* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download EO_Paper3_AtrialSeptalDefect
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Congenital heart defect wikipedia , lookup
Atrial septal defect wikipedia , lookup
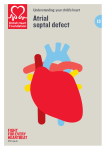
Dextro-Transposition of the great arteries wikipedia , lookup
Atrial Septal Defect Emily Otero December 6, 2016 Everybody hopes for a healthy baby, but the truth of the matter is that not everyone is fortunate enough to be born free of major adverse health condition at birth. Approximately 3-4% of almost four million children born in the United States every year are born with some sort of congenital abnormality. The term congenital refers to a condition existing at or prior to birth, and so congenital abnormalities are medical conditions present manifesting in a baby at or before birth that somehow deviate from what is expected from a conventionally healthy child. While congenital defects account for 20% of infant deaths in the United States, they do not necessarily indicate an urgent or life-threatening injury. However, they do require immediate treatment or supervision from doctors in order to ensure timely and appropriate treatment. Many children born with congenital defects must continue to see doctors into adolescence, and may stand a risk of developing complications from their congenital defect, or find themselves at higher risk for certain adverse medical conditions well into adulthood. Approximately one third of all children born with congenital defects are born with a heart defect of some kind or another. Heart defects are very diverse, and are associated with a variety of afflicted areas, symptoms, causes, risk factors, and consequences. Even the same kind of heart defect is experienced in radically different ways by different individuals, and may have resulted from different risk factors and may demand different ranges of treatment or maintenance for varying amounts of time. For this reason, instead of attempting to analyze a wide variety of heart defects for a limited understanding of a very broad range of issues, this paper will focus on examining many different aspects of a single heart defect – the atrial septal defect – in depth. DEFINITION In order to fully grasp the complications and symptoms that arise from the atrial septal defect, it is critical to understand the way a healthy human heart functions. The function of blood in the body is to provide a vessel with which to transport oxygen from the lungs to every cell in every corner of the body, so that this oxygen can be converted to energy for the cells to complete their individual functions. The heart serves a dual purpose: its pumping allows for the physical act of blood flow throughout the body, and the heart itself also serves as a crossroads to direct oxygen-rich and oxygen-poor blood out to the rest of the body or back to the lungs, respectively. The latter function can be easily visualized when taking into account the internal structure of the human heart, as seen in the figure below. The main body of the heart is divided into four chambers – two atria and two ventricles. The atria are situated in the top part of the heart, and collect blood flowing into the heart from other parts of the body, before being sent into the ventricles. The ventricles make up the lower part of the organ, and are responsible for pumping blood out of the heart (either to the lungs or to other parts of the body). The left and right halves of the heart are separated by a wall called the septum, which does not allow for blood to pass between the two halves, as each half is responsible for the handling of either oxygen rich blood or oxygen poor blood – never both. Thus blood cycles through the body in the following way: oxygen-rich blood flows into the left atrium of the heart from the lungs, then is passed into the left ventricle and then the aorta to be distributed to the rest of the body. Then, oxygen poor blood is returned to the heart, flowing into the right atrium, then is passed into the right ventricle and into the pulmonary artery to be oxygenized again by the lungs, and the cycle begins again. This process is outlined more clearly in the figure below. A labeled cross section of a healthy human heart including arrows that represent blood flow. Blue arrows represent the flow of blood with low levels of oxygen towards the lungs, and red arrows represent the flow of oxygen-rich blood as it moves from the lungs to the rest of the body. Image credit: National Heart, Lung, and Blood Institute official website (nhlbi.nih.gov) The important thing to understand in the context of an atrial septal defect is the presence of a clear separation between the left and right atriums in a healthy heart. It may be difficult to determine due to the positioning of the aorta and the pulmonary artery as being superimposed over the division between the two atria in the above diagram, but a healthy heart would have the septum that clearly divides the two ventricles and the two atria. This is made clearer in the diagram below, which has removed the representations of the superimposed aorta and pulmonary artery. Image credit: Fairview Ebenezer Health Library (http://www.fairviewebenezer.org/HealthLibrary/Article/89100) In prenatal development, it is perfectly normal for fetuses to have many openings along the septal wall prior to birth. These openings are a perfectly normal aspect of child development, and are not necessarily cause for concern. However, if these openings have not resolved themselves by the time the baby is born, they are classified as congenital heart defects and must be dealt with by a medical professional before the child can be released into the care of the parents, as they can cause serious health risks. Depending on where the hole is situated on the septal wall, three different defects, all posing different risks and demanding different treatments, can occur: if the hole exists in the division between the two ventricles, then it is a ventricular septal defect; if the hole exists in the division between the two atria, then it is an atrial septal defect (the focus of this paper); if the hole exists in the middle, affecting both the divisions between the ventricles and the atria, then it is an atrioventricular septal defect, and requires immediate surgical correction upon threat of death. Hearts with the atrial septal defect allow for the comingling of blood between both atriums. Specifically, oxygenized blood from the left atrium flows into the right atrium, mixing with the oxygen poor blood. The oxygenized blood in the right atrium is then passed into the right ventricle and sent straight back to the lungs through the pulmonary artery without having passed on any oxygen to other parts of the body, elevating the amount of oxygen present in the lungs and weakening them over time, as they are not used to the higher concentration of oxygen being presented to them. Additionally, there is now a higher amount of blood in the right atrium, resulting in a higher volume of blood being passed through the blood vessels around the lungs than is normal or expected, wearing down the strength of these blood vessels over time, leading to complications if the problem is left unresolved for long periods of time. Every instance of atrial septal defect is different, as the sizes of the holes present in the atrial septum may vary from case to case, and thus require different treatments and pose different threats to varying degrees of urgency. In general, there are four major types: The ostium primum atrial septal defect is, in actuality, associated with atrioventricular canal defects, and is characterized by a cleft in the mitral valve of the heart in the left atrium. The mitral valve operates as a “gate” that separates blood from the left atrium from the left ventricle, so as to not allow blood to flow from the ventricle into the aorta while still letting blood flow into the left ventricle. A cleft in this valve renders this capability null. The sinus venosus atrial septal defect is a defect that occurs in the right atrium, at the junction with the pulmonary veins that allow deoxygenated blood to flow into the heart. This results in abnormal drainage, and the flow of blood into the heart leaks into the left atrium. The coronary sinus atrial septal defect is when there is an opening in the coronary sinus in the right atrium, where the veins in the right atrium drain into the chamber proper. The ostium secundum atrial septal defect is the most common type. Approximately 70% of all children born with atrial septal defects are affected by this variety. It is characterized by the presence of a hole in the center of the atrial septal wall, an opening that never closed while the heart was still in neonatal development. A diagram of a heart with an atrial septal defect, with an arrow demonstrating the flow of oxygenized blood (represented by the red arrow and chambers) to deoxygenized areas (represented by the blue chambers). Image source: Centers for Disease Control and Prevention official website (cdc.gov) PREVALENCE Out of all the children born with congenital heart defects, approximately from 5 to 10% of children are diagnosed with the atrial septal defect. For every one thousand five hundred live births, one is detected with an atrial septal defect. Female babies are twice as likely to develop an atrial septal defect than male babies. The reasons for this are not yet understood. Likely due to the fact that atrial septal defects are often minor and sometimes asymptomatic, and can sometimes go undiagnosed until adverse health effects manifest themselves later in life, approximately 30 to 40 percent of congenital heart diseases present in surviving adults are atrial septal defects. DIAGNOSIS Identification of abnormal heart development is usually a focus in prenatal and very early childhood development. Medical professionals use ultrasounds to get a general picture of the health of the heart. This will usually portray the presence of a serious or obvious atrial septal defect. After birth, pediatricians will begin the regular process of auscultation, or the close listening of internal bodily functions through a stethoscope, at check-ups. They may notice palpitations or a heart murmur in the fetus, which will warrant further testing by a pediatric cardiologist. Further tests can include x-rays, which can tip doctors off to the presence of an atrial septal defect because of possible swelling in or enlargement of the heart as a result of the increased blood flow in the right half of the heart. Electrocardiograms measure electrical activity of the heart through the placement of plastic patches called electrodes on the surface of the skin of a child. Abnormal electrical readings may be symptomatic of muscle stress or arrhythmia, a type of abnormal heart rhythm. The presence of arrhythmia may be indicative of a congenital heart defect. Once the presence of such an anomaly is suspected, echocardiograms use ultrasound to capture a real-time, moving image of the heart and its internal structures, and can reveal more details about the specifics of the defect. It can visually depict information about the pattern of blood flow within the heart, and this information can be used to determine the size of the opening and the amount of blood passing through it. A much more invasive procedure called cardiac catheterization used only when the presence of the defect is practically confirmed and when more information about the specifics of how the heart is affected by the defect are needed in order to proceed with treatment. Cardiac catheterization requires the patient to be sedated as a flexible tube, the catheter, is guided by the cardiologist through the body into the heart, starting from a blood vessel in the groin. Not only does the tube make measurements of blood pressure and oxygen levels in each of the four chambers of the heart, but it also injects a dye to stain the inside walls of the heart, so that relevant structures are easier to discern from future less invasive techniques to see the heart. If the defect is not diagnosed early in development (a frequent occurrence, as the swelling of the heart and the presence of the heart murmur are usually only detected in very serious cases), the afflicted child may not realize there is a problem until they grow up and develop medical complications from the defect. Most instances of atrial septal defect are not urgent causes for medical concern and are often asymptomatic. The symptoms that do exist in some children are often mistaken for isolated incidents, or may resemble other heart or even mental conditions. Fatigue, shortness of breath after activities such as playing or feeding, arrhythmia, heart murmurs, poor physical growth, a susceptibility to respiratory infections are all exhibited symptoms of children who have atrial septal defects. Most people who discover the defect in adulthood realize it due to the presence of a heart murmur. CAUSES Causes of atrial septal defect are not largely understood, though there is reason to believe that some children may have a genetic predisposition to being born with a congenital heart defect. Atrial septal defects in particular are typically associated with Down syndrome (caused by an abnormality with the number of chromosomes passed down to a child). Women who consumed alcohol, drugs, or certain medications while pregnant, or women who suffered from a viral infection in the first trimester of pregnancy were also found to be more likely to have children with a congenital heart defect. COMPLICATIONS AND TREATMENT As mentioned above, when left untreated for long periods of time, the atrial septal defect can irreparably damage the heart and lungs by the time the individual is well into adulthood. Though such effects typically don’t manifest until after years of having the defect, swift and timely correction is preferred so as to minimize the risk of developing adverse effects through neglect. Some of these consequences include lung disease, exercise intolerance, shortened lifespan, and an increased risk of stroke. When detected prenatally or in young childhood, doctors often recommend leaving it alone to give it the chance to close on its own. In this case, the defect was simply a matter of belated cardiac development, and should be monitored throughout childhood and minded throughout life as part of a patient’s resolved medical history. If the defect does not seal itself on its own, cardiologists will resort to invasive surgeries to manually correct the defect. In some less serious cases of secundum atrial septal defects, the hole can be sealed through cardiac catheterization, in which the doctor uses the catheter to guide a device called the septal occluder into the opening and prevents the flow of blood through it. However, in more severe or complex cases, the patient may need to undergo open-heart surgery to close the opening with stitches or a patch, and to manage any damage that may have occurred in the heart as a result of the opening. Leading up to the procedures to close the heart, young children may be prescribed certain medications to help manage some of the side effects that result from atrial septal defect. Digoxin is prescribed in cases in which the heart has already been weakened from the stress, and is not pumping blood as efficiently as it should be as a result of the septal opening, and its purpose is to help the heart pump more blood per beat. Diuretics are prescribed when the kidneys are affected by the lower amounts of oxygen they are receiving from the blood, and help to maintain the proper water balance in the body by facilitating the removal of excess fluid through the weakened kidneys. Children born with atrial septal defects are more susceptible to bacterial infections in the inner surfaces of the heart, a condition known as bacterial endocarditis. The use of antibiotics may be prescribed if the patient will undergo an invasive procedure, such as surgery or cardiac catheterization to reduce the risk of infection. All in all, the concept of the atrial septal defect as an unpreventable hole in the heart of a child sounds much scarier than it is in most cases. The truth is that it is a manageable condition that can be easily corrected, provided that it is detected and diagnosed early in life. WORKS CITED "Atrial Septal Defect (ASD) in Children." Phoenix Children's Hospital Heart Center. Phoenix Children's Hospital, 19 Oct. 2016. Web. 05 Dec. 2016. "Birth Defects - Data & Statistics." Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, 21 Sept. 2016. Web. 05 Dec. 2016. "Birth Defects - Data & Statistics." Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, 21 Sept. 2016. Web. 05 Dec. 2016. "Birth Defects and Congenital Anomalies Symptoms & Causes." Boston Children's Hospital. Boston Children's Hospital, 2016. Web. 05 Dec. 2016. "Congenital Abnormalities." HealthyChildren.org. American Academy of Pediatrics, 21 Nov. 2015. Web. 05 Dec. 2016. "Congenital Anomalies." World Health Organization. World Health Organization, Sept. 2016. Web. 05 Dec. 2016. "Congenital Heart Disease Explained." WebMD. WebMD, 2016. Web. 05 Dec. 2016. "Data & Statistics - Congenital Heart Defects." Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, 07 Nov. 2016. Web. 05 Dec. 2016. "Facts about Atrial Septal Defect." Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, 14 Nov. 2016. Web. 05 Dec. 2016. Martin, Joyce A., MPH, Brady E. Hamilton, PhD, Stephanie J. Ventura, MA, Michelle JK Osterman, MHS, Elizabeth C. Wilson, MPH, and TJ Mathews, MS. "Births: Final Data for 2010." National Vital Statistics Reports 62.1 (2012): 1-72. Center for Disease Control and Prevention. Web. 5 Dec. 2016. "Types of CHD and Their Descriptions." Types of CHD and Their Descriptions. Baby Hearts Press, 19 Nov. 2013. Web. 05 Dec. 2016. Van Der Linde, Denise, Elisabeth EM Konings, Maarten A. Slager, Maarten Witsenburg, Willem A. Helbing, Johanna JM Takkenberg, and Jolien W. Roos-Hesselink. "Birth Prevalence of Congenital Heart Disease Worldwide: A Systematic Review and MetaAnalysis." Journal of the American College of Cardiology 58.21 (2011): n. pag. JACC Journals. Web. 5 Dec. 2016. "When Your Child Has a Ventricular Septal Defect (VSD)." When Your Child Has a Ventricular Septal Defect (VSD) - Ebenezer. Fairview Health Services, 2011. Web. 08 Dec. 2016.