* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 1 - The Mostowy Lab
Survey
Document related concepts
Cell culture wikipedia , lookup
Extracellular matrix wikipedia , lookup
Cell encapsulation wikipedia , lookup
Cellular differentiation wikipedia , lookup
Cell growth wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Cell membrane wikipedia , lookup
Cytokinesis wikipedia , lookup
Lipopolysaccharide wikipedia , lookup
Endomembrane system wikipedia , lookup
Signal transduction wikipedia , lookup
Type three secretion system wikipedia , lookup
List of types of proteins wikipedia , lookup
Transcript
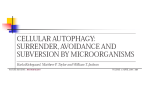
TICB-869; No. of Pages 9 Opinion Bacterial autophagy: restriction or promotion of bacterial replication? Serge Mostowy1,2,3,4 and Pascale Cossart1,2,3 1 Institut Pasteur, Unité des Interactions Bactéries-Cellules, Département de Biologie Cellulaire et Infection, F-75015 Paris, France Inserm, U604, F-75015 Paris, France 3 INRA, USC2020, F-75015 Paris, France 2 In order to survive inside the host cell, bacterial pathogens have evolved a variety of mechanisms to avoid or interfere with innate immune defenses. Several reports have shown that bacterial pathogens are targeted by the autophagy pathway, and autophagy has been increasingly recognized as an important defense mechanism to clear intracellular microbes. However, it now appears that some bacterial pathogens have evolved mechanisms to evade autophagic recognition or even co-opt the autophagy machinery for their own benefit as a replicative niche. A complete understanding of bacterial autophagy in vivo shall be critical to exploit autophagy and its therapeutic potential. Autophagy: bacterial friend or foe? Autophagy is an intracellular degradation process by which cytosolic materials are delivered to a lysosomal compartment (Figure 1). The ‘canonical’ autophagy pathway involves the initiation and elongation of double-membrane phagophores that close upon themselves to form autophagosomes — vacuoles typically 0.3–1.0 mm in diameter — to sequester cargo; this process requires a group of 35 autophagy-related (ATG) proteins conserved from yeast to humans [1–3] (Box 1). Many studies have revealed the diverse functions of autophagy in important cellular processes such as aging, development and inflammation [4]. Autophagy is also linked to a wide range of disease states, including microbial infection [5,6]. Autophagosomes were first regarded to sequester cytosolic material nonspecifically; however, the recently discovered paradigm of ‘selective’ autophagy, where autophagosomes can degrade cytosolic material in a selective manner as a result of receptor–ligand interactions, has highlighted the recognition of specific cargo, such as intracellular bacteria, by autophagy receptors for targeted lysosomal destruction. By binding to both ubiquitin and ATG8 family proteins (i.e. LC3s and GABARAPs), autophagy receptors can mediate targeting of ubiquitinated cargo to autophagy [7]. p62 (sequestosome 1 or SQSTM1) [8], NBR1 (neighbor of BRCA1 gene 1) [9], NDP52 (nuclear dot protein, 52 kDa) [10] and OPTN (optineurin) [11] are well-characterized autophagy receptors, and together represent an emerging Corresponding authors: Mostowy, S. ([email protected]); Cossart, P. ([email protected]) Keywords: autophagy; cytoskeleton; ubiquitination; Listeria; Shigella; Salmonella; mycobacteria. 4 Present address: Section of Microbiology, Centre for Molecular Microbiology and Infection, Imperial College London, Armstrong Road, London SW7 2AZ, UK. category of pattern recognition receptors, called sequestosome 1/p62-like receptors (SLRs), linking autophagy to innate immunity [12,13] (Table 1). Some pathogenic bacteria, in order to circumvent extracellular host immune responses, establish an intracellular niche to live inside host cells and replicate. Internalized bacteria first localize within a vacuolar compartment. This residence is sometimes very transient, and some pathogens, such as Listeria or Shigella, have evolved mechanisms to escape from their internalization vacuole to the cytosol and avoid destruction in phagolysosomes. Other pathogens, such as Salmonella or mycobacteria, interfere with the normal biogenesis of phagolysosomes to form replicative vacuoles. Discovered almost 10 years ago, bacterial autophagy has been highlighted as a fundamental host cell response to bacterial invasion in vitro by degrading intracellular pathogens located both in the cytosol and inside an internalization vacuole, including Listeria monocytogenes [14], Shigella flexneri [15], Salmonella Typhimurium [16] and Mycobacterium tuberculosis [17]. Since then, research in the field has exploded, revealing that some pathogens may avoid autophagy-mediated degradation, whereas others may exploit the autophagy machinery for intracellular survival. As a result, the in vivo consequence of bacterial autophagy remains unclear, and probably varies for different bacterial species. This review will focus on the recognition of pathogenic bacteria by the autophagy machinery to illustrate the emerging roles of autophagy during infection (Figure 2). In addition, we highlight the mechanisms evolved by pathogenic bacteria to avoid or co-opt the autophagy machinery, strongly suggesting that autophagy should not be strictly considered as antibacterial. Pathogens that escape to the cytosol Escape from the internalization vacuole is a bacterially driven process, and the survival of pathogens in the cytosol relies on their ability to avoid recognition and degradation by autophagy. L. monocytogenes: escape from autophagic destruction L. monocytogenes is a Gram-positive bacterium responsible for foodborne infections. The intracellular lifestyle of this pathogen has been well studied [18]. Listeria survives intracellularly by escaping from phagosomes using a combination of effectors including LLO, a pore-forming cytotoxin. Once in the cytosol, L. monocytogenes uses ActA, 0962-8924/$ – see front matter ß 2012 Elsevier Ltd. All rights reserved. http://dx.doi.org/10.1016/j.tcb.2012.03.006 Trends in Cell Biology xx (2012) 1–9 1 TICB-869; No. of Pages 9 Opinion Trends in Cell Biology xxx xxxx, Vol. xxx, No. x Phagophore Autolysosome Autophagosome Lyso Lyso Initiation Membrane elongation Completion Maturation Degradation TRENDS in Cell Biology Figure 1. Cellular events of the autophagy process. Cytoplasmic material, in this case a bacterium (gray), is enclosed by an isolation membrane, called a phagophore (blue), which elongates to form an autophagosome. The autophagosome fuses with the lysosome (Lyso), and the enclosed material is degraded in the autolysosome. which is expressed on the surface of the bacteria, to assemble the actin polymerization machinery and form actin tails for intra- and intercellular motility [19]. Strikingly, autophagic markers do not accumulate around intracytosolic L. monocytogenes polymerizing actin [20–22]. This situation results from the fact that ActA disguises Listeria from ubiquitination and autophagic recognition [23,24]. Therefore, ActA-expressing Listeria are not targeted to autophagic degradation. These findings suggest that host Box 1. Canonical autophagy versus non-canonical autophagy Canonical autophagy includes three different pathways: macroautophagy (herein referred to as autophagy) [1–3]; microautophagy (the engulfment of cytoplasmic material by invagination of the lysosomal membrane) [79]; and chaperone-mediated autophagy (the delivery of cytoplasmic proteins to the lysosome through interaction with chaperone proteins) [80]. Here, we focus on autophagy, which is: A degradation process that targets cytoplasmic material to double membrane vacuoles that fuse with lysosomes for destruction. Dependent on the systematic recruitment of ATG proteins to the phagophore (i.e. the autophagosome initiation site) to form and elongate an autophagosome that will fuse with the lysosomal compartment (Figure 1). Originally viewed as a random, non-selective degradation process. However, the involvement of specificity factors, such as ubiquitin [81], for selective autophagy is increasingly recognized. Classically activated in vitro by treating cells with rapamycin. Rapamycin is an inhibitor of mTOR, a serine/threonine protein kinase that is a suppressor of autophagy [82]. A mechanism to target bacteria to lysosomal degradation and therefore a critical component of innate immunity. Autophagy receptors act as cytosolic sensors and recruit ATG proteins at different steps of the invasion process. Non-canonical autophagy is a new and developing concept, and can be characterized by features that are different from those in canonical autophagy [3]. In particular, non-canonical autophagy is: A mechanism in which the double-membraned autophagosome does not require all of the ATG proteins to form, and may elongate from multiple sources of membrane. A process in which a subset of ATG proteins can be recruited to an already-existing and probably damaged membrane (e.g. a phagocytic vacuole containing Salmonella or mycobacteria) that is different from a phagophore. Potentially favorable in some cases of infection. Certain bacteria may replicate inside autophagosome-like structures (i.e. vacuoles with a double membrane and a subset of ATG proteins that will not fuse with the lysosomal compartment) generated by noncanonical autophagy. Bacterial species apparently benefitting from non-canonical autophagy includes Brucella and Staphylococcus. 2 proteins that interact with ActA on the surface of Listeria may disguise the bacteria to prevent autophagic recognition, or that ActA itself prevents recruitment of proteins normally involved in autophagy. Indeed, bacteria lacking ActA are ubiquitinated and targeted to autophagy. InlK is another Listeria surface protein that contributes to escape from autophagy [25]. This protein is poorly expressed in vitro, but when expressed it can protect bacteria from autophagy in the absence of ActA. Instead of recruiting the actin polymerization machinery, Listeria expressing InlK recruits the major vault protein (MVP) to evade ubiquitination and autophagic recognition. Several reports have shown that L. monocytogenes lacking LLO production fail to induce autophagy [14,21,26], suggesting that autophagy induction by Listeria is LLO dependent. Indeed, purified LLO triggers formation of aggregates associated with ubiquitin, p62 and LC3 [27], all of which are hallmarks of autophagosomes [28]. Cytosolic lectins (e.g. Galectin 3, 8 and 9) are also recruited to vesicles damaged by LLO and probably other factors [29,30], and this recruitment may trigger autophagy (see Salmonella below). However, work in bone marrowderived macrophages has shown that autophagy triggered by host-cell membrane remnants, created by rupture of phagosomal vacuoles by LLO, does not control intracytosolic Listeria replication [31]. By contrast, work in Drosophila has shown that LLO-dependent autophagy, triggered by the pattern-recognition receptor PGRP-LE, may control Listeria replication [32]. Further studies are therefore required to clarify the role of LLO-mediated autophagy induction during bacterial infection. Together, L. monocytogenes can avoid autophagic destruction, at least in vitro, by preventing the accumulation of ubiquitinated substrates at the bacterial cell surface; however, it triggers autophagy by LLO-mediated membrane rupture. The precise, and probably multiple, roles of autophagy in Listeria pathogenesis thus remain to be established. S. flexneri: a target of autophagic destruction S. flexneri is a Gram-negative, foodborne pathogen that invades the colonic mucosa, causing inflammation and diarrhea. The infectious process at the cellular level is similar to that of L. monocytogenes, but the mechanisms that Shigella uses to escape from the vacuole are less understood. Once in the cytosol, the actin-based motility of Shigella is mediated by its surface expressed IcsA protein [19]. TICB-869; No. of Pages 9 Opinion Trends in Cell Biology xxx xxxx, Vol. xxx, No. x Table 1. Autophagy receptors implicated in bacterial autophagy and the bacteria they recognize, and bacterial effectors that prevent autophagy recognition* Autophagy receptor p62 OPTN Targeted bacteria L. monocytogenes, S. flexneri, S. Typhimurium, M. marinum, M. tuberculosis S. flexneri L. monocytogenes, S. flexneri, S. Typhimurium S. Typhimurium Effector protein ActA Bacteria L. monocytogenes InlK L. monocytogenes IcsB S. flexneri NBR1 NDP52 Mode of action Self-oligomerization; binds ubiquitin and ATG8 family proteins References [24,35,51,60,89] Interacts with p62 via PB1 domains; binds ubiquitin and ATG8 family proteins Binds ubiquitin and ATG8 family proteins; binds ubiquitinated bacteria in the cytosol and binds Galectin 8 at vesicle damage; NDP52 and p62 form non-overlapping subdomains around ubiquitinated bacteria Binds ubiquitin and ATG8 family proteins; OPTN and NDP52 localize to common subdomains around ubiquitinated bacteria separate from p62; phosphorylation of OPTN promotes selective autophagy [24,90] [10,24,29,53] Role Recruits Arp2/3 for actin-based motility; masks from ubiquitination and autophagy recognition by p62, NDP52 Recruits MVP; masks from ubiquitination and autophagy recognition by p62 before ActA Prevents ATG5 recognition of IcsA; masks from ubiquitination and autophagy recognition by septin cage, p62, NDP52; prevents recognition byTECPR1 [11] References [23,24] [25] [15,24,35,36] * Aside from bacterial effectors listed here, there are likely to be others that have not yet been discovered. At the Shigella-entry site, NOD1 and NOD2, key pathogen recognition receptors, are recruited together with ATG16L1, a protein required for phagophore formation (Box 1) and associated with Crohn’s disease, beneath the plasma membrane [26]. NOD proteins sense the bacterial invasion process as danger signals, and this sensing triggers autophagy in the infected cell cytosol. At the same time, membrane remnants, generated by Shigella-mediated membrane damage, are ubiquitinated and recognized by autophagy receptors, thereby helping to control inflammatory signaling [33]. Indeed, inflammasome components have been localized to damaged membranes, and their ubiquitination and degradation by p62-mediated autophagy leads to a dampened inflammatory response [34]. Cytosolic lectins may also detect vesicle damage by Shigella and trigger autophagy [29,30]. Thus, membrane damage is considered to alert the host cell to subsequent bacterial invasion; however, further studies are required to determine whether induction of autophagy by membrane damage can limit Shigella replication. Autophagy is also induced by the presence of cytosolic Shigella. In epithelial cells infected with Shigella, autophagy is triggered by the recognition of IcsA by ATG5 [15], a protein critical for autophagosome elongation and completion (Figure 1). However, Shigella can evade autophagy by expressing IcsB, a type III secretion system (T3SS) effector, which competitively binds IcsA to block ATG5 binding. Thus, IcsB enables Shigella to evade autophagic recognition [15,24,26,35]. Recent work has identified a Tectonin domain-containing protein, TECPR1, as a receptor for ATG5 in Shigella-infected cells [36]. Via binding to ATG5, and not to ubiquitinated substrate, TECPR1 activity promotes autophagosome–lysosome fusion and mediates bacterial autophagy [37]. Strikingly, septin cage-like structures target Shigella to autophagy, and are required for this process [24,35] (Box 2). Septins are GTP-binding proteins that assemble as filaments and approximately 0.6-mm diameter rings, and accumulate at bacterial entry sites and around intracytosolic bacteria [38]. In the cytosol, septin rings assemble at sites of IcsA-induced actin polymerization and form cages surrounding the bacterium to restrict cell-to-cell spreading [35]. The precise role of septins in autophagy is unknown, yet work has shown that septins help to scaffold ubiquitinated proteins and autophagy receptors around actin-polymerizing bacteria [24,35]. Whether septin cages and autophagy serve to clear intracytosolic Shigella in vivo has yet to be tested. Mycobacterium marinum: recruitment of canonical and non-canonical autophagy M. marinum causes a systemic tuberculosis-like disease in fishes and frogs, and a localized disease in humans, and has been widely used as an alternative model to study M. tuberculosis. Like most pathogenic mycobacteria, M. marinum survives within host macrophages by preventing phagolysosome fusion [39]. However, M. marinum can also escape from the phagosome to the cytosol and, unlike other mycobacteria, initiate actin-based motility [19,39]. Mutations in ESX-1, a specialized secretion pathway in mycobacteria that encodes for genes with membrane lysing activity, attenuates the virulence of M. marinum by abrogating phagosomal escape. Recent work has shown that phagosomes containing M. marinum recruit the autophagic marker LC3, and this recruitment depends on ESX-1 activity [40]. M. marinum can temporarily reside in a LC3-decorated compartment, characterized as a late endosome lacking the degradative properties of a lysosome. By contrast, when autophagy is stimulated by rapamycin, there is increased LC3 recruitment to the M. marinum-containing compartment, and this leads to its fusion with the lysosome. This suggests that autophagy can help to eliminate mycobacterial-containing phagosomes, in agreement with studies using M. tuberculosis (see below). 3 TICB-869; No. of Pages 9 Opinion Trends in Cell Biology xxx xxxx, Vol. xxx, No. x Bacterial invasion Autophagy of bacteria inside a phagosome Autophagy of membrane remnants Ub 3 LC 3 LC AR AR Bacteria inside a damaged phagosome Cytosolic bacteria Ub Ub 3 3 3 LC LC LC Autophagy of bacteria and septin cage formation AR AR AR Autophagy of cytosolic bacteria Autophagy of bacteria inside a damaged phagosome TRENDS in Cell Biology Figure 2. Different autophagy pathways triggered by bacterial invasion. Ub, ubiquitin; AR, autophagy receptor (see Table 1 for examples); LC3, ATG8. In the cytosol, ubiquitinated M. marinum can be found within organelles that resemble autophagosomes (i.e. they have a double membrane) albeit lacking canonical autophagy markers ATG5 and LC3 [41]. In close proximity to cytosolic bacteria, a mixture of host membrane remnants and shed M. marinum cell walls are also ubiquitinated [41]. From these observations, it has been proposed that ubiquitinated M. marinum cell walls are sequestered into autophagy-like organelles by a non-canonical autophagy pathway, and cell wall shedding may enable bacterial escape from this process. Indeed, similarly to Listeria [23,24,35] and Shigella [15,24,35], M. marinum that polymerize actin tails are not recognized by ubiquitin. By contrast, ubiquitin, p62, LC3 and septin caging have been observed around cytosolic M. marinum at the onset of actin tail formation [24,35,41]. Considering the role of septin caging during Shigella infection, it is likely that septin caging also helps the targeting of M. marinum to 4 autophagy (Box 2). A major issue is now to determine the respective roles of canonical and non-canonical pathways in the autophagy of M marinum. Francisella tularensis: autophagic restriction of cytosolic replication F. tularensis is a Gram-negative, facultative intracellular bacterium that causes tularemia, a human infection that starts through contact with infected animal tissues or spread through an arthropod vector. Following entry into cells, F. tularensis is localized within a phagosome, but escapes to the cytosol to avoid destruction in phagolysosomes [42]. In the cytosol, Francisella does not exhibit actin-based motility, and instead replicates rapidly until the cell undergoes apoptosis and the bacteria are released to continue infection. However, an infected host cell can restrict cytosolic replication by sequestering Francisella into a compartment called the Francisella-containing TICB-869; No. of Pages 9 Opinion Trends in Cell Biology xxx xxxx, Vol. xxx, No. x Box 2. Autophagy and the cytoskeleton Proteins involved in actin-based motility are also connected to bacterial autophagy. Septins, increasingly well-characterized cytoskeleton components [38], are recruited with autophagy proteins to some intracytosolic bacteria and form cage-like structures to counteract actin tail formation and restrict bacterial dissemination [35] (Figure I). These observations have linked septin caging and autophagy as interdependent host defense processes, and suggest that a more comprehensive understanding of septins and autophagy will have important consequences for the understanding of bacterial pathophysiology and its control. In the cytosol, Listeria, Shigella and M. marinum all share the ability to polymerize actin tails. However, septin caging has been observed for Shigella and M. marinum, but not for Listeria [35]. In this case, caging does not occur because Listeria ActA masks the bacteria from autophagic recognition so that septin caging is also avoided [24,35]. Comparative investigation of these different intracellular bacteria has highlighted the role for actin and septins in selective autophagy, and has revealed that Shigella and Listeria are recognized by different pathways of autophagy [24,35] (Figure 2). Septin-mediated bacterial autophagy will have to be studied in vivo across a panel of pathogens to fully understand its role in host defense. Given that septin assembly [38] and autophagy [1,2] are processes well-conserved from yeast to humans, their interdependence may not be limited to bacterial autophagy. In uninfected cells, levels of autophagy critical components are reduced upon septin depletion [24,35], consistent with the hypothesis that multiple autophagic activities benefit from septin assembly. It is now critical to investigate the role of septin assemblies in various autophagic processes, including starvation-induced autophagy [83], microautophagy [79], chaperone-mediated autophagy [80], and other processes of selective autophagy such as clearance of the midbody ring [84], entotic cell death [85], mitophagy [86] and virophagy [87,88]. TRENDS in Cell Biology Figure I. The Shigella-septin cage. Recruitment of septin (SEPT9, red) to actin (green)-polymerizing S. flexneri (blue) devoid of actin tails. Scale bar, 1 mm. Reproduced, with permission, from [35]. vacuole (FCV), which shares several hallmarks of canonical autophagosomes, including a double membrane and LC3 labeling [43]. The precise role of FCV compartmentalization remains unknown, yet the expression of type IV pili (Tfp) [44] may help F. tularensis to avoid this compartmentalization. In agreement with this, microarray analysis of cells infected with F. tularensis has shown that several canonical autophagy markers are down-regulated during infection [45]. However, the potential subversion of autophagy by F. tularensis awaits further characterization. Streptococcus pyogenes: degradation by non-canonical autophagy S. pyogenes [Group A Streptococcus (GAS)] is a Grampositive bacterium responsible for a variety of infectious diseases associated with significant morbidity and mortality worldwide. It is noninvasive, but once taken up by phagocytic cells, GAS escapes from phagosomes using streptolysin O (SLO), a cholesterol-dependent cytolysin [46]. SLO induces autophagy, and cytosolic GAS are contained within an LC3-positive, membrane-bound structure called GAS-containing autophagosome-like vacuoles (GcAVs) [47]. Unlike canonical autophagosome formation (Box 1), GcAV formation requires the small GTPases Rab7, Rab9a and Rab23 [48,49]; otherwise, the molecules responsible for GcAV formation – and not for canonical autophagosome formation – are largely unknown. GAS are degraded upon fusion of GcAVs with lysosomes, and in autophagy-deficient cells, GAS survive and replicate [50]. Thus, non-canonical autophagy may represent a critical defense against GAS infection. Pathogens that survive inside the phagosome Several pathogens can survive inside the vacuole and avoid destruction upon fusion, or by preventing fusion, with the lysosome. For these pathogens, escape to the cytosol is considered to be accidental. Remarkably, these bacteria can be recognized by autophagy both in the phagosome and in the cytosol, and their survival may be critically linked to their ability to co-opt the autophagy machinery. Salmonella Typhimurium: a paradigm of selective autophagy S. Typhimurium is a Gram-negative intracellular foodborne pathogen with a broad host range. Following Salmonella invasion of host cells, most bacteria reside and replicate within a modified endosomal compartment called the Salmonella-containing vacuole (SCV) [51]. However, approximately 25% of S. Typhimurium become cytosolic, and Salmonella in the cytosol can be surrounded by ubiquitin [20]. The first autophagy receptor discovered to target ubiquitinated Salmonella to autophagic destruction was p62 [52]. Shortly thereafter, NDP52 was also shown to act as an autophagy receptor that restricts the replication of ubiquitinated Salmonella in the cytosol [10]. The unique features of NDP52 important for bacterial autophagy are unknown, although p62 and NDP52 may be recruited to 5 TICB-869; No. of Pages 9 Opinion distinct membrane domains surrounding bacteria [53]. Interestingly, post-translational modification may be critical for autophagy receptor function [11]. The autophagy receptor OPTN, which seems to function more closely with NDP52 than p62, is phosphorylated to efficiently detect and eliminate ubiquitinated, cytosolic Salmonella [11]. The role of OPTN in other autophagy pathways, and the general role of post-translational modifications in autophagy receptor function, remain relatively unexplored. Independent of ubiquitin-mediated autophagy recognition, a diacylglycerol (DAG)-dependent signaling pathway also contributes to anti-Salmonella autophagy [54]. Salmonella targeted to autophagy are indeed labeled with either ubiquitin or DAG, suggesting that at least two autophagy pathways independently promote bacterial clearance. A major issue is now to investigate what other non-ubiquitin signals may target bacteria to autophagy. Recent work has revealed that NDP52 can be recruited to the damaged vacuoles by Galectin 8 (LGALS8) [29]. Strikingly, this recruitment occurs independently of ubiquitin, which is critical for NDP52 recruitment to cytosolic bacteria [10]. This suggests a temporal pattern of autophagy recruitment (i.e. Galectin 8-mediated recruitment of NDP52 occurs first and is followed by a ubiquitin-dependent recruitment of NDP52) and highlights the emerging concept that different pathways of bacterial autophagy may act at distinct steps of the infectious process, an issue that now deserves careful characterization using other invasive bacteria. Considering work showing that autophagosome-like (i.e. double-membrane, LC3-positive) structures can surround bacteria still residing within the SCV independent of canonical phagophore generation [55,56] (Box 1), future studies should also investigate whether bacteria targeted by autophagy have only compromised the SCV, or have fully escaped from the SCV. M. tuberculosis: delivery of the phagosome to the lysosome by autophagy The pathogenicity of M. tuberculosis, the causative agent of human tuberculosis, is largely attributed to its ability to survive within macrophages by arresting phagosomal maturation toward an acidified phagolysosome, and thus residing in a phagosomal compartment that maintains many characteristics of an early endosome [57]. However, recent studies using cryo-immunogold electron microscopy and single-cell fluorescence resonance energy transfer (FRET)based methods have reported an ESX-1-dependent mechanism of phagosomal escape of M. tuberculosis into the cytosol [58,59], which may lead to necrotic death of the infected host cell [59]. Whereas M. tuberculosis can clearly escape to the cytosol, the role of autophagy in recognizing cytosolic M. tuberculosis and in delaying host cell necrosis caused by cytosolic entry of M. tuberculosis has not been investigated. In contrast to the well-documented ability of M. tuberculosis to prevent phagosome maturation and allow bacterial survival, several studies have shown that autophagy can help to efficiently eliminate phagosomal M. tuberculosis [60]. Indeed, the induction of autophagy by starvation, mTOR (mammalian target of rapamycin) inhibition, vitamin D and interferon-gamma (IFNg) is reported to 6 Trends in Cell Biology xxx xxxx, Vol. xxx, No. x contribute to phagosome maturation and M. tuberculosis elimination [60,61]. How mycobacteria can survive in phagosomes, but not in phagosomes having recruited the autophagy machinery, is a key issue. It has been suggested that cytosolic components, such as ubiquitin, p62 and ribosomal proteins [62], may equip mycobacterial autophagolysosomes (i.e. phagosomes surrounded by a doublemembrane decorated with LC3) with potent antimicrobial properties to abrogate M. tuberculosis survival [12]. In agreement with this proposal, recent work has shown that vitamin D is required for IFNg-mediated induction of autophagy, the maturation of phagosomes and the production of cathelicidin to result in antimicrobial activity against M. tuberculosis [63]. Despite convincing evidence obtained in vitro, a role for autophagy in control of M. tuberculosis in vivo has yet to be shown. This will be a critical issue, considering that clinical isolates of M. tuberculosis have been suggested to manipulate autophagy for their own survival [64]. Legionella pneumophila: inhibition of autophagosome maturation and exploitation of the autophagy machinery L. pneumophila, a Gram-negative bacterium, is the causative agent of a form of pneumonia called Legionnaires’ disease. The natural hosts of L. pneumophila are different species of protozoa abundant in aquatic environments, and the capacity to grow intracellularly in protozoa has selected for virulence traits that allow Legionella to also infect humans [65]. Inside mammalian phagocytic cells, L. pneumophila recruits vesicles emerging from the endoplasmic reticulum (ER), and remodels Legionella-containing vacuoles (LCVs) to evade the phagocytic pathway and support bacterial replication [66]. LCVs in macrophages from mice resistant to Legionella infection (e.g. C57BL/6) rapidly fuse with lysosomes, resulting in bacterial degradation. However, in macrophages from mice permissive to Legionella infection (e.g. A/J, which are deficient in Naip5, a NOD-like receptor), bacteria can replicate within LCVs that do not fuse with lysosomes. Studies have shown that these bacteria persist in LCVs that also recruit LC3 and resemble autophagosomes, and the ability of Legionella to inhibit maturation of these vacuoles is considered to promote bacterial survival [67]. The precise role of Legionella effector proteins and autophagy in Legionella survival now requires further dissection using host genotypes that are permissive and resistant to infection. Coxiella burnetii: exploitation of the autophagy machinery C. burnetii, a highly infectious Gram-negative bacterium, is the causative agent of Q fever. An obligate intracellular pathogen, C. burnetii enters a phagocytic pathway and interacts with the autophagy machinery shortly after internalization [68,69]. In this case, the autophagy marker LC3 is recruited to the Coxiella-containing vacuole. This interaction delays fusion with lysosomes and enables bacteria to replicate [68,70]. Strikingly, the number of infected cells, the size of the vacuoles and the bacterial load all increase when autophagy is stimulated by rapamycin, TICB-869; No. of Pages 9 Opinion highlighting the benefit of autophagy for Coxiella survival. Similarly to L. pneumophila, C. burnetii also encodes a functional type IV secretion system (T4SS), and C. burnetii is likely to secrete T4SS effectors which co-opt the autophagic machinery and create a replicative niche. How Coxiella exploits the autophagy machinery for better replication awaits investigation. Yersinia pseudotuberculosis: promotion of bacterial replication by autophagy Y. pseudotuberculosis is an enteric pathogen and Y. pestis is the causative agent of plague; both of these species possess T3SS and deliver effectors called Yersinia outer proteins (Yops). After internalization into host cells, Y. pseudotuberculosis replicates inside Yersinia-containing vacuoles (YCVs) that display markers of autophagy (i.e. a double membrane and LC3 recruitment) [71]. When autophagy is stimulated by rapamycin, YCVs increase in size with more replicating bacteria. When autophagy is inhibited by 3-methyladenine (3-MA), an inhibitor of phosphoinositide 3-kinases (PI3Ks), YCVs mature into an acidic bactericidal compartment. Together, these results strongly suggest that autophagy can promote Y. pseudotuberculosis replication. YCVs containing Y. pestis are also recognized by autophagy [72]. However, unlike Y. pseudotuberculosis, Y. pestis-containing YCVs may colocalize with markers of acidic lysosomes in the absence of autophagy inhibition. This suggests that autophagy is not involved in promoting Y. pestis survival, in agreement with observations that Y. pestis does not require autophagy for intracellular replication [72] and instead proliferates by suppressing innate immune responses [73]. Together, the role of autophagy in Yersinia intracellular survival is different between the two species. Future work should exploit interspecies differences to investigate the autophagy of Yersinia, and a potential role for Yops in modifying this process. Brucella abortus: subversion of the autophagy machinery B. abortus is a Gram-negative, intracellular pathogen which causes brucellosis, a zoonosis which can result in spontaneous abortion and infertility in a wide variety of animals. Shortly after Brucella entry into host cells in a lipid raft-dependent manner, Brucella-containing vacuoles (BCVs) transiently interact with endosomes, acquire early endosomal markers, become acidified and fuse with ER-derived membrane to establish a replicative compartment [74]. Recent work has shown that bacteria convert their ER-derived replicative vacuole into an autophagosome-like compartment, called autophagic BCVs (aBCVs) [75]. Indeed, Brucella generate aBCVs by co-opting autophagosome initiation factors ATG1 (ULK1), Beclin1 (ATG6) and ATG14. By contrast, autophagosome elongation factors ATG4B, ATG5, ATG7, LC3B and ATG16L1 are not required for aBCV formation. Although the mechanism by which B. abortus manipulates this non-canonical autophagy pathway has yet to be fully defined, the Brucella T4SS may be required for biogenesis of aBCVs, as has previously been shown for biogenesis of replicative BCVs [74]. Trends in Cell Biology xxx xxxx, Vol. xxx, No. x Interestingly, the formation of aBCVs from ER-derived BCVs is similar to the formation of autophagosomal, ERderived LCVs in the case of Legionella (see above). This suggests that Brucella and Legionella exploit similar components of the autophagy machinery for replication and survival [75]. The ability of pathogenic bacteria to subvert the autophagy machinery and promote their infection process in vivo has yet to be shown. Staphylococcus aureus: replication in an autophagosomal niche S. aureus is a Gram-positive bacterium that causes a wide range of infectious diseases and can lead to septic and toxic shock. Classically considered an extracellular pathogen, S. aureus has been increasingly recognized to invade cells and replicate intracellularly [76]. After invasion of epithelial cells, S. aureus can be found in autophagosome-like vacuoles, characterized by double membrane and colocalization with LC3 [77]. This process is dependent on agr, a global regulator of S. aureus virulence. S. aureus-containing autophagosomes do not fuse with lysosomes, creating a niche for bacteria to replicate. After replication, S. aureus eventually escape from autophagosomes into the cytoplasm and induce apoptosis-like cell death. Therefore, in the case of S. aureus, the autophagy machinery is essential for bacterial replication and host cell killing. Similarly to what has been described for LLO and SLO (see above), a-hemolysin (Hla) is a pore-forming toxin secreted by S. aureus that can trigger autophagy [78]. Work has shown that membrane damage mediated by Hla is required for the recruitment of autophagy markers (e.g. LC3 labeling) to S. aureus-containing phagosomes that do not fuse with lysosomes. Together with the fact that Hla-induced autophagy requires ATG5 but not Beclin1 nor PI3Kinase activity [78], this suggests the involvement of a non-canonical autophagy pathway to prevent the maturation of S. aureus containing autophagosomes. Concluding remarks Autophagy controls the fate of some intracellular bacteria, such as Listeria, Shigella, Francisella, Salmonella and mycobacteria, through the ATG protein-dependent machineries required for canonical autophagy (Box 1). As a result, canonical autophagy deserves recognition as a critical component of innate immunity. By contrast, other bacterial pathogens, such as Legionella, Coxiella, Yersinia, Brucella and Staphylococcus, benefit from autophagy pathways, and may subvert the autophagy machinery in favor of an infection process. These alternative outcomes highlight the molecular complexity that underlies bacterial autophagy, and suggests possible difficulties in therapeutic modulation of autophagy to resolve bacterial infection. Is autophagy strictly an antibacterial process in vivo? Clearly, in vitro data show that more research is required to answer this question (Box 3). Key molecules, mechanisms and pathways have to be tested across a variety of cell types and bacterial pathogens. In the future, a detailed comparative survey of the composition of the various bacterial autophagosomes will be crucial to elucidate the molecular features unique to the various autophagic 7 TICB-869; No. of Pages 9 Opinion Box 3. Outstanding questions Are there different roles for different autophagy receptors? Under what circumstance is ubiquitination a prerequisite for autophagy receptor recruitment? What are the ubiquitinated proteins that allow recognition by autophagy receptors? Are they of host or bacterial origin? DAG and Galectin 8 are examples of non-ubiquitin signals that may target bacteria to autophagy. What other non-ubiquitin signals may target bacteria to autophagy? Are they all lipid-based sensors? Can autophagy receptors target bacteria to different autophagy pathways? Can recognition by autophagy receptors be co-opted for growth by bacterial pathogens? What are the sources of membrane during bacterial autophagy? What are the different molecules and mechanisms underlying bacterial autophagy? Do they overlap with other processes of autophagy, such as virophagy and/or mitophagy? What is the role of the cytoskeleton? Under what circumstance is autophagy antibacterial? Under what circumstance can bacteria co-opt autophagy? Which bacterial effectors enable survival inside autophagosomes? How can bacterial autophagy be exploited for therapeutics and clinical application? pathways (Figure 2). It will also be critical to test the role of cytokines, such as tumor necrosis factor alpha and IFNg, and other physiological stimuli for their ability to induce autophagy and/or autophagy receptor activity. Finally, a major issue will be to validate the molecular and cellular events analyzed in vitro during bacterial infection in vivo using relevant animal models including Drosophila, zebrafish and mice. Nevertheless, the results generated from the study of bacterial autophagy are expected to provide fundamental advances in understanding the biology of cellular immunity. They could also suggest the development of new strategies aimed at combating infectious diseases, and possibly other human diseases arising from a dysfunctional autophagic response. Acknowledgments Work in the Serge Mostowy laboratory is supported by a Wellcome Trust Research Career Development Fellowship. Work in the Pascale Cossart laboratory is supported by the Institut Pasteur, INSERM, INRA, Fondation Louis-Jeantet and a European Research Council Advanced Grant Award (233348). References 1 Mizushima, N. et al. (2011) The role of Atg proteins in autophagosome formation. Annu. Rev. Cell Dev. Biol. 27, 107–132 2 Nakatogawa, H. et al. (2009) Dynamics and diversity in autophagy mechanisms: lessons from yeast. Nat. Rev. Mol. Cell Biol. 10, 458–467 3 Codogno, P. et al. (2012) Canonical and non-canonical autophagy: variations on a common theme of self-eating? Nat. Rev. Mol. Cell Biol. 13, 7–12 4 Mizushima, N. and Komatsu, M. (2011) Autophagy: renovation of cells and tissues. Cell 147, 728–741 5 Levine, B. et al. (2011) Autophagy in immunity and inflammation. Nature 469, 323–335 6 Mizushima, N. et al. (2008) Autophagy fights disease through cellular self-digestion. Nature 451, 1069–1075 7 Johansen, T. and Lamark, T. (2011) Selective autophagy mediated by autophagic adapter proteins. Autophagy 7, 279–296 8 Pankiv, S. et al. (2007) p62/SQSTM1 binds directly to Atg8/LC3 to facilitate degradation of ubiquitinated protein aggregates by autophagy. J. Biol. Chem. 282, 24131–24145 9 Kirkin, V. et al. (2009) A role for NBR1 in autophagosomal degradation of ubiquitinated substrates. Mol. Cell 33, 505–516 8 Trends in Cell Biology xxx xxxx, Vol. xxx, No. x 10 Thurston, T.L.M. et al. (2009) The TBK1 adaptor and autophagy receptor NDP52 restricts the proliferation of ubiquitin-coated bacteria. Nat. Immunol. 10, 1215–1221 11 Wild, P. et al. (2011) Phosphorylation of the autophagy receptor optineurin restricts Salmonella growth. Science 333, 228–233 12 Deretic, V. (2011) Autophagy as an innate immuntiy paradigm: expanding the scope and repertoire of pattern recognition receptors. Curr. Opin. Immunol. 24, 21–31 13 Ogawa, M. et al. (2011) Manipulation of autophagy by bacteria for their own benefit. Microbiol. Immunol. 55, 459–471 14 Py, B.F. et al. (2007) Autophagy limits Listeria monocytogenes intracellular growth in the early phase of primary infection. Autophagy 3, 117–125 15 Ogawa, M. et al. (2005) Escape of intracellular Shigella from autophagy. Science 307, 727–731 16 Birmingham, C.L. et al. (2006) Autophagy controls Salmonella infection in response to damage to the Salmonella-containing vacuole. J. Biol. Chem. 281, 11374–11383 17 Gutierrez, M.G. et al. (2004) Autophagy is a defense mechanism inhibiting BCG and Mycobacterium tuberculosis survival in infected macrophages. Cell 119, 753–766 18 Cossart, P. (2011) Illuminating the landscape of host–pathogen interactions with the bacterium Listeria monocytogenes. Proc. Natl. Acad. Sci. U.S.A. 103, 19484–19491 19 Gouin, E. et al. (2005) Actin-based motility of intracellular pathogens. Curr. Opin. Microbiol. 8, 35–45 20 Perrin, A.J. et al. (2004) Recognition of bacteria in the cytosol of mammalian cells by the ubiquitin system. Curr. Biol. 14, 806– 811 21 Birmingham, C.L. et al. (2007) Listeria monocytogenes evades killing by autophagy during colonization of host cells. Autophagy 3, 442–451 22 Kathryn, A.R. et al. (2003) Cytoplasmic bacteria can be targets for autophagy. Cell. Microbiol. 5, 455–468 23 Yoshikawa, Y. et al. (2009) Listeria monocytogenes ActA-mediated escape from autophagic recognition. Nat. Cell Biol. 11, 1233–1240 24 Mostowy, S. et al. (2011) p62 and NDP52 proteins target intracytosolic Shigella and Listeria to different autophagy pathways. J. Biol. Chem. 286, 26987–26995 25 Dortet, L. et al. (2011) Recruitment of the major vault protein by InlK: a Listeria monocytogenes strategy to avoid autophagy. PLoS Pathog. 7, e1002168 26 Travassos, L.H. et al. (2009) Nod1 and Nod2 direct autophagy by recruiting ATG16L1 to the plasma membrane at the site of bacterial entry. Nat. Immunol. 11, 55–62 27 Viala, J.P.M. et al. (2008) A bacterial pore-forming toxin forms aggregates in cells that resemble those associated with neurodegenerative diseases. Cell. Microbiol. 10, 985–993 28 Mizushima, N. et al. (2010) Methods in mammalian autophagy research. Cell 140, 313–326 29 Thurston, T.L.M. et al. (2012) Galectin 8 targets damaged vesicles for autophagy to defend cells against bacterial invasion. Nature 482, 414– 418 30 Paz, I. et al. (2010) Galectin-3, a marker for vacuole lysis by invasive pathogens. Cell. Microbiol. 12, 530–544 31 Meyer-Morse, N. et al. (2010) Listeriolysin O is necessary and sufficient to induce autophagy during Listeria monocytogenes infection. PLoS ONE 5, e8610 32 Yano, T. et al. (2008) Autophagic control of Listeria through intracellular innate immune recognition in drosophila. Nat. Immunol. 9, 908–916 33 Dupont, N. et al. (2009) Shigella phagocytic vacuolar membrane remnants participate in the cellular response to pathogen invasion and are regulated by autophagy. Cell Host Microbe 6, 137–149 34 Shi, C.S. et al. (2012) Activation of autophagy by inflammatory signals limits IL-1B production by targeting ubiquitinated inflammasomes for destruction. Nat. Immunol. 13, 255–263 35 Mostowy, S. et al. (2010) Entrapment of intracytosolic bacteria by septin cage-like structures. Cell Host Microbe 18, 433–444 36 Ogawa, M. et al. (2011) A Tecpr1-dependent selective autophagy pathway targets bacterial pathogens. Cell Host Microbe 9, 376–389 37 Chen, D. et al. (2012) A mammalian autophagosome maturation mechanism mediated by TECPR1 and the Atg12–Atg5 conjugate. Mol. Cell 45, 629–641 TICB-869; No. of Pages 9 Opinion 38 Mostowy, S. and Cossart, P. (2012) Septins: the fourth component of the cytoskeleton. Nat. Rev. Mol. Cell Biol. 13, 183–194 39 Stamm, L.M. and Brown, E.J. (2004) Mycobacterium marinum: the generalization and specialization of a pathogenic mycobacterium. Microbes Infect. 6, 1418–1428 40 Lerena, M.C. and Colombo, M.I. (2011) Mycobacterium marinum induces a marked LC3 recruitment to its containing phagosome that depends on a functional ESX-1 secretion system. Cell. Microbiol. 13, 814–835 41 Collins, C.A. et al. (2009) Atg5-independent sequestration of ubiquitinated mycobacteria. PLoS Pathog. 5, e1000430 42 Santic, M. et al. (2006) Francisella tularensis travels a novel, twisted road within macrophages. Trends Microbiol. 14, 37–44 43 Checroun, C. et al. (2006) Autophagy-mediated reentry of Francisella tularensis into the endocytic compartment after cytoplasmic replication. Proc. Natl. Acad. Sci. U.S.A. 103, 14578–14583 44 Naslund Salomonsson, E. et al. (2011) Type IV pili in Francisella – a virulence trait in an intracellular pathogen. Front. Microbiol. 2, 29 45 Butchar, J.P. et al. (2008) Microarray analysis of human monocytes infected with Francisella tularensis identifies new targets of host response subversion. PLoS ONE 3, e2924 46 Cole, J.N. et al. (2011) Molecular insight into invasive group A streptococcal disease. Nat. Rev. Microbiol. 9, 724–736 47 Nakagawa, I. et al. (2004) Autophagy defends cells against invading group A Streptococcus. Science 306, 1037–1040 48 Yamaguchi, H. et al. (2009) An initial step of GAS-containing autophagosome-like vacuoles formation requires Rab7. PLoS Pathog. 5, e1000670 49 Nozawa, T. et al. (2012) The small GTPases Rab9A and Rab23 function at distinct steps in autophagy during Group A Streptococcus infection. Cell. Microbiol. http://dx.doi.org/10.1111/ j.1462-5822.2012.01792.x 50 Sakurai, A. et al. (2010) Specific behavior of intracellular Streptococcus pyogenes that has undergone autophagic degradation is associated with bacterial streptolysin O and host small G proteins Rab5 and Rab7. J. Biol. Chem. 285, 22666–22675 51 Brumell, J.H. and Grinstein, S. (2004) Salmonella redirects phagosomal maturation. Curr. Opin. Microbiol. 7, 78–84 52 Zheng, Y.T. et al. (2009) The adaptor protein p62/SQSTM1 targets invading bacteria to the autophagy pathway. J. Immunol. 183, 5909– 5916 53 Cemma, M. et al. (2010) The ubiquitin-binding adaptor proteins p62/ SQSTM1 and NDP52 are recruited independently to bacteriaassociated microdomains to target Salmonella to the autophagy pathway. Autophagy 7, 22–26 54 Shahnazari, S. et al. (2010) A diacylglycerol-dependent signaling pathway contributes to regulation of antibacterial autophagy. Cell Host Microbe 8, 137–146 55 Kageyama, S. et al. (2011) The LC3 recruitment mechanism is separate from Atg9L1-dependent membrane formation in the autophagic response against Salmonella. Mol. Biol. Cell 22, 2290– 2300 56 Noda, T. et al. (2012) Three-axis model for Atg recruitment in autophagy against Salmonella. Int. J. Cell Biol. 2012, 389562 57 Rohde, K. et al. (2007) Mycobacterium tuberculosis and the environment within the phagosome. Immunol. Rev. 219, 37–54 58 van der Wel, N. et al. (2007) M. tuberculosis and M. leprae translocate from the phagolysosome to the cytosol in myeloid cells. Cell 129, 1287– 1298 59 Simeone, R. et al. (2012) Phagosomal rupture by Mycobacterium tuberculosis results in toxicity and host cell death. PLoS Pathog. 8, e1002507 60 Deretic, V. et al. (2009) Autophagy in immunity against Mycobacterium tuberculosis: a model system to dissect immunological roles of autophagy. Curr. Top. Microbiol. Immunol. 335, 169–188 61 Deretic, V. (2011) Autophagy in immunity and cell-autonomous defense against intracellular microbes. Immunol. Rev. 240, 92– 104 62 Ponpuak, M. et al. (2010) Delivery of cytosolic components by autophagic adaptor protein p62 endows autophagosomes with unique antimicrobial properties. Immunity 32, 329–341 Trends in Cell Biology xxx xxxx, Vol. xxx, No. x 63 Fabri, M. et al. (2011) Vitamin D is required for IFN-g-mediated antimicrobial activity of human macrophages. Sci. Trans. Med. 12, 104ra102 64 Kumar, D. et al. (2010) Genome-wide analysis of the host intracellular network that regulates survival of Mycobacterium tuberculosis. Cell 140, 731–743 65 Bruggemann, H. et al. (2006) Adaptation of Legionella pneumophila to the host environment: role of protein secretion, effectors and eukaryotic-like proteins. Curr. Opin. Microbiol. 9, 86–94 66 Isberg, R.R. et al. (2009) The Legionella pneumophila replication vacuole: making a cosy niche inside host cells. Nat. Rev. Microbiol. 7, 13–24 67 Joshi, A.D. and Swanson, M.S. (2011) Secrets of a successful pathogen: Legionella resistance to progression along the autophagic pathway. Front. Microbiol. 2, 138 68 Gutierrez, M.G. et al. (2005) Autophagy induction favours the generation and maturation of the Coxiella-replicative vacuoles. Cell. Microbiol. 7, 981–993 69 Beron, W. et al. (2002) Coxiella burnetii localizes in a Rab7-labeled compartment with autophagic characteristics. Infect. Immun. 70, 5816–5821 70 Romano, P.S. et al. (2007) The autophagic pathway is actively modulated by phase II Coxiella burnetii to efficiently replicate in the host cell. Cell. Microbiol. 9, 891–909 71 Moreau, K. et al. (2010) Autophagosomes can support Yersinia pseudotuberculosis replication in macrophages. Cell. Microbiol. 12, 1108–1123 72 Pujol, C. et al. (2009) Yersinia pestis can reside in autophagosomes and avoid xenophagy in murine macrophages by preventing vacuole acidification. Infect. Immun. 77, 2251–2261 73 Price, P.A. et al. (2012) Pulmonary infection by Yersinia pestis rapidly establishes a permissive environment for microbial proliferation. Proc. Natl. Acad. Sci. U.S.A. 109, 3083–3088 74 Celli, J. and Gorvel, J-P. (2004) Organelle robbery: Brucella interactions with the endoplasmic reticulum. Curr. Opin. Microbiol. 7, 93–97 75 Starr, T. et al. (2012) Selective subversion of autophagy complexes facilitates completion of the Brucella intracellular cycle. Cell Host Microbe 11, 33–45 76 Kim, H.K. et al. (2011) Recurrent infections and immune evasion strategies of Staphylococcus aureus. Curr. Opin. Microbiol. 15, 92–99 77 Schnaith, A. et al. (2007) Staphylococcus aureus subvert autophagy for induction of caspase-independent host cell death. J. Biol. Chem. 282, 2695–2706 78 Mestre, M.B. et al. (2010) a-Hemolysin is required for the activation of the autophagic pathway in Staphylococcus aureus infected cells. Autophagy 6, 110–125 79 Mijaljica, D. et al. (2011) Microautophagy in mammalian cells: revisiting a 40-year-old conundrum. Autophagy 7, 673–682 80 Arias, E. and Cuervo, A.M. (2011) Chaperone-mediated autophagy in protein quality control. Curr. Opin. Cell Biol. 23, 184–189 81 Husnjak, K. and Dikic, I. (2012) Ubiquitin-binding proteins: decoders of ubiquitin-mediated cellular functions. Annu. Rev. Biochem. (in press) 82 Laplante, M. and Sabatini, D.M. (2012) mTOR signaling in growth control and disease. Cell 149, 274–293 83 Rabinowitz, J.D. and White, E. (2010) Autophagy and metabolism. Science 330, 1344–1348 84 Pohl, C. and Jentsch, S. (2009) Midbody ring disposal by autophagy is a post-abscission event of cytokinesis. Nat. Cell Biol. 11, 65–70 85 Florey, O. et al. (2011) Autophagy machinery mediates macroendocytic processing and entotic cell death by targeting single membranes. Nat. Cell Biol. 13, 1335–1343 86 Youle, R.J. and Narendra, D.P. (2011) Mechanisms of mitophagy. Nat. Rev. Mol. Cell Biol. 12, 9–14 87 Sumpter, R. and Levine, B. (2011) Selective autophagy and viruses. Autophagy 7, 260–265 88 Orvedahl, A. et al. (2011) Image-based genome-wide siRNA screen identifies selective autophagy factors. Nature 480, 113–117 89 Itakura, E. and Mizushima, N. (2011) p62 targeting to the autophagosome formation site requires self-oligomerization but not LC3 binding. J. Cell Biol. 192, 17–27 90 Lamark, T. et al. (2003) Interaction codes within the family of mammalian Phox and Bem1p domain-containing proteins. J. Biol. Chem. 278, 34568–34581 9