* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download cAlnOfficial Journalofthe c.AmericanHeart cjlssociation
Survey
Document related concepts
Discovery and development of beta-blockers wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Discovery and development of antiandrogens wikipedia , lookup
NMDA receptor wikipedia , lookup
Toxicodynamics wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Chlorpromazine wikipedia , lookup
5-HT2C receptor agonist wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Norepinephrine wikipedia , lookup
Nicotinic agonist wikipedia , lookup
Cannabinoid receptor antagonist wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Transcript
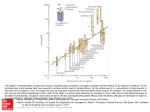
VOL 72 AUGUST NO 2 1985 cAln Official Journalof the c.American Heart cjlssociation, Inc. FEATURES Dopamine receptors: applications in clinical cardiology LEON I. GOLDBERG, M.D., PH.D., AND SOL I. RAJFER, M.D. Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017 THE DISCOVERY of the renal vasodilating action of dopamine more than 20 years ago led to extensive research that demonstrated other unusual actions of this endogenous catecholamine. 1-' Investigators using traditional pharmacologic models and modern biochemical techniques have documented the existence of distinct dopamine receptor subtypes that mediate these responses. Appreciation of the structure-activity requirements of these receptors has led to the synthesis of drugs that may have a profound influence on the management of the patient with heart disease. Taxonomy of dopamine receptors. Rigid criteria must be met to prove the existence of a new receptor by classical pharmacologic methods, including construction of a unique potency series of agonists and demonstration of specific antagonism.4 5 In contrast, biochemical techniques are applied to tissue homogenates, and different standards are frequently used to classify receptors.P 7 After many years of research, two distinct dopamine receptor subtypes, DA, and DA2, were identified conclusively by classical criteria in physiologic preparations.5 DA receptors are located postsynaptically and subserve vasodilation in renal, mesenteric, coronary, and cerebral blood vessels (figure 1). DA,-induced vasodilation can be observed in other vascular beds, but the response is less prominent, probably because of the lower density of dopamine receptors. The molecular structure required for activation of DA, receptors is very strict.4 Currently, all active compounds have two hydroxyl groups in positions analogous to the 3- and 4positions on the benzene ring of the dopamine molecule, and a limited distance exists between the hydroxyl groups and the amino group. From the Committee on Clinical Pharmacology, Departments of Pharmacological and Physiological Sciences and Medicine, Section of Cardiology, The University of Chicago. Address for correspondence: Leon I. Goldberg, M.D., Ph.D., Committee on Clinical Pharmacology, The University of Chicago, 947 E. 58th St., Chicago, IL 60637. Supported in part by National Institutes of Health grant GM-22220 and HL-00872. Dr. Rajfer is the recipient of a National Institutes of Health Clinical Investigator award HL-00872. Vol. 72, No. 2, August 1985 DA2 receptors are located on postganglionic sympathetic nerves and autonomic ganglia, and when these receptors are activated, norepinephrine release from sympathetic nerve endings is inhibited (figure 1). DA2 receptors are also located in the emetic center of the area postrema and in the anterior lobe of the pituitary gland. Activation of these receptors results in emesis and inhibition of prolactin release, respectively. The structural requirements for DA2 agonists are much less restrictive than those for DA, agonists. Indeed, the structures of DA2 agonists are so diverse that it is difficult to determine molecular requirements for activity.4 Major advances have been made in the synthesis of dopamine agonists, and compounds are now available with spectra of receptor activity different from that of dopamine. Of significance, the benzazepine derivative, fenoldopam, proved to be a selective DA, agonist.' Selective DA2 agonists have been available for several years. Examples include piribedil and ergot derivatives, which are used for the treatment of Parkinson's disease, and LY 17155, an ergoline derivative.4 The first dopamine antagonists used to classify dopamine receptors were the neuroleptics, haloperidol and chlorpromazine.2 Although these agents made it possible to distinguish dopamine receptors from other receptors, the dose range in which they are specific antagonists for dopamine receptors is very narrow. Furthermore, these antagonists cannot be used to differentiate dopamine receptor subtypes. Recently, selective antagonists that discriminate between DA, and DA2receptors have been synthesized. An example of a selective DA, antagonist is the benzazepine, SCH 23390, which is chemically related to fenoldopam.9 Domperidone, a butyrophenone derivative related to haloperidol, is an example of a selective DA2 antagonist. Availability of selective dopamine agonists and antagonists has aided in the determination of whether dopamine subtypes classified on the basis of cardionew 10 245 GOLDBERG and RAJFER PREJUNCTIONAL SYMPATHETIC NERVE TERMINAL POSTJUNCTIONAL VASCULAR EFFECTOR CELL DA (EXOGENOUS) Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017 FIGURE 1. Location of DA, receptors, a1- and a2-adrenoceptors on postganglionic vascular effector cells, and DA2 receptors and a2-adrenoceptors on the prejunctional sympathetic nerve terminal. When dopamine is administered, activation of DA1 receptors causes vasodilation and activation of DA2 receptors causes inhibition ( - ) of norepinephrine (NE) release from storage granules. A larger dose of dopamine activates a1- and a2-adrenoceptors on the postjunctional effector cells to cause vasoconstriction and on a2-adrenoceptors on the prejunctional sympathetic terminal to inhibit release of norepinephrine. Norepinephrine released from the prejunctional sympathetic terminal also acts on a1- and a2-adrenoceptors. vascular responses are similar to those receptors identified in brain and endocrine tissues by biochemical techniques. In one biochemical method, dopamine receptors are subdivided according to the effects of agonists on the enzyme, adenylate cyclase. Activation of D, receptors results in stimulation of adenylate cyclase; activation of D2 receptors either results in inhibition of adenylate cyclase or has no effect on that enzyme.6 In a second biochemical method, dopamine receptors are subdivided according to the pattern of displacement of radioactive ligands by dopamine agonists or antagonists.7 The radioligand binding assays have been extremely controversial because of the many inconsistencies in the dopamine receptor subtypes "identified" by these assays.6' It appears that many of the early ligand-binding investigations yielded increased numbers of receptor subtypes because the ligands used were not selective or because strict criteria required to characterize receptors were not fulfilled.4 6 Recent studies conducted with more selective ligands have identified only two dopamine subtypes similar to D andD9.6 Comparison of the DA, and DA, classification with the revised D, and D2 classification suggests that the same receptors are identified by the two methods. However, a few significant discrepancies in the potency series of agonists and antagonists remain, and further studies are needed to determine the reasons for these differences.' Pharmacologic actions of dopamine. The activation of adrenoceptors and dopamine receptors by dopamine is the basis for its diverse clinical applications.2' 3 Because of extreme individual variations in the infusion rates of dopamine required to activate the different 246 receptors, patients must be monitored carefully to achieve the desired hemodynamic profile. DA, and DA, receptors are activated at the lowest infusion rates, resulting in a decline in peripheral vascular resistance and modest increments in renal blood flow, urine volume, and sodium excretion. At these low rates of infusion (usually 0.5 to 2 gg/kg/min) dopamine may initiate a diuresis in patients refractory to furosemide. 1 1 As the infusion rate is increased (usually above 2 ,ug/kg/min), f,-adrenoceptors are activated and cardiac output begins to increase, typically with little change in heart rate. This is the hemodynamic response sought in the treatment of heart failure. The infusion rate may then be gradually increased until recruitment of a°- and a2-adrenoceptors occurs as manifested by an increase in vascular resistance or until excessive 3,-adrenoceptor activity leads to tachycardia or ventricular arrhythmias. Higher infusion rates can be used if the undesirable vasoconstriction is eliminated by simultaneous administration of a vasodilating agent.3 With such concurrent administration, caution must be exercised to avoid excessive reduction in arterial pressure. Indeed, unmasking of the vasodilating effects of dopamine in the presence of phenoxybenzamine was the first demonstration of its potential use in the treatment of hypertension.'2 A different hemodynamic pattern may be achieved by conjoint administration of dopamine and dobutamine. This combination provides greater ,/3-adrenoceptor activity, maintenance of the beneficial renal effects of dopamine, and avoidance of a-adrenoceptor-mediated vasoconstriction seen with high doses of dopamine.3 Orally active pro-drugs. Poor oral bioavailability of CIRCULATION PERSPECTIVE Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017 dopamine stimulated the development and investigation of orally active pro-drugs with dopamine activity. Two oral pro-drugs, levodopa and ibopamine, have been studied in the treatment of congestive heart failure. After oral administration of the biochemical precursor of dopamine, levodopa, dopamine is generated by the action of aromatic amino acid decarboxylase in the liver and other tissues. Investigations in patients with Parkinson's disease demonstrated that oral administration of levodopa in doses of 1 to 1.5 g produces cardiac and natriuretic effects approximating the responses observed with intravenous infusions of dopamine at rates of 2 to 4 1tg/kg/min.2 On this basis, levodopa was studied recently in patients with severe congestive heart failure. After ingestion of levodopa (1.5 to 2.0 g), significant improvement in cardiac performance was observed. Furthermore, the beneficial hemodynamic effects were sustained during long-term therapy for 3 or more months. The lack of tolerance to levodopa is in sharp contrast to the findings of previous studies conducted with pirbuterol, which was ineffective after sustained therapy. 13 This difference could be explained by the partial agonist activity of pirbuterol and the full agonist activity of dopamine. Down-regulation of 8,-adrenoceptors with continuous therapy should decrease activity of partial agonists to a much greater extent than that of full agonists. 14 No serious adverse effects were observed in this initial study with levodopa. However, levodopa can produce nausea and vomiting unless the dose is gradually increased. Accordingly, the dose was increased from 250 mg qid to 1.5 to 2.0 g qid over a 5 to 7 day period. In addition 50 mg of pyridoxine was administered daily, since previous studies have shown that this vitamin is required for the decarboxylation of levodopa. In addition to the trial of levodopa in congestive heart failure, the pro-drug has also been used to help wean patients from long-term intravenous infusion of dopamine.3 Ibopamine is the diisobutyric ester of N-methyl dopamine (epinine). When ibopamine is absorbed, it is acted upon by esterases in the plasma to release Nmethyl dopamine (epinine). Epinine resembles dopamine pharmacologically. Several studies in Europe and the United States have shown that oral ingestion of 100 to 300 mg of ibopamine produces beneficial hemodynamic effects in patients with congestive heart failure.'5'16 Ibopamine has recently been approved for clinical use in Italy. New dopamine agonists. The possibility that several Vol. 72, No. 2, August 1985 receptors may be responsible for the beneficial hemodynamic effects of dopamine, levodopa, and ibopamine is supported by the results of studies which demonstrate that dopamine agonists lacking ,B,-adrenergic activity elicit beneficial responses in patients with severe congestive heart failure. Propylbutyl dopamine (an agonist of DA1 and DA2 receptors) was administered intravenously to patients with severe congestive heart failure."' Cardiac index increased while pulmonary capillary wedge pressure and systemic vascular resistance were significantly reduced. No change in heart rate was observed. Mean arterial pressure decreased in a dose-related manner, declining 20 mm Hg when infused at a rate of 20 gg/kg/min. Vasodilation caused by activation of DA1 and DA2 receptors by propylbutyl dopamine appeared to be responsible for the hemodynamic responses observed. Renal hemodynamics were not measured in these patients, but studies in normal subjects and hypertensive patients demonstrated that propylbutyl dopamine produces pronounced increments in renal blood flow.12 Hemodynamic improvement was also observed in patients with severe congestive heart failure when the ergot derivative, bromocriptine, was administered orally in a dose of 2.5 mg.'8 Bromocriptine has been shown to act as a DA2 agonist in peripheral nerves but also may decrease sympathetic activity via a central nervous system mechanism. Heart rate, mean arterial pressure, left ventricular end-diastolic pressure, and mean right atrial pressure decreased while stroke volume increased. Cardiac index did not increase, possibly because of the decrease in heart rate. A decline in plasma norepinephrine concentrations accompanied these hemodynamic changes. Hemodynamic actions of the selective DA, agonist, fenoldopam, were evaluated in a pilot study in patients with congestive heart failure. 19 Oral administration of fenoldopam (200 mg) resulted in a decline in pulmonary capillary wedge pressure and systemic vascular resistance and an increase in cardiac index. Heart rate did not change. The renal effects of fenoldopam were not studied in these patients, but increments in renal blood flow and sodium excretion were observed when the drug was administered to normal subjects and hypertensive patients.'2 The natriuresis induced by DA, agonists is unusual for vasodilating agents. The availability of orally effective dopamine congeners has greatly expanded the potential clinical indications for these agonists. Of particular significance, fenoldopam, propylbutyl dopamine, and bromocriptine have been found to be effective in lowering blood pressure in hypertensive patients.'2 Another possible 247 GOLDBERG and RAJFER Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017 new use for dopamine agonists is in the treatment of arrhythmias. A study in the anesthetized dog has shown that bromocriptine is effective in the prevention of digitalis-induced arrhythmias.20 The mechanism responsible for this antiarrhythmic effect appears to be decreased sympathetic activity. In summary, the results of studies with orally effective dopamine agonists have suggested new approaches to the management of patients with cardiovascular disease. The safety and efficacy of these agents during long-term therapy remains to be established. Athough the results of preliminary investigations are encouraging, only a limited number of patients have been observed for prolonged periods. Regardless of the results of these studies, future research will undoubtedly lead to the development of new dopamine agonists with greater bioavailability, different spectra of receptor activity, and fewer adverse effects. A new and exciting era of dopamine research has begun. References 1.McDonald RH Jr, Goldberg LI, McNay JL, Tuttle EP Jr: Effects of dopamine in man: augmentation of sodium excretion, glomerular filtration rate, and renal plasma flow. J Clin Invest 43: 1116, 1964 2. Goldberg LI: Cardiovascular and renal actions of dopamine: potential clinical applications. Pharmacol Rev 24: 1, 1972 3. Goldberg LI, Hsieh YY, Resnekov L: Newer catecholamines for treatment of heart failure and shock: an update on dopamine and a first look at dobutamine. Prog Cardiovasc Dis 4: 327, 1977 4. Goldberg LI, Kohli JD: Differentiation of dopamine receptors in the periphery. In Kaiser C, Kebabian 1W, editors: American Chemical Society Symposium Series No. 224. Dopamine receptors. Washington, DC, 1983, American Chemical Society, pp 101-113 248 5. Goldberg Ll, Kohli JD: Peripheral pre- and post-synaptic dopamine receptors: are they different from dopamine receptors in the central nervous system? Commun Psychopharmacol 3: 447, 1979 6. Stoof JC, Kebabian SW: Two dopamine receptors: biochemistry, physiology, and pharmacology. Life Sci 35: 2281, 1984 7. Seeman P: Brain dopamine receptors. Pharmacol Rev 32: 230, 1981 8. Hahn RA, Wardell JR Jr, Sarua HM, Ridley PT: Characterization of the peripheral and central effects of SK&F 82526, a novel dopamine receptor agonist. J Pharmacol Exp Ther 223: 305, 1982 9. Goldberg LI, Glock D, Kohli JD, Barnett A: Separation of peripheral dopamine receptors by a selective DA1 antagonist, SCH 23390. Hypertension 6 (suppl 1): 1-25, 1984 10. Kohli JD, Glock D, Goldberg Ll: Selective DA2 versus DA1 antagonist activity of domperidone in the periphery. Eur J Pharmacol 89: 137, 1983 11. Henderson IS, Beattie TJ, Kennedy AC: Dopamine hydrochloride in oliguric states. Lancet 2: 827, 1980 12. Goldberg Ll: Dopamine receptors and hypertension: physiological and pharmacological implications. Am J Med 77: 37, 1984 13. Rajfer SI, Anton AH, Rossen J, Goldberg LI: Beneficial hemodynamic effects of oral levodopa in heart failure: relationship to the generation of dopamine. N EngI J Med 310: 1357, 1984 14. Kenakin TP, Ferris RM: Effects of in vivo beta-adrenoceptor down-regulation on cardiac responses to prenalterol and pirbuterol. J Cardiovasc Pharmacol 5: 90, 1983 15. Dei Cas L, Bolognesi R, Cucchini F, Fappani A, Riva S, Visioli 0: Hemodynamic effects of ibopamine in patients with idiopathic congestive cardiomyopathy. J Cardiovasc Pharmacol 5: 249, 1983 16. Ren JH, Unverferth DV, Leier CV: The dopamine congener, ibopamine, in congestive heart failure. I Cardiovasc Pharmacol 6: 748, 1984 17. Fennell WH, Taylor AA, Young JB, Brandon TA, Ginos JZ, Goldberg LI, Mitchell JR: Propylbutyldopamine: hemodynamic effects in conscious dogs, normal human volunteers, and patients with heart failure. Circulation 67: 829, 1983 18. Francis GS, Parks R, Cohn JN: The effects of bromocriptine in patients with congestive heart failure. Am Heart J 106: 100, 1983 19. Leon CA, Suarez JM, Aranoff RD, Murray MJ, Pratt CM, Young JB: Fenoldopam: efficacy of a new orally active dopamine analog in heart failure. Circulation 70 (suppl II): 11-307, 1984 20. Kao A, Kriett JM, Tobler HG, Detloff BLS, Pritzker MR, Benson DW Jr, Benditt DG: Bromocriptine treatment of digitalis-induced ventricular tachyarrhythmias: studies in a canine model. J Am Coil Cardiol 4: 1188, 1984 CIRCULATION Dopamine receptors: applications in clinical cardiology. L I Goldberg and S I Rajfer Downloaded from http://circ.ahajournals.org/ by guest on June 18, 2017 Circulation. 1985;72:245-248 doi: 10.1161/01.CIR.72.2.245 Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 1985 American Heart Association, Inc. All rights reserved. Print ISSN: 0009-7322. Online ISSN: 1524-4539 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circ.ahajournals.org/content/72/2/245.citation Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation is online at: http://circ.ahajournals.org//subscriptions/