* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Reminder: Review the Histology lectures* about Cells and Organs of
Survey
Document related concepts
Monoclonal antibody wikipedia , lookup
Inflammation wikipedia , lookup
Lymphopoiesis wikipedia , lookup
Molecular mimicry wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Complement system wikipedia , lookup
Immune system wikipedia , lookup
Polyclonal B cell response wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Adaptive immune system wikipedia , lookup
Cancer immunotherapy wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Transcript
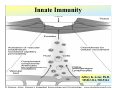
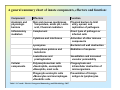
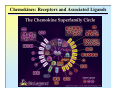
Reminder: Review the Histology lectures* about Cells and Organs of the Immune System Review posted review on Blackboard. Also found at: http://www.uth.tmc.edu/pathology/medic/immunology/Immuno/ReviewInfoImmuneOrgans.2012.pdf *Info from Histology lectures is testable material Innate Immunity Jeffrey K. Actor, Ph.D. MSB 2.214, 500-5344 Lecture Objectives: • Introduce innate immune defense mechanisms. • Review cell types involved in innate immune responses, and their role in inflammation. • Define ADCC, Chemokines, and Pattern-Recognition Receptors. What Constitutes Innate Immunity? • The innate immune system: • present from birth • present prior to onset of infection • constitutes non-specific mechanisms of defense • Innate components recognize classes of molecules frequently encountered on invading pathogens • allows defensive measures until specific immune response is generated 4 Categories of Innate Immunity • Anatomic. • Physiologic. • Phagocytic and Endocytic. • Inflammatory. Anatomic Barrier • Skin • thin outer epidermis, thicker underlying dermis • impedes entry of foreign material • Sebaceous glands • produce sebum, comprised of lactic acid and fatty acids • reduces skin pH, inhibits organism growth. • Mucous membranes • covered by cilia • traps organisms, propels them out of the body. Physiologic Barrier • Includes temperature, low pH, chemical mediators. • • Organisms can not multiply in elevated temperature. Lysozymes degrade bacterial membranes. • Complement components in serum attack bacterial membranes. Low stomach pH discourages organism growth. Lactoferrin inhibits bacterial growth. • • Anatomic/Physiologic (Secreted Substances) Defensins: natural anti-microbial peptides Phagocytic and Endocytic Barrier • Blood monocytes, tissue macrophages and neutrophils phagocytose and kill microorganisms via complex digestion mechanisms. • Bacteria ingested into phagocytic vesicles. • Phagosomes fuse with lysosomes. • Lysosomal enzymes digest captured organisms. • Interferons ( and ) inhibit viral expansion. Inflammatory Barrier Rubor et Tumor cum Calore et Dolore 2000 years ago Celcus defined 4 cardinal signs of acute inflammation Inflammation through injury Inflammation through infection Rubor et Tumor cum Calore et Dolore • Redness (rubor) – Inflamed tissue appears red due to dilatation of small blood vessels within the damaged area. • Swelling (tumor) – Extravascular fluid accumulation as part of the fluid exudate (edema). – Physical mass of inflammatory cell migration into area. • Heat (calor) – Vascular dilation and increased blood flow (hyperaemia). – Chemical mediators lead to systemic fever. • Pain (dolor) – Stretching/distortion of tissues by inflammatory edema, pus pressure. – Via chemical mediators (bradykinin, prostaglandins, serotonin). Beneficial Effects of Fluid Exudate (Vascular Permeability) • Dilution of toxins. • Entry of antibodies. – Lysis of microorganisms (complement). – Assisted phagocytosis (opsonisation). – Neutralization of toxins. • Fibrin formation. – Impede movement/trap micro-organisms; facilitate phagocytosis. • Delivery of nutrients and oxygen. • Stimulation of immune response. – Drainage of fluid exudate/antigens into lymphatics. Harmful Effects of Fluid Exudate • Release of lysosomal enzymes by inflammatory cells. • Digestion/destruction of normal tissues by enzymes. • Swelling. – Obstruction of ducts, lymphatics. – Leads to ischaemic damage (vascular constriction by pressure). Chemical Mediators of Inflammation Kinin -> Fibrinolytic Clotting Complement Critical Molecules in Injury • Many of the clotting factors and kininogens lead to production of vasoactive peptides. Some activate phospholipases…. Phospholipases then feed into the Arachidonic Acid Pathway…. Arachidonic Acid Metabolites: Inflammatory Role Cells of the Innate Immune Response Neutrophils • The neutrophil's main role is in inflammation. – First cells to arrive at the site of inflammation. • Neutrophils are attracted to tissue by chemotactic factors. – Complement proteins and clotting proteins. • actively phagocytic in tissue • kill microorganisms by oxygen dependent or independent pathways. Neutrophils (cont’d) • Chemoattractants (eg. Interleukin-8 [IL-8], complement C5a) trigger adhesion and subsequent diapedesis. • Neutrophil interaction with antibody and complement allow increased phagocytosis of invading organisms. • Activation of neutrophils leads to: – respiratory burst – production of reactive oxygen and nitrogen intermediates – release of primary and secondary granules • proteases, phospholipases, elastases and collagenases. • Pus, a yellowish white opaque creamy matter produced by the process of suppuration consists of innumerable neutrophils (some dead and dying) and tissue debris. Bactericidal Agents in Phagocytes Neutrophil Transendothelial Migration • Reversible binding, activation, adherence, and movement between endothelial cells. Erythrocyte Sedimentation Rate (ESR = sed rate) • During infection, elevated ESR – Increased protein – Interaction with charge on RBCs – Causes “stacking” • Rouleaux formation – Stacking of RBC in vascular beds gives neutrophils extra time to interact with adhesion molecules Loss of any factor that impairs neutrophil function would make individual susceptible to bacterial infection! •See case study #27: Leukocyte Adhesion Deficiency • Missing expression of integrin LFA-1, beta chain. Mononuclear Cells and Macrophages • Monocytes and macrophages ingest and destroy bacteria • Multiple factors prepare particulate for engulfment and targeting for destruction – opsonins comprised of complement components. • Phagocytes bear several different receptors that recognize microbial components – induce phagocytosis – Pattern Recognition Receptors Phagosome:Lysosome fusion • enzymatic degredation • NO mediated events • low pH See Case #26: Chronic Granulomatous Disease Macrophages • After activation, these cells secrete interferons, lysosyme and other immunoregulators of immune response. Released molecules (cytokines) work on a local and on a systemic level. What are Cytokines???? Cytokines from macrophages link Innate immunity (nonspecific) with Adaptive immunity (specific). Cytokines • Small molecular weight glycopeptides • Made by a variety of cells • Each cytokine has multiple activities [plieotropic], dependent upon cell target, concentration, and presence of other cytokines • Cytokines can facilitate innate immune function and assist in activation of inflammatory responses • Often referred to as Interleukins Selected Cytokines and their functions. IL-8 Oh so simple….. Remember: I mentioned that each cytokine has multiple activities [plieotropic] and is dependent upon cell target, concentration, and presence of other cytokines. Actions can get complicated very quickly…. NK Cells and “ADCC” • Kill infected or tumor “self” cells in the absence of antigen-specific receptors. • Therefore, NK cell killing is considered nonspecific. • NK cells can function to actively lyse target cells in a process know as: Antibody-Dependent, Cell Mediated Cytotoxicity (ADCC). ADCC • Mediate ADCC using receptors for the constant portion of an antibody. – CD16 • Recognize antibody coated target – release lytic enzymes that damage target cell membranes . • They also cause death by inducing apoptosis in the target. Antibody-Dependent, Cell Mediated Cytotoxicity: target cells coated with antibody are destroyed by specialized killer cells (Type II hypersensitivity). Chemokines • Small polypeptides acting via G-protein coupled receptors. • All chemokines related in amino acid sequence. • Grouped into two distinct categories: – CC chemokines have two adjacent cysteine residues (hence the name "CC"). – CXC chemokines have an amino acid between two cysteine residues. • Chemokine receptors are integral membrane proteins having seven membrane-spanning helices. Properties of Selected Chemokines Chemokine Major Cell Source Cell Type Attracted CCL2 (MCP-1) Monocytes and Macrophages, Fibroblasts Chemoattractant for monocytes CCL3 (MIP-1) Monocytes, T cells, Fibrobalsts, Mast cells Chemoattractant for neutrophilic granulocytes CCL5 (Rantes) T cells, Endothelium Chemoattractant for Eosinophils and Basophils, Monocytes and Dendritic cells, and T cells CCL11 (Eotaxin) Monocytes and Macrophages, Endothelium and Epithelium Chemoattractant for Eosinophils CXCL8 (IL-8) Monocytes and Macrophages, Fibroblasts, Endothelial cells Chemoattractant for Neutrophils See syllabus appendix for more complete list of chemokines, their source, and their biological function. Complement Complement • Direct Cytolysis of foreign organisms • An enyzmatic cascade: forms a pore channel in the lipid bilayer, causing osmotic lysis of the cell. • Opsonization of foreign organisms • Coating organism enhances phagocytosis and targeted destruction. • Directed leukocyte migration • Proteolytic degradation of complement components results in leukocyte chemotaxis. The innate immune system is a universal and ancient form of host defense against infection. Question: How does innate immunity (nonspecific) directly recognize invading micro-organisms to trigger a host defense response? Receptors of the innate immune system recognize broad structural motifs highly conserved within microbial species. Pattern Recognition Receptors • Receptors are referred to as Pattern-Recognition Receptors (PRRs). • Engagement of PRRs leads to triggering of signal pathways that promote inflammation. -Complement receptors: target cell wall components -Mannose-binding lectins: target mannose microbial carbohydrates in bacterial cell membranes -LPS-binding proteins: target bacterial lipopolysaccharide -Toll-like receptors: multiple targets -Scavenger receptors: targets phosphatidylserine and lipoproteins Toll-Like Receptors: The Simplified Explanation A way for innate cells to influence development of adaptive immune function. 11+ “Toll-like” receptors and ligands have been identified. They recognize various pattern motifs, and control subsequent signal transduction pathways. Nature Reviews Immunology 1; 135-145 (2001); TOLL-LIKE RECEPTORS AND INNATE IMMUNITY See Appendix for full list of receptors and ligands. • Recognition of pathogen via TLRs activates and matures Dendritic Cells and macrophages (APCs). • APCs process antigen and present to naïve T cells. • Presentation is accompanied by secretion of specific cytokines to control development of phenotypic T cell responses. Toll-Like Receptors: The Complex Explanation A general summary chart of innate components, effectors and function: Component Effectors Anatomic and physiologic barriers Skin and mucous membranes Physical barriers to limit Temperature, acidic pH, Lactic entry, spread, and acid, Chemical mediators replication of pathogens Inflammatory mediators Complement Direct lysis of pathogen or infected cells Cytokines and interferons Activation of other immune components Lysozymes Bacterial cell wall destruction Acute-phase proteins and lactoferrin Mediation of response Leukotrienes and prostaglandins Vasodilation and increased vascular permeability Polymorphonuclear cells Neutrophils, eosinophils Basophils, mast cells Phagocytosis and intracellular destruction of microorganisms Phagocytic-endocytic cells Monocytes and macrophages Dendritic cells Presentation of foreign antigen to lymphocytes Cellular components Table 1.1. Consult . Elsevier’s Integrated Immunology and Microbiology. 2007. Function Geha and Notarangelo Correlates 15. Chediak-Higashi Syndrome 25. Neutropenia 26. Chronic Granulomatous Disease * 27. Leukocyte Adhesion Deficiency * * Posted online Innate -> Adaptive Summary Immune responses of the innate immune system provide natural immunity and first line of defense against microorganisms via phagocytosis and intracellular killing, recruitment of other inflammatory cells, and presentation of antigens. Innate defense barriers include (1) anatomic barriers, (2) physiologic barriers, (3) Phagocytic barriers, and (4) inflammatory barriers. Tissue damage causes an influx of inflammatory cells through chemotaxis, activation, margination and diapedesis. Neutrophils are usually the first cell type to arrive at the site of tissue damage. Activation leads to respiratory bursts and release of granules to control bacterial growth. Mononuclear cells and macrophages engulf organisms via multiple mechanisms, leading to destruction within intracellular phagosomes. Chemokines and cytokines are critical for activation of innate immune functions. Defects may lead to severe clinical complications. Pattern Recognition Receptors present on innate immune system cells assist in the recognition of bacteria and virions. Recognition by PRRs leads to activation of multiple facets of cellular response. Signals from innate immune response drive maturation of T cell responses. Selected Cytokines and their functions. More Selected Cytokines and their functions. See syllabus appendix for more complete list of mediators, their source, and their biological function. Chemokines: Receptors and Associated Ligands Complement • Direct Cytolysis of foreign organisms • Antibodies recognize pathogens. • Complement interacts with antibodies. • An enyzmatic cascade occurs to initiate development of a “membrane attack complex” forming a pore channel in the lipid bilayer, causing osmotic lysis of the cell. • Opsonization of foreign organisms • Complement components bind to pathogens. • Bound components interact with complement receptors on the surface of macrophages, monocytes, and neutrophils. • Enhances phagocytosis and targeted organism destruction. • Activation and directed leukocyte migration • Proteolytic degradation of complement components results in leukocyte chemotactic anaphylatoxin. Critical Molecules in Injury • Hageman factor: Clotting and Complement activation • Thrombin: Clotting – Protease (34 kD) that acts on fibrinogen to produce fibrin • Kallikrein: Vascular reactions and Pain mediation – Plasma serine proteases; acts on kininogens to produce kinins • Plasmin: Management of Blood Clotting – Digestion of fibrin in blood clots • Bradykinin: Vasoactive nonapeptide – Potent vasodilator to increase post capillary venules permeability; activates phospholipase A2 Phospholipases then feed into the Arachadonic Acid Pathway….