed regardless of symptoms when RV dysfunction develops (RVP may then be lower) I C • Surgical repair should be considered in asymptomatic patients with RVOTO and systolic RVP >80 mmHg (TR velocity > 4.3 m/sec) IIa C • Aortic root surgery should be considered when the (neo-)aortic root is larger than 55 mm, providing average adult stature (for aortic valve replacement for severe AR see guidelines for AR) IIa C • Stenting or surgery (depending on substrate) should be considered for peripheral PS, regardless of symptoms, if > 50% diameter narrowing and RV systolic pressure > 50 mmHg and/or lung perfusion abnormalities IIa C a = class of recommendation. b = level of evidence. AR = aortic regurgitation; AV = atrioventricular; RV = right ventricle; RVP = right ventricular pressure; RVOTO = right ventricular outflow tract obstruction; TR = tricuspid regurgitation. www.escardio.org/guidelines Indications for Intervention in Transposition of the Great Arteries After Arterial Switch Operation Classa Levelb • Stenting or surgery (depending on substrate) should be performed for coronary artery stenosis causing ischaemia I C • Surgical repair of RVOTO should be performed in symptomatic patients with RV systolic pressure > 60 mmHg (TR velocity > 3.5 m/sec) I C • Surgical repair of RVOTO should be performed regardless of symptoms when RV dysfunction develops (RVP may then be lower) I C • Surgical repair should be considered in asymptomatic patients with RVOTO and systolic RVP >80 mmHg (TR velocity > 4.3 m/sec) IIa C • Aortic root surgery should be considered when the (neo-)aortic root is larger than 55 mm, providing average adult stature (for aortic valve replacement for severe AR see guidelines for AR) IIa C • Stenting or surgery (depending on substrate) should be considered for peripheral PS, regardless of symptoms, if > 50% diameter narrowing and RV systolic pressure > 50 mmHg and/or lung perfusion abnormalities IIa C a = class of recommendation. b = level of evidence. AR = aortic regurgitation; AV = atrioventricular; RV = right ventricle; RVP = right ventricular pressure; RVOTO = right ventricular outflow tract obstruction; TR = tricuspid regurgitation. www.escardio.org/guidelines TGA + arterial switch: Follow-up ● All patients should be seen at least annually in a specialized GUCH centre. Frequent complications to look for: ● LV dysfunction and arrhythmias: both may be related to coronary artery problems (re-implanted ostia) ● Dilatation of the proximal part of the ascending aorta resulting in AR ● Supravalvular PS, pulmonary branch stenosis (unilaterally or bilaterally). www.escardio.org/guidelines Indications for Intervention in Transposition of the Great Arteries After Arterial Switch Operation Classa Levelb • Stenting or surgery (depending on substrate) should be performed for coronary artery stenosis causing ischaemia I C • Surgical repair of RVOTO should be performed in symptomatic patients with RV systolic pressure > 60 mmHg (TR velocity > 3.5 m/sec) I C • Surgical repair of RVOTO should be performed regardless of symptoms when RV dysfunction develops (RVP may then be lower) I C • Surgical repair should be considered in asymptomatic patients with RVOTO and systolic RVP >80 mmHg (TR velocity > 4.3 m/sec) IIa C • Aortic root surgery should be considered when the (neo-)aortic root is larger than 55 mm, providing average adult stature (for aortic valve replacement for severe AR see guidelines for AR) IIa C • Stenting or surgery (depending on substrate) should be considered for peripheral PS, regardless of symptoms, if > 50% diameter narrowing and RV systolic pressure > 50 mmHg and/or lung perfusion abnormalities IIa C a = class of recommendation. b = level of evidence. AR = aortic regurgitation; AV = atrioventricular; RV = right ventricle; RVP = right ventricular pressure; RVOTO = right ventricular outflow tract obstruction; TR = tricuspid regurgitation. www.escardio.org/guidelines TGA atrial and arterial switch ● We went through the normal routine of the annual outpatient clinic visit ● Made “jumps” to the guidelines what to do when something abnormal/deteriorated was found ● And that is how I use the guidelines ● I do not know the guidelines by heart www.escardio.org/guidelines TGA atrial and arterial switch ● We went through the normal routine of the annual outpatient clinic visit ● Made “jumps” to the guidelines what to do when something abnormal/deteriorated was found ● And that is how I use the guidelines ● I do not know the guidelines by heart www.escardio.org/guidelines Thank you