* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download How the Heart Pumps Blood
Survey
Document related concepts
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Jatene procedure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Electrocardiography wikipedia , lookup
Atrial septal defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
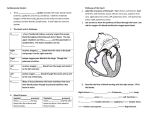
How the Heart Pumps Blood Michael Brinton The heart is a muscular organ in the circulatory system of all mammals. In humans, it is about the size of a fist and is located in the center of the thoracic cavity, directly behind the sternum (breastbone). The muscles of the heart form four chambers. Coordinated contractions of the heart muscles pump blood through these four chambers and out to the pulmonary and systemic circulation. As with all muscles, electrical impulses control the contractions of the heart. This document will first examine the anatomy of the human heart and the path of blood flow through the heart. It will then move on to the electrical pathways controlling the contractions of the heart muscles. Finally, these electrical pathways will be related to an electrocardiogram, a diagnostic tool used in medicine to observe the electrical events of the heart. Anatomy and Blood Flow The heart is separated down the center by the septum, forming the left and right sides. Each side has an upper chamber, the atrium, and a lower chamber, the ventricle. Each chamber has a oneway valve at its exit. These valves control the blood flow by inhibiting any backward flow. The atria function to collect blood that is returning to the heart from the body (right atrium) or from the lungs (left atrium) and to push that blood into the ventricles. The ventricles function to pump blood out to other parts of the body. The walls of the left ventricle are thicker than the walls of the right ventricle, because the left ventricle must pump blood to the whole body, whereas the right ventricle only pumps blood to the pulmonary circulation (in the lungs). Figure 1 illustrates the anatomy of the heart, with arrows showing blood flow. Figure 1. Anatomy and Blood Flow of the Heart (Source: texasheartinstitute.org) 1 of 4 Deoxygenized blood returns to the heart through a series of veins, dumping into the right atrium via the vena cava. The right atrium pushes blood to the right ventricle. The right ventricle then pumps blood to the lungs through the pulmonary artery. In the lungs, red blood cells refill with oxygen, while at the same time carbon dioxide and other waste products leave the blood. As blood leaves the lungs, it travels back to the heart through the pulmonary vein, dumping into the left atrium. The left atrium pushes blood into the left ventricle, which then pumps the blood out to the rest of the body. Blood delivers oxygen and picks up waste products in the tissues of the body. Then it travels back to the heart, and the cycle starts again. The Electrical System Although the heart is made mostly of muscle tissue, it also contains tissues that direct electrical impulses to coordinate the contractions of the heart. These impulses originate in the sinoatrial (SA) node, a specialized group of cells located at the back of the right atrium. From the SA node, impulses travel around both atria, causing them to contract. Impulses are then paused at the atrioventricular (AV) node. As can be guessed by the name, this node is located between the atria and the ventricles. The AV node pauses the electrical impulse for one to two tenths of a second to allow the blood time to pass from the atria to the ventricles. The impulse then travels down the septum (between the ventricles) and then back up through the outer walls of the ventricle via the Purkinje fibers. This way, the ventricle contracts from the bottom up, allowing as much blood as possible to exit into the arteries. Figure 2 below illustrates the electrical pathways in the heart. Figure 2. Electrical Pathways of the Heart (Source: heartrhythmclinic.com) 2 of 4 The Clinical Picture The electrical pathways above can be viewed in a clinical setting using a device called and electrocardiogram (EKG or ECG). An EKG consists of several wires which are connected to the patient’s chest, generally with a sticky, electricity-conducting patches. The number and placement of these wires varies greatly, depending on what the clinician wishes to see. However, all placements view the heart in the same way, by measuring electric potential between different wires. A “normal” four-lead EKG reading is shown in Figure 3, with the waveforms labeled. This readout can be very helpful to diagnose problems with the heart, but first one must know what a normal reading signifies. Figure 3. Normal EKG (Source: a-fib.com) The first upward wave of the EKG, the P wave, represents the contraction of the atria (the upper chambers). The flat segment before the next wave, the PR segment, shows the time that the electrical impulse is paused at the AV node. The next set of waves, the QRS complex, represents the contraction of the ventricles (the lower chambers). There is another pause, and then the T wave is formed when the ventricles electrically reset to be ready for the next impulse. Note that the atria also reset, but this happens at the same time that the ventricles contract, and thus it is covered by the much more intense electrical activity of the ventricles. While a printout of an EKG can be useful to a trained medical provider in an ambulance, a hospital, or a doctor’s office, the EKG is also used in some other devices without needing to be interpreted by a medical provider. For example, an AED (Automated External Defibrillator) is a 3 of 4 tool that can be used by medical providers and laymen alike to deliver shocks during CPR for a person in cardiac arrest. However, those who will benefit from a shock in cardiac arrest still have electrical activity in their heart. It just is not normal or coordinated. The AED actually contains a computer that analyzes the electric potential between the pads (which were placed on the patient’s chest by the rescuer) in a similar way as a regular EKG machine. If the computer identifies an abnormal, but “shockable” rhythm, the rescuer can administer that shock without ever having to see or interpret the rhythm. This way, life-saving treatment can be delivered by those without the knowledge to properly interpret an EKG. Conclusion This document has provided the basics of how the heart pumps blood and how the events of the cardiac cycle can be recorded using EKG technology. One could get lost in the intricacies of EKG interpretation, cardiac dysrhythmias, and hemodynamics. As such, those topics require a much deeper study than what this document can provide. However, the anatomy and basic function of the heart, contained above, can serve as foundational knowledge, should one wish to continue their study of the heart beyond the information contained in this document. 4 of 4