* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Propionate stimulates pyruvate oxidation in the - AJP
Survey
Document related concepts
Biosynthesis wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Butyric acid wikipedia , lookup
Microbial metabolism wikipedia , lookup
Metabolic network modelling wikipedia , lookup
Basal metabolic rate wikipedia , lookup
Nuclear magnetic resonance spectroscopy of proteins wikipedia , lookup
Metabolomics wikipedia , lookup
Pharmacometabolomics wikipedia , lookup
Isotopic labeling wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Biochemistry wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Lactate dehydrogenase wikipedia , lookup
Fatty acid metabolism wikipedia , lookup
Transcript
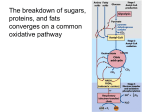
Am J Physiol Heart Circ Physiol 307: H1134 –H1141, 2014. First published August 22, 2014; doi:10.1152/ajpheart.00407.2014. Innovative Methodology Propionate stimulates pyruvate oxidation in the presence of acetate Colin Purmal,1 Blanka Kucejova,2 A. Dean Sherry,2,3,6 Shawn C. Burgess,2,4 Craig. R. Malloy,2,3,5,7 and Matthew E. Merritt2,6 1 School of Medicine, University of Texas Southwestern Medical Center, Dallas, Texas; 2Advanced Imaging Research Center, University of Texas Southwestern Medical Center, Dallas, Texas; 3Department of Radiology, University of Texas Southwestern Medical Center, Dallas, Texas; 4Department of Pharmacology, University of Texas Southwestern Medical Center, Dallas, Texas; 5Department of Internal Medicine, University of Texas Southwestern Medical Center, Dallas, Texas; 6 Department of Chemistry, University of Texas at Dallas, Richardson, Texas; and 7Veterans Affairs North Texas Healthcare System, Dallas, Texas Submitted 12 June 2014; accepted in final form 21 August 2014 substrate selection; pyruvate; glucose; propionate; hyperpolarization; isotopomer analysis myocardial ischemia inhibits production of hyperpolarized (HP) [13C]bicarbonate derived from HP [1-13C]pyruvate (8, 9, 36). Because the appearance of HP [13C]bicarbonate is due to metabolism in functioning mitochondria, the appearance of HP [1-13C]bicarbonate may provide evidence of viable myocardium (3, 18, 25, 26, 35, 36). Consequently, it is important to understand the factors controlling appearance of HP [1-13C]bicarbonate from HP [1-13C]pyruvate. Under simple conditions in isolated hearts, HP [113 C]bicarbonate is generated from HP [1-13C]pyruvate only by flux through pyruvate dehydrogenase (PDH) (25). Flux through this pathway is inhibited by acetyl-CoA and other end END STAGE CARDIOMYOPATHY OR Address for reprint requests and other correspondence: M. E. Merritt, Advanced Imaging Research Center, Univ. of Texas Southwestern Medical Center, Dallas, Texas 75390 (e-mail: [email protected]). H1134 products, and further regulated by phosphorylation-dephosphorylation of the PDH complex. Because metabolism of fatty acids generates high concentrations of acetyl-CoA, the appearance of HP 13CO2 and HP [13C]bicarbonate is markedly inhibited by fats even in normal hearts (25, 27). Consequently, in addition to disease processes, physiological fluctuations in the concentrations of fatty acids also influence the appearance of HP [13C]bicarbonate. An intervention that stimulates flux through PDH in the presence of fatty acids could remove the effects of substrate competition in detecting oxidation of HP [1-13C]pyruvate. One such approach is co-administration of glucose, insulin, and potassium (16). This mixture has multiple effects on plasma glucose, plasma free fatty acids, and myocardial membrane potential, so any effects on bicarbonate appearance probably reflect a complex interaction between substrate concentrations and direct effects on PDH (4). Propionate, a physiological short chain fatty acid, also influences PDH flux. The interaction of propionate with pyruvate metabolism in the heart has been extensively studied using 14C tracers. Fatty acids of even carbon chain length markedly inhibit appearance of 14CO2 from [1-14C]pyruvate (14, 32). When compared with acetate, propionate increased the rate of 14 CO2 production from [1-14C]pyruvate under steady state conditions (14), suggesting that propionate may be an alternative to glucose, insulin, and potassium for stimulating PDH flux. However, the relevance of these studies for HP 13C NMR observations is unclear, for two reasons. First, the radiotracer studies examined the influence of individual fatty acids such as acetate or propionate on pyruvate metabolism. The effect of propionate on pyruvate metabolism in the presence of even chain fatty acids has not been studied extensively, and it is not known whether the stimulatory effects of propionate on PDH flux overcome the inhibitory effects of fatty acids. Second, the magnitude of the increase in 14CO2 appearance from [114 C]pyruvate induced by propionate was only about threefold compared with acetate (14). Because these data were acquired under steady state conditions, it is not clear if HP pyruvate would detect similar effects, since the window for observing the HP species is ⬃2 min. The purpose of this study was to determine whether the reduced appearance of HP [13C]bicarbonate from HP [113 C]pyruvate caused by acetate can be overcome by propionate-induced stimulation of PDH flux. Hearts from C57/bl6 mice were perfused to steady state in the presence of glucose and saturating concentrations of acetate. Acetate is the most avidly metabolized fatty acid, since it freely diffuses into the mitochondria, bypassing carnitine palmitoyl transferase-I. In 0363-6135/14 Copyright © 2014 the American Physiological Society http://www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.5 on May 4, 2017 Purmal C, Kucejova B, Sherry AD, Burgess SC, Malloy CR, Merritt ME. Propionate stimulates pyruvate oxidation in the presence of acetate. Am J Physiol Heart Circ Physiol 307: H1134 –H1141, 2014. First published August 22, 2014; doi:10.1152/ajpheart.00407.2014.—Flux through pyruvate dehydrogenase (PDH) in the heart may be reduced by various forms of injury to the myocardium, or by oxidation of alternative substrates in normal heart tissue. It is important to distinguish these two mechanisms because imaging of flux through PDH based on the appearance of hyperpolarized (HP) [13C]bicarbonate derived from HP [1-13C]pyruvate has been proposed as a method for identifying viable myocardium. The efficacy of propionate for increasing PDH flux in the setting of PDH inhibition by an alternative substrate was studied using isotopomer analysis paired with exams using HP [1-13C]pyruvate. Hearts from C57/bl6 mice were supplied with acetate (2 mM) and glucose (8.25 mM). 13C NMR spectra were acquired in a cryogenically cooled probe at 14.1 Tesla. After addition of hyperpolarized [1-13C]pyruvate, 13C NMR signals from lactate, alanine, malate, and aspartate were easily detected, in addition to small signals from bicarbonate and CO2. The addition of propionate (2 mM) increased appearance of HP [13C]bicarbonate ⬎30-fold without change in O2 consumption. Isotopomer analysis of extracts from the freeze-clamped hearts indicated that acetate was the preferred substrate for energy production, glucose contribution to energy production was minimal, and anaplerosis was stimulated in the presence of propionate. Under conditions where production of acetyl-CoA is dominated by the availability of an alternative substrate, acetate, propionate markedly stimulated PDH flux as detected by the appearance of hyperpolarized [13C]bicarbonate from metabolism of hyperpolarized [1-13C]pyruvate. Innovative Methodology H1135 PROPIONATE STIMULATES PYRUVATE OXIDATION addition, it is not -oxidized, but can immediately be used to synthesize acetyl-CoA. As such, the acetate perfused heart represents a model where flux through PDH is expected to be maximally inhibited. In addition, to our knowledge, this is the first application of a combination of hyperpolarization and cryoprobe technology to study the perfused mouse heart. MATERIALS AND METHODS RESULTS Effects of propionate on oxidation of acetate and glucose. The presence of propionate in the perfusion medium did not alter O2 consumption (44 ⫾ 21 mol·gdw⫺1·min⫺1 in group 1 vs. 48 ⫾ 15 mol·gdw⫺1·min⫺1 in group 2). Flux through citrate synthase was calculated from O2 consumption (17). Table 1 summarizes these values for the two different conditions. Table 1 also reports that anaplerotic flux (relative to TCA cycle flux) was significantly elevated in the presence of propionate as expected. There was no significant change in phosphorylation at serine 293 of PDH as measured in Western blots in hearts supplied with propionate (data not shown). The effects of unlabeled propionate on conventional 13C NMR spectra from extracts of hearts supplied with [1,213 C2]acetate plus unlabeled glucose are illustrated in Fig. 1. In addition to the dominant glutamate resonances, the spectra also show resonances of malate, citrate, and aspartate, with malate and citrate being higher when propionate is supplied (Fig. 1B). The insets in Fig. 1 show the glutamate C2, C3, and C4 resonances. Isotopomers of glutamate that have three or more carbons labeled consecutively produce doublets of doublets, marked Q for quartet when the J-couplings are resolved, or T for triplet when they are degenerate as occurs in carbon 3 of glutamate. Glutamate labeled in positions 3, 4, and 5 is derived from the condensation of [U-13C]acetyl-CoA with [2-13C]oxaloacetate and its subsequent forward flux to ␣-ketoglutarate and exchange into the glutamate pool. The relative areas of the multiplets in each glutamate resonance provide a direct read-out of substrate preferences and anaplerosis under steady-state isotopic conditions (17, 19 –21). Table 1. Metabolic fluxes calculated from a combination of 13 C-isotopomer analysis of 13C NMR spectra of perfused mouse heart extracts plus O2 consumption data Without propionate With propionate O2 Consumption, mol·gdw⫺1·min⫺1 Citrate Synthase Flux, mol·gdw⫺1·min⫺1 Y 44 ⫾ 22 48 ⫾ 15 21 ⫾ 9 22 ⫾ 7 0.12 ⫾ 0.01 0.25 ⫾ 0.02 Anaplerosis (Ys) is expressed as a fraction of citrate synthase flux (TCA cycle turnover). Anaplerosis, y, is significantly different (P ⬍ 0.001). AJP-Heart Circ Physiol • doi:10.1152/ajpheart.00407.2014 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.5 on May 4, 2017 Materials. [1-13C]pyruvic acid and [2-13C]pyruvic acid were purchased from Sigma-Aldrich Isotec (Miamisburg, OH) or Cambridge Isotope Laboratories (Tewksbury, MA) and used without further purification. The various 13C isotopomers of sodium acetate, glucose, and propionate were purchased and used as supplied from Cambridge Isotopes (Andover, MA). Trityl-OXO63 free radical was purchased from Oxford Instruments Molecular Biotools (Oxford, UK). Protocol. The protocol was approved by the Institutional Animal Care and Use Committee of the University of Texas Southwestern Medical Center. Female mice, 14 –16 wk in age, were purchased from Charles River and housed four to a cage. All animals were fed ad libitum. A single ketamine (43 mg/kg) and xylazine (8.7 mg/kg) intraperitoneal injection was used for general anesthesia. Depth of anesthesia was assessed by observation of the respiratory rate, paw pinch reflex, and palpebral reflex of the animal. Under general anesthesia, the hearts were rapidly excised and arrested in ice-cold perfusion medium. Langendorff perfusions were performed according to Stowe et al. (39) including measurements of developed pressure, coronary flow, heart rate, and O2 consumption. Briefly, the aorta of the excised heart was cannulated and perfused in nonrecirculating mode at a constant perfusion pressure of 80 cm H2O. A KrebsHenseleit buffered medium containing 25 mM NaHCO3, 118 mM NaCl, 4.7 mM KCl, 1.2 mM MgSO4, 1.2 mM KH2PO4, and 0.5 mM ethylene diamine tetraacetic acid was bubbled continuously with a 95/5 mixture of O2/CO2 gas to maintain a pH of 7.4. The perfusing medium was maintained at 37°C using a water bath. Two sets of perfusion conditions were used in the studies of HP [1-13C]pyruvate. Hearts in group 1 were supplied with 8.25 mM glucose and 2 mM [U-13C]acetate with subsequent addition of HP pyruvate (n ⫽ 5). Hearts in group 2 were perfused with identical concentrations of glucose and acetate plus 2 mM propionate (n ⫽ 5). Additional experiments were performed with unlabeled acetate, [213 C]pyruvate, [U-13C]glucose, or [U-13C]propionate, depending on the experiment. Hearts were freeze-clamped and extracted for 1H and 13 C NMR spectroscopy. Dynamic nuclear polarization. All NMR experiments were carried out at 14.1 T using a Bruker Avance 3 HD console (Bruker BioSpin, Billerica, MA) equipped with a 10 mm 13C cryoprobe operating at a temperature of 15° K. The temperature of the sample was held at 37°C throughout the experiment. Samples of pyruvic acid (5 l) were polarized essentially as described previously (1). The samples were dissolved and injected by catheter immediately above the heart (25). 13 C NMR spectra were acquired using 15° excitation pulses with a 2-s repetition time. Acquisition was terminated upon completion of 96 single-pulse acquisitions, the perfusion rig was removed from the magnet, and the heart was immediately freeze-clamped for tissue extraction. The time delay between initial injection of pyruvate to freeze-clamping, including all NMR data acquisition from the perfused heart, was ⬃200 s. Peak areas from the DNP experiments were measured by integration. NMR and isotopomer analysis of tissue extracts. Freeze-clamped hearts were extracted using perchloric acid (27). 13C NMR of the extracts was acquired as previously (24). The resulting multiplets derived from the utilization of the isotopically labeled substrates were fit using a mixed Gaussian/Lorentzian lineshape in the ACD NMR Processor Software (Advanced Chemistry Development, Toronto, Canada). Proton spectra were fitted with the Chenomx software package to obtain lactate and alanine concentrations (Chenomx, Al- berta, Canada). Relative peak areas of the resonances adjacent to 12C versus the 13C satellites were measured in the 1H NMR spectrum to obtain a final concentration of the metabolites as well as the 13C enrichments. The 13C NMR spectra of glutamate were analyzed according to Sherry et al. (37). Fractions of acetyl-CoA derived from [U-13C]acetate were also analyzed using the C5D/C5S ratio. Western blot analysis. Tissue lysates were prepared in RIPA buffer (Cell Signaling, Danvers, MA) containing CompleteTM protease inhibitors (Roche, Indianapolis, IN). Anti-PDH ␣1 subunit antibodies were obtained from Cell Signaling, and anti-phospho-PDH ␣1 subunit (S293) were obtained from Millipore (Billerica, MA). Statistical analysis. Significant differences were evaluated using GraphPad Prism (La Jolla, CA) using multiple t-tests with a significance level of P ⬍ 0.05. For the HP data, each resonance was analyzed individually without the assumption of a consistent standard deviation. The False Discovery Rate approach with a rate of 5% was used to suppress random correlations between variables. For comparisons of concentrations and fractional enrichments, simple t-tests were used without further correction. For all graphs, error bars reflect the standard deviation of the data. Innovative Methodology H1136 PROPIONATE STIMULATES PYRUVATE OXIDATION The dominant signal from [3,4,5-13C3]glutamate C4 (the doublet of doublet, or quartet) indicates qualitatively that a high fraction of acetyl-CoA was derived from exogenous [1,213 C2]acetate (Fig. 1A). The [3,4,5-13C]glutamate isotopomer is decreased in the presence of propionate as evidenced by the increase in the relative fraction of the D45 doublet versus the C4Q fraction (Fig. 1B). This isotopomer is produced by the condensation of [U-13C]acetyl-CoA with oxaloacetate that is not labeled in the C2 position. Under these conditions, unenriched propionate increases the fraction of OAA that is not labeled. The relevant pathways are summarized in Fig. 2. The isotopomers of ␣-ketoglutarate derived from [1,2-13C2]oxaloacetate or [3,4-13C2]oxaloacetate are shown in the dotted box. With the addition of unlabeled propionate and consequently an increase in the fraction of unlabeled oxaloacetate, the fraction of ␣-ketoglutarate that is [3,4,5C]␣-ketoglutarate will decrease (Fig. 1B). Because the heart was clamped less than 3.5 min after addition of [1-13C]pyruvate, the 13C NMR spectrum is dominated by isotopomers generated before addition of pyruvate. Conventional isotopomer analysis was used to measure anaplerosis and the fraction of acetyl-CoA derived from [1,213 C2]acetate (20). After the introduction of [1-13C]pyruvate, metabolism through PDH could briefly provide a new source of unenriched acetyl-CoA. In hearts supplied with acetate and glucose, 98% of acetyl-CoA was derived from [1,213 C2]acetate. Among the hearts supplied with acetate, glucose, and propionate, the same amount of acetyl-CoA was derived from [1,2-13C2]acetate, as measured by the fraction of C5D/ C5S. The singlet was assumed to be derived from natural 13 AJP-Heart Circ Physiol • doi:10.1152/ajpheart.00407.2014 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.5 on May 4, 2017 Fig. 1. 1H-Decoupled 13C NMR spectra of tissue extracts. Thermally polarized 13C NMR spectra of tissue extracts of hearts perfused to steady state with unlabeled glucose and [U-13C]acetate and exposed briefly to hyperpolarized (HP)-[1-13C]pyruvate are illustrated over the chemical shift range of ⬃25 to 57 ppm. In the absence of propionate (A), both acetyl-CoA and oxaloacetate must be highly enriched as measured by the high fractional contribution of the quartets (in C2 and C4) or triplets (in C3) of glutamate. Hearts supplied with propionate (B) showed an increase in the doublet, D45, relative to the quartet, indicating lower 13C enrichment in oxaloacetate. Propionate also induced an increase in citrate and malate abundance. C: concentrations (conc.) of lactate and alanine as measured by quantitative 1H NMR of the heart extracts. Addition of propionate to the perfusion medium resulted in a decrease in the alanine concentration in the heart. D: fractional enrichments of the C1 position of lactate and alanine as measured by proton NMR of the methyl protons and 3 bond j-couplings to the C1 position. Alanine is more enriched than lactate in both perfusions conditions, although the difference is accentuated in the presence of propionate. Innovative Methodology PROPIONATE STIMULATES PYRUVATE OXIDATION H1137 Fig. 2. Metabolic model for hearts supplied with [1,2-13C2]acetate. Ball-andstick figures of acetate, acetyl-CoA, pyruvate, oxaloacetate (OAA), ␣-ketoglutarate, and glucose (2, 2, 3, 4, 5, or 6 carbons, respectively) are shown. 13C is indicated by filled circles, and each carbon position is numbered from left to right. The isotopomers presented assume 1 turn of the TCA cycle has been completed with labeled acetate present, hence the symmetric enrichment of the OAA pool. Under these conditions, neglecting natural abundance 13C, the acetyl-CoA pool is either [1,2-13C2]acetyl-CoA or unlabeled. Consequently, the C4 signal of glutamate is either a doublet due to labeling in carbons 4 and 5, or a doublet of doublets due to labeling in positions 3 and 4 and 5. In the presence of propionate, the fraction of unenriched OAA is increased and, consequently, the fraction of ␣-ketoglutarate labeled simultaneously in carbons 3 and 4 and 5 decreases. The dashed rectangle indicates ␣-ketoglutarate derived from 13C-labeled OAA. PDH, pyruvate dehydrogenase. abundance 13C. Separate bench experiments using [U-13C]glucose and [2-13C]acetate confirmed that acetate was the overwhelming source of acetyl-CoA; less than 3% of acetyl-CoA was derived from glucose either in the presence or absence of propionate. These experiments confirmed that exogenous glucose was not metabolized in the TCA cycle via either PDH or pyruvate carboxylase, consistent with earlier studies of isolated rat hearts (20). 1 H NMR spectra of these same samples indicated that propionate resulted in a significant decrease in total tissue alanine and a trend toward lower lactate (Fig. 1, C and D). The lactate-to-alanine ratio was not significantly different. Similarly, the fractional 13C enrichment in the lactate was not significantly different in the presence of propionate, but the enrichment in [1-13C]alanine was significantly higher in propionate-perfused hearts. Labeling in the C1 position can only result from the exogenous, hyperpolarized [1-13C]pyruvate. Fig. 3. Metabolism of [1-13C]pyruvate. Flux through PDH leads to production of 13CO2, but there are 3 other possible sources in a single turn of the TCA cycle. After carboxylation by PC, the 13C label can become symmetrized by exchange between malate and fumarate (faded circle). Subsequent flux through the malic enzyme produces 13CO2 but the fractional enrichment has a maximal value of 50%. Alternatively, after carboxylation, a forward turn of the TCA cycle could eliminate a 13CO2 at the step of isocitrate dehydrogenase (shaded circle). This pathway could have a maximal enrichment equal to the exogenous pyruvate. Finally, after symmetrization at fumarate, a forward turn of the TCA cycle could produce a 13CO2 at ␣-ketoglutarate dehydrogenase. AJP-Heart Circ Physiol • doi:10.1152/ajpheart.00407.2014 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.5 on May 4, 2017 Both [1-13C] and [2-13C]lactate and alanine have similar 2JCH and 3JCH values to the methyl protons, but inspection of the 13C spectra allow the couplings to be assigned exclusively to labeling at the C1 position. This provides direct evidence showing that exogenous [1-13C]pyruvate exchanges more fully with tissue pools of alanine than it does with tissue lactate, as reported previously (31). Effect of propionate on metabolism of hyperpolarized [1-13C]pyruvate. Mouse hearts were studied in the 10 mm 13C optimized cryoprobe. All four possible biochemical fates of [1-13C]pyruvate, illustrated in Fig. 3, could be directly detected in the functioning mouse heart. Metabolism of pyruvate to lactate, alanine, or bicarbonate could be monitored in real time, and the fourth possibility - carboxylation via pyruvate carboxylase - could be detected in summed spectra. Spectra obtained by summing the 25 individual spectra with the highest signal following injection with hyperpolarized [113 C]pyruvate are shown in Fig. 4. Downstream products resulting from carboxylation of pyruvate (malate and aspartate) as well as the expected signals of [1-13C]lactate, [1- Innovative Methodology H1138 PROPIONATE STIMULATES PYRUVATE OXIDATION DISCUSSION C]alanine, and H13CO3⫺ were observed. In hearts supplied with propionate in the perfusion media, there was a marked increase in the signal intensity of HP [13C]bicarbonate and a small decrease in signal intensities of aspartate and malate. The increase in the malate signal in conventional 13C NMR spectra shows that the pool size of malate is increased by propionate (Fig. 1), a well-known effect (40), yet the HP malate signal was reduced. Representative time-intensity curves for [1-13C]lactate, [113 C]alanine, H13CO3⫺, and 13CO2 are shown in Fig. 5. The most striking differences were in the magnitude of the [13C]bicarbonate and 13CO2 signals in the presence of propionate. An alternative approach to display data such as this is to normalize the total signal intensity derived from pyruvate and its metabolites and graph the hyperpolarized “activities” of each, i.e., taking the area under the curve for the time evolution of each metabolite (Fig. 6) (11). The integrated [13C]bicarbonate intensity was ⬃37 times higher in the presence of propionate (P ⬍ 0.01). Other significant differences were found for alanine (P ⬍ 0.01), aspartate-C1 (P ⬍ 0.01), aspartate-C4 (P ⬍ 0.01), and for 13CO2 (P ⬍ 0.01), which is in fast equilibrium with bicarbonate. No significant differences were observed for signals associated with lactate or either C1- or C4-labeled malate. 13 Fig. 5. Effect of propionate on dynamic appearance of lactate, alanine, bicarbonate, and CO2. Representative kinetic curves for appearance of [113 C]lactate, [1-13C]alanine, 13CO2, and [13C]bicarbonate in the absence (B) and presence (A) of propionate after addition of HP [1-13C]pyruvate are shown. Propionate perfusion causes not only an increase in [1-13C]pyruvate decarboxylation but also a decrease and a change in the time to maximum signal for the [1-13C]alanine. AJP-Heart Circ Physiol • doi:10.1152/ajpheart.00407.2014 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.5 on May 4, 2017 Fig. 4. 13C spectra of the functioning mouse heart. Spectra were obtained following the addition of HP [1-13C]pyruvate to perfused hearts without propionate and with propionate. The [13C]bicarbonate ([13C]bicarb) signal was increased in the presence of propionate, but there was little effect on the intensity of the malate-C4 resonances. If the increase in [13C]bicarbonate signal is derived from malic enzyme or ␣-ketoglutarate dehydrogenase flux, an increase in the malate resonance intensity would be expected. Pyr-hyd, pyruvate hydrate. This experiment was designed to assess the effects of propionate on pyruvate metabolism in the presence of a high concentration of a fatty acid. Acetate was chosen because there is no question that it is the preferred substrate for oxidation by heart tissue when present in millimolar concentrations, and it therefore serves as a model for maximal substrate-induced suppression of PDH flux. These studies confirm that in the presence of high concentrations of acetate and glucose, the overwhelming majority of acetyl-CoA production in hearts was derived from acetate (20). The current results further demonstrate that oxidation of HP [1-13C]pyruvate, even in a high concentration administered as a bolus, is nearly eliminated in the presence of acetate (27). Oxygen consumption was not changed by propionate (Table 1), yet HP [13C]bicarbonate increased ⬎30-fold (Fig. 5). A much smaller increase in HP [13C]bicarbonate was noted under conditions where malate was co-administered in vivo (34). Administration of dichloroacetate also activates PDH flux, but side effects of the drug prevent its long-term usage medically (2, 12, 23). This model is another condition where bicarbonate production from HP [1-13C]pyruvate is completely dissociated from myocardial oxygen consumption (25). Earlier studies examined the effects of acetate or propionate, studied independently, on [1-14C]pyruvate metabolism and the rate of appearance of 14CO2 compared with the absence of either fatty acid. These studies suggest approximately threefold increase in 13CO2 could be expected in the presence of propionate. The current observation of ⬎30-fold increase likely occurred for two reasons. First, more physiological concentration of pyruvate, ⬃0.1 mM, was used previously (14). The current design delivered a much higher concentration of pyruvate, 2 mM. Although this is Innovative Methodology PROPIONATE STIMULATES PYRUVATE OXIDATION higher than the physiological concentration of pyruvate in normal plasma, millimolar concentrations of pyruvate are common and probably necessary for in vivo HP experiments (33). A second factor in the large effect of propionate on [13C]bicarbonate production is the control condition. In the study design, advantage was taken of the known effects of acetate on pyruvate oxidation and the anticipated marked suppression on the appearance of HP [13C]bicarbonate and 13CO2 in control hearts. The present results demonstrate that the stimulatory effects of propionate on PDH flux override the inhibitory effects of acetate on appearance of HP [13C]bicarbonate from HP [1-13C]pyruvate. Acetate is not subject to transport by carnitine palmitoyl transferase-I, nor is it -oxidized. As such, it is the most avidly metabolized substrate available to the heart. The overwhelming preference of the heart for acetate underscores just how powerful the effects of propionate are on substrate selection. The activity of the PDH is regulated by reversible phosphorylations of multiple subunits and by inhibition by its end products, acetyl CoA and NADH. The phosphorylation state of PDH, in turn, is controlled by competing activity of pyruvate dehydrogenase kinase and pyruvate dehydrogenase phosphatase. In the absence of acetate, propionate caused almost complete dephosphorylation of PDH in rat hearts (14). Under the current experimental conditions, with a high concentration of both acetate and propionate in group 2, the Western blot analysis did not demonstrate a measurable change in the phosphorylation state at serine 293 (data not shown). The effect of propionate on PDH flux could be due to trapping of CoA as propionyl-CoA rather than acetyl-CoA, with a consequent loss of end-product inhibition at PDH (41). Alternatively, propionate could exert control through secondary phosphorylation sites on PDH (10). Exact determination of the mechanism of PDH activation in this condition is the subject of ongoing research. Pyruvate may also undergo carboxylation in the heart (20) as illustrated in Fig. 3, which allows additional decarboxylation reactions that could serve as sources of HP [13C]bicarbonate (30, 38). As illustrated in Fig. 4, HP [1-13C]malate, HP [113 C]aspartate, and HP [4-13C]aspartate were all detected. Because the T1 of 13C limits the duration of these studies, conversion of [1-13C]pyruvate ¡ [1-13C]oxaloacetate ¡ [113 C]malate ¡ [1-13C]fumarate ⫹ [4-13C]fumarate ¡ [413 C]malate ¡ [4-13C]aspartate must have occurred within 10 s of addition of pyruvate. The presence of HP [4-13C]aspartate demonstrates that [4-13C]oxaloacetate must also be present. Phosphoenolpyruvate carboxykinase does not exist in the heart, but the malic enzyme can serve to cycle malate back to pyruvate with release of CO2 (40). Introduction of propionate produced highly significant increases in both HP 13CO2 and [13C]bicarbonate. The HP signals of aspartate-C1 and -C4 were both lower in the presence of propionate, but the HP signals of malate-C1 and -C4 only trended lower without reaching statistical significance. Given the stable or declining pool sizes of malate and aspartate (Fig. 1), this result indicates that the amount of [1-13C]pyruvate entering the citric acid cycle via pyruvate carboxylation is reduced when propionate is present. By extension, the increase in anaplerosis shown by 13C isotopomer analysis can be largely ascribed to entry of propionate into the TCA cycle via propionyl-CoA carboxylase. Consequently, we conclude that production of 13CO2 via carboxylation of HP [1-13C]pyruvate followed re-arrangement and eventual decarboxylation contributes little, probably insignificant amounts, to overall appearance of HP[13C]bicarbonate under these conditions. Furthermore, if the malic enzyme was highly active, pyruvate formed by decarboxylation of malate would be labeled in multiple positions concurrently due to the high fractional enrichment of the oxaloacetate pool achieved by perfusion with [1,2-13C2]acetate. Although pyruvate is not detectable in the extracts, the lactate and alanine pools did not demonstrate any labeling beyond that caused by the injection of HP [1-13C]pyruvate. Finally, in the presence of HP [213 C]pyruvate, 13C labeling observed in citrate and glutamate could only arise from decarboxylation of HP [2-13C]pyruvate by the PDH (data not shown). Together, these spectra indicate that the only significant source of [13C]bicarbonate is the product of pyruvate decarboxylation in PDH. These observations are consistent with previous findings in the rat heart (14, 20, 38) and further demonstrate the stimulatory effects of propionate on flux of exogenous pyruvate through PDH even in the presence of inhibition by short chain fatty acid metabolism. In addition to its effects on pyruvate oxidation, exposure to propionate also stimulates anaplerosis in the heart (5, 14). In this case, propionate itself is the anaplerotic substrate. After activation to propionyl-CoA and carboxylation to form methylmalonyl-CoA, it undergoes rearrangement to an intermediate AJP-Heart Circ Physiol • doi:10.1152/ajpheart.00407.2014 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.5 on May 4, 2017 Fig. 6. Effect of propionate on hyperpolarized signal of metabolic products. The integrated areas under the curve expressed as the fraction of total intensity of pyruvate and its metabolites are shown for 8 signals. The 4-carbon intermediates are ⬃4 – 8 times less intense than the alanine and lactate signals. Lack of measurable differences in intensity of the malate (mal)-C4 resonance strongly suggests the [13C]bicarbonate (bicarb) production is not related to increased malic enzyme flux. *P ⬍ 0.05. Asp, aspartate. H1139 Innovative Methodology H1140 PROPIONATE STIMULATES PYRUVATE OXIDATION GRANTS This research was funded through National Heart, Lung, and Blood Institute Grants R21 EB016197, P41 EB015908, R37 HL34557, and R01 DK058398. Dr. Merritt acknowledges salary support from CPRIT RP-101243. S. C. Burgess acknowledges support from the Robert A. Welch foundation. DISCLOSURES No conflicts of interest, financial or otherwise, are declared by the author(s). AUTHOR CONTRIBUTIONS Author contributions: C.P., B.K., and M.E.M. performed experiments; C.P., A.D.S., S.C.B., C.R.M., and M.E.M. edited and revised manuscript; A.D.S., S.C.B., C.R.M., and M.E.M. interpreted results of experiments; C.R.M. and M.E.M. analyzed data; M.E.M. conception and design of research; M.E.M. prepared figures; M.E.M. drafted manuscript; M.E.M. approved final version of manuscript. REFERENCES 1. Ardenkjaer-Larsen JH, Fridlund B, Gram A, Hansson G, Hansson L, Lerche MH, Servin R, Thaning M, Golman K. Increase in signal-tonoise ratio of ⬎ 10,000 times in liquid-state NMR. Proc Natl Acad Sci USA 100: 10158 –10163, 2003. 2. Atherton HJ, Dodd MS, Heather LC, Schroeder MA, Griffin JL, Radda GK, Clarke K, Tyler DJ. Role of pyruvate dehydrogenase inhibition in the development of hypertrophy in the hyperthyroid rat heart: a combined magnetic resonance imaging and hyperpolarized magnetic resonance spectroscopy study. Circulation 123: 2552–2561, 2011. 3. Atherton HJ, Schroeder MA, Dodd MS, Heather LC, Carter EE, Cochlin LE, Nagel S, Sibson NR, Radda GK, Clarke K, Tyler DJ. Validation of the in vivo assessment of pyruvate dehydrogenase activity using hyperpolarised 13C MRS. NMR Biomed 24: 201–208, 2011. 4. Bothe W, Olschewski M, Beyersdorf F, Doenst T. Glucose-insulinpotassium in cardiac surgery: a meta-analysis. Ann Thorac Surg 78: 1650 –1657, 2004. 5. Brunengraber H, Roe CR. Anaplerotic molecules: current and future. J Inherit Metab Dis 29: 327–331, 2006. 6. Ferrari R, Merli E, Cicchitelli G, Mele D, Fucili A, Ceconi C. Therapeutic effects of l-carnitine and propionyl-l-carnitine on cardiovascular diseases: a review. Ann N Y Acad Sci 1033: 79 –91, 2004. 7. Garland PB, Newsholme EA, Randle PJ. Regulation of glucose uptake by muscle. Effects of fatty acids and ketone bodies, and of alloxandiabetes and starvation, on pyruvate metabolism and on lactate-pyruvate and L-glycerol 3-phosphate-dihydroxyacetone phosphate concentration ratios in rat heart and rat diaphragm muscles. Biochem J 93: 665–678, 1964. 8. Golman K, Petersson JS. Metabolic imaging and other applications of hyperpolarized 13C. Academic Radiology 13: 932–942, 2006. 9. Golman K, Petersson JS, Magnusson P, Johansson E, Åkeson P, Chai C, Hansson G, Månsson S. Cardiac metabolism measured noninvasively by hyperpolarized 13C MRI. Magn Reson Med 59: 1005–1013, 2008. 10. Holness MJ, Sugden MC. Regulation of pyruvate dehydrogenase complex activity by reversible phosphorylation. Biochem Soc Trans 31: 1143–1151, 2003. 11. Hu S, Chen AP, Zierhut ML, Bok R, Yen YF, Schroeder MA, Hurd RE, Nelson SJ, Kurhanewicz J, Vigneron DB. In vivo carbon-13 dynamic MRS and MRSI of normal and fasted rat liver with hyperpolarized 13C-pyruvate. Mol Imaging Biol 11: 399 –407, 2009. 12. Hu S, Yoshihara HAI, Bok R, Zhou J, Zhu M, Kurhanewicz J, Vigneron DB. Use of hyperpolarized [1-13C]pyruvate and [2-13C]pyruvate to probe the effects of the anticancer agent dichloroacetate on mitochondrial metabolism in vivo in the normal rat. Magn Reson Imaging 30: 1367–1372, 2012. 13. Lango R, Smolenski RT, Rogowski J, Siebert J, Wujtewicz M, Slominska EM, Lysiak-Szydlowska W, Yacoub MH. Propionyl-L-carnitine improves hemodynamics and metabolic markers of cardiac perfusion during coronary surgery in diabetic patients. Cardiovasc Drugs Ther 19: 267–275, 2005. 14. Latipaa PM, Peuhkurinen KJ, Hiltunen JK, Hassinen IE. Regulation of pyruvate dehydrogenase during infusion of fatty acids of varying chain lengths in the perfused rat heart. J Mol Cell Cardiol 17: 1161–1171, 1985. 15. Lau AZ, Chen AP, Ghugre NR, Ramanan V, Lam WW, Connelly KA, Wright GA, Cunningham CH. Rapid multislice imaging of hyperpolarized 13C pyruvate and bicarbonate in the heart. Magn Reson Med 64: 1323–1331, 2010. 16. Lauritzen MH, Laustsen C, Butt SA, Magnusson P, Søgaard LV, Ardenkjær-Larsen JH, Åkeson P. Enhancing the [13C]bicarbonate signal in cardiac hyperpolarized [1-13C]pyruvate MRS studies by infusion of glucose, insulin and potassium. NMR Biomed 26: 1496 –1500, 2013. 17. Malloy CR, Jones JG, Jeffrey FM, Jessen ME, Sherry AD. Contribution of various substrates to total citric acid cycle flux and ]anaplerosis as determined by 13C isotopomer analysis and O2 consumption in the heart. MAGMA 4: 35–46, 1996. AJP-Heart Circ Physiol • doi:10.1152/ajpheart.00407.2014 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.5 on May 4, 2017 of the citric acid cycle, succinyl-CoA (20, 22, 29, 38). In the current study, anaplerosis was stimulated by propionate, as reported previously (Table 1). The role of cardiac anaplerosis in health and disease is only partially understood, but it remains a potential target for therapy. Propionate itself has been suggested as a compound useful for replenishing depleted pools of TCA cycle intermediates (5), and propionyl-L-carnitine has beneficial effects in animal models and human subjects (6, 13). There are currently no methods for detecting the effects of propionate on the human heart. Because multislice cardiac imaging of HP [13C]bicarbonate is feasible in the pig heart (15) and administration of HP [1-13C]pyruvate is safe in human patients (28), extension of these results to human cardiac imaging is feasible. The cytosol of the heart is considered by many as a homogeneous space where exogenous pyruvate presumably has free access to high-activity cytosolic enzymes such as lactate dehydrogenase and alanine aminotransferase. Nevertheless, earlier studies (7, 30, 31) found that 14C labeling in alanine and lactate derived from exogenous [1-14C]pyruvate was not consistent with a single pool of pyruvate freely exchanging with alanine and lactate. The current results confirm earlier studies with 14C that alanine enrichment is consistently significantly higher than lactate (Fig. 1D), and this discrepancy is enhanced by propionate. Furthermore, as elucidated in the [U-13C]glucose experiment (data not shown), considerable lactate was produced in these hearts via glycolysis, yet little of that carbon source was oxidized in the TCA cycle (0 –3%). The appearance of [13C]bicarbonate generated from [1-13C]pyruvate is not proportional to glucose oxidation. Glucose and pyruvate, under certain conditions, can have very different metabolic fates in the myocardium. Future experiments that vary the perfusion conditions will test whether this conclusion can be further generalized in the perfused heart. In general, the HP 13 C signal from any metabolite is proportional to (fractional enrichment)·(polarization)·(concentration). Because we have shown here that exogenous [1-13C]pyruvate does not equilibrate with total lactate in heart tissue, the HP [1-13C]lactate signal must also underestimate total tissue lactate in these experiments. Meticulous optimization of pulse sequence design has allowed imaging of HP [13C]bicarbonate and [113 C]lactate, but results here suggest that lactate derived from exchange with exogenous HP pyruvate might underestimate the size of the lactate pool (36). Furthermore, the high alanine enrichment does not parallel lactate enrichment. Oftentimes, the lactate-to-alanine ratio is taken as a surrogate marker of the redox state of the cytosol. In this perfusion condition at least, assessing the redox state by making a ratio of the lactate to alanine signal intensity would lead to fallacious results. This study stresses the importance of gaining a complete understanding of the effect of the multiple compartments available to the heart in vivo. Innovative Methodology PROPIONATE STIMULATES PYRUVATE OXIDATION 30. Peuhkurinen KJ, Hassinen IE. Pyruvate carboxylation as an anaplerotic mechanism in the isolated perfused rat heart. Biochem J 202: 67–76, 1982. 31. Peuhkurinen KJ, Hiltunen JK, Hassinen IE. Metabolic compartmentation of pyruvate in the isolated perfused rat heart. Biochem J 210: 193–198, 1983. 32. Randle PJ, Newsholme EA, Garland PB. Regulation of glucose uptake by muscle. Effects of fatty acids, ketone bodies and pyruvate, and of alloxan-diabetes and starvation, on the uptake and metabolic fate of glucose in rat heart and diaphragm muscles. Biochem J 93: 652–665, 1964. 33. Schroeder MA, Atherton HJ, Cochlin LE, Clarke K, Radda GK, Tyler DJ. The effect of hyperpolarized tracer concentration on myocardial uptake and metabolism. Magn Reson Med 61: 1007–1014, 2009. 34. Schroeder MA, Atherton HJ, Heather LC, Griffin JL, Clarke K, Radda GK, Tyler DJ. Determining the in vivo regulation of cardiac pyruvate dehydrogenase based on label flux from hyperpolarised [113 C]pyruvate. NMR Biomed 24: 980 –987, 2011. 35. Schroeder MA, Cochlin LE, Heather LC, Clarke K, Radda GK, Tyler DJ. In vivo assessment of pyruvate dehydrogenase flux in the heart using hyperpolarized carbon-13 magnetic resonance. Proc Natl Acad Sci USA 105: 12051–12056, 2008. 36. Schroeder MA, Lau AZ, Chen AP, Gu Y, Nagendran J, Barry J, Hu X, Dyck JRB, Tyler DJ, Clarke K, Connelly KA, Wright GA, Cunningham CH. Hyperpolarized 13C magnetic resonance reveals early- and late-onset changes to in vivo pyruvate metabolism in the failing heart. Eur J Heart Fail 15: 130 –140, 2013. 37. Sherry AD, Jeffrey FM, Malloy CR. Analytical solutions for 13C isotopomer analysis of complex metabolic conditions: substrate oxidation, multiple pyruvate cycles, and gluconeogenesis. Metab Eng 6: 12–24, 2004. 38. Sherry AD, Malloy CR, Roby RE, Rajagopal A, Jeffrey FM. Propionate metabolism in the rat heart by 13C nmr spectroscopy. Biochem J 254: 593–598, 1988. 39. Stowe KA, Burgess SC, Merritt M, Sherry AD, Malloy CR. Storage and oxidation of long-chain fatty acids in the C57/BL6 mouse heart as measured by NMR spectroscopy. FEBS Lett 580: 4282–4287, 2006. 40. Sundqvist KE, Heikkila J, Hassinen IE, Hiltunen JK. Role of NADP⫹ (corrected)-linked malic enzymes as regulators of the pool size of tricarboxylic acid-cycle intermediates in the perfused rat heart. Biochem J 243: 853–857, 1987. 41. Sundqvist KE, Peuhkurinen KJ, Kalervo Hiltunen J, Hassinen IE. Effect of acetate and octanoate on tricarboxylic acid cycle metabolite disposal during propionate oxidation in the perfused rat heart. Biochim Biophys Acta 801: 429 –436, 1984. AJP-Heart Circ Physiol • doi:10.1152/ajpheart.00407.2014 • www.ajpheart.org Downloaded from http://ajpheart.physiology.org/ by 10.220.33.5 on May 4, 2017 18. Malloy CR, Merritt ME, Dean Sherry A. Could 13C MRI assist clinical decision-making for patients with heart disease? NMR Biomed 24: 973– 979, 2011. 19. Malloy CR, Sherry AD, Jeffrey FM. Analysis of tricarboxylic acid cycle of the heart using 13C isotope isomers. Am J Physiol Heart Circ Physiol 259: H987–H995, 1990. 20. Malloy CR, Sherry AD, Jeffrey FMH. Evaluation of carbon flux and substrate selection through alternate pathways involving the citric acid cycle of the heart by 13C NMR spectroscopy. J Biol Chem 263: 6964 – 6971, 1988. 21. Malloy CR, Thompson JR, Jeffrey FM, Sherry AD. Contribution of exogenous substrates to acetyl coenzyme A: measurement by 13C NMR under non-steady-state conditions. Biochemistry 29: 6756 –6761, 1990. 22. Martini WZ, Stanley WC, Huang H, Rosiers CD, Hoppel CL, Brunengraber H. Quantitative assessment of anaplerosis from propionate in pig heart in vivo. Am J Physiol Endocrinol Metab 284: E351–E356, 2003. 23. Mayer D, Yen YF, Josan S, Park JM, Pfefferbaum A, Hurd RE, Spielman DM. Application of hyperpolarized [1-13C]lactate for the in vivo investigation of cardiac metabolism. NMR Biomed 25: 1119 –1124, 2012. 24. Merritt ME, Harrison C, Sherry AD, Malloy CR, Burgess SC. Flux through hepatic pyruvate carboxylase and phosphoenolpyruvate carboxykinase detected by hyperpolarized 13C magnetic resonance. Proc Natl Acad Sci USA 108: 19084 –19089, 2011. 25. Merritt ME, Harrison C, Storey C, Jeffrey FM, Sherry AD, Malloy CR. Hyperpolarized 13C allows a direct measure of flux through a single enzyme-catalyzed step by NMR. Proc Natl Acad Sci USA 104: 19773– 19777, 2007. 26. Merritt ME, Harrison C, Storey CJ, Sherry AD, Malloy CR. Inhibition of carbohydrate oxidation during the first minute of reperfusion after brief ischemia: NMR detection of hyperpolarized 13CO2 and H13CO3⫺. Magn Reson Med 60: 1029 –1036, 2008. 27. Moreno KX, Sabelhaus SM, Merritt ME, Sherry AD, Malloy CR. Competition of pyruvate with physiological substrates for oxidation by the heart: implications for studies with hyperpolarized [1-13C]pyruvate. Am J Physiol Heart Circ Physiol 298: H1556 –H1564, 2010. 28. Nelson SJ, Kurhanewicz J, Vigneron DB, Larson PE, Harzstark AL, Ferrone M, van Criekinge M, Chang JW, Bok R, Park I, Reed G, Carvajal L, Small EJ, Munster P, Weinberg VK, Ardenkjaer-Larsen JH, Chen AP, Hurd RE, Odegardstuen LI, Robb FJ, Tropp J, Murray JA. Metabolic imaging of patients with prostate cancer using hyperpolarized [1-13C]pyruvate. Sci Transl Med 5: 198ra108, 2013. 29. Nuutinen EM, Peuhkurinen KJ, Pietilainen EP, Hiltunen JK, Hassinen IE. Elimination and replenishment of tricarboxylic acid-cycle intermediates in myocardium. Biochem J 194: 867–875, 1981. H1141