* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Connective Tissue Disorders 61 Gene Panel
Cell-free fetal DNA wikipedia , lookup
Gene expression programming wikipedia , lookup
Frameshift mutation wikipedia , lookup
Site-specific recombinase technology wikipedia , lookup
Therapeutic gene modulation wikipedia , lookup
Genome (book) wikipedia , lookup
DNA paternity testing wikipedia , lookup
Gene therapy of the human retina wikipedia , lookup
Public health genomics wikipedia , lookup
Genetic testing wikipedia , lookup
Epigenetics of diabetes Type 2 wikipedia , lookup
Genealogical DNA test wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Point mutation wikipedia , lookup
Gene therapy wikipedia , lookup
Gene nomenclature wikipedia , lookup
Medical genetics wikipedia , lookup
Neuronal ceroid lipofuscinosis wikipedia , lookup
Saethre–Chotzen syndrome wikipedia , lookup
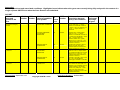
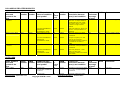
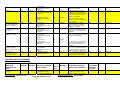
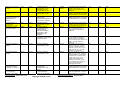
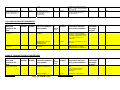
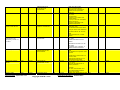
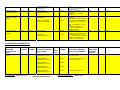
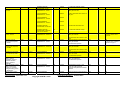
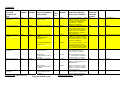
Proposal form for the evaluation of a genetic test for NHS Service Gene Dossier/Additional Provider Submitting laboratory: Sheffield RGC 1. Disorder/condition – approved name and symbol as published on the OMIM database (alternative names will be listed on the UKGTN website) If this submission is for a panel test please complete appendix 1 listing all of the conditions included using approved OMIM name, symbol and OMIM number. Connective Tissue Disorders - See appendix 1 2. OMIM number for disorder/condition If a panel test – see 1. above See appendix 1 3a. Disorder/condition – please provide, in laymen’s terms, a brief (2-5 sentences) description of how the disorder(s) affect individuals and prognosis. Connective tissue support organs and other parts of the body and can be described as the ‘biological glue’ that gives tissues form and strength, as well as helping them function. Connective tissue disorders often affect bones, muscles, and skin although organs such as the eyes, heart, lungs, kidneys, brain, gastrointestinal tract, and blood vessels can also be involved. Symptoms of a connective tissue disorder can include bone growth problems leading to deformity and brittle bones, skin symptoms including poor wound healing, kidney disease, brain lesions, and weak blood vessels that can easily rupture. These disorders can be severely disabling with pain and impaired mobility. In severe cases connective tissue disorders are life threatening and can lead to death shortly after birth. 3b. Disorder/condition – if required please expand on the description of the disorder provided in answer to Q3a. Alport syndrome is characterised by progress glomerulonephrities resulting in end stage renal failure. It is associated with haematuria, characteristic eye signs and sensorineral deafness. Collagen VI –related myopathies fall into the category of congenital muscular dystrophies and mainly affect skeletal muscles. Individuals with these conditions may experience progressive muscle weakness and develop contractures in the hands, wrists, elbows, and ankles. Mild respiratory muscle weakness is also present. Cutis Laxa is characterized by inelastic skin that is loose and sagging. Extremely wrinkled skin may be evident on the face and neck giving a droopy appearance, and in the armpits and groin. Cutis Laxa can also affect other organs, including the heart, joints, intestines, lungs and blood vessels including tearing of arteries. Diverticula can also develop in the walls of organs such as the bladder and intestines. Depending on which organs and tissues are affected, the signs and symptoms of cutis laxa can range from mild to life-threatening. Ehlers-Danlos Syndromes (EDS) are a group of disorders which share common features including easy bruising, loose joints, skin that stretches easily and weakness of tissues. The outlook for individuals with EDS depends on the type of EDS with which they have been diagnosed. Symptoms vary in severity, even within one sub-type, and the frequency of complications changes on an individual basis. Some individuals have negligible symptoms while others are severely restricted in their daily life. Vascular EDS can be life threatening due to rupture of hollow organs. Collagen IV -related disorders include: small-vessel brain disease of varying severity variably associated with porencephaly, cerebral aneurysms, eye defects and systemic findings. Small-vessel brain disease manifests as infantile hemiparesis, seizures, single or recurrent hemorrhagic stroke, ischemic stroke, and isolated migraine with aura. Familial Porencephaly is characterised by the presence of fluid-filled cavities in the brain, caused by antenatal and/or perinatal parenchymal haemorrhage. Brain Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 imaging shows porencephalic cysts, varying degrees of leucoencephalopathy, cerebral micro haemorrhage and lacunar infarct. The neurological symptoms vary in severity and age of onset. Typically affected individuals present with infantile hemiparesis, seizures, mental retardation, dystonia, stroke and migraine. Familial Thoracic Aortic Aneursym (FTAA) syndromes exhibit phenotypic overlap and diagnosis can be complicated by extensive phenotypic variability. They can be associated with a high morbidity and mortality rate. The most common inherited form of syndromic aneurysms is Marfan syndrome that presents with a wide range of clinical abnormalities including cardiovascular, skeletal, and ocular abnormalities. Other syndromic conditions include Loeys-Dietz Syndrome, vascular Ehlers-Danlos Syndrome , and Arterial tortuosity syndrome. Familial nonsyndromic aneurysms are characterized by aneurysms without the presence of other clinical manifestations and typically follow an autosomal dominant pattern of inheritance. Osteogenesis Imperfecta (OI) is characterised by low bone mass and an increased tendency to fracture, often with minimal or no apparent trauma. There is considerable variation in both severity and age of onset, which ranges from death in the perinatal period to very mildly affected individuals with few or no fractures. The clinical features of OI can include fractures, short stature with bone deformities, hyperlaxity of joints and skin, and Wormian bones. Extraskeletal symptoms such as blue sclerae, progressive adult hearing loss and dentinogenesis imperfecta may also be evident. Other important features are bone pain and impaired mobility. Stickler syndrome is a connective tissue disorder that can include ocular findings of high myopia, cataract, and retinal detachment; hearing loss that is both conductive and sensorineural; midfacial underdevelopment and cleft palate (either alone or as part of the Robin sequence); and mild spondyloepiphyseal dysplasia and/or precocious arthritis. Spinal abnormalities can include scoliosis or kyphosis and platyspondyly. 4. Disorder/condition – mode of inheritance If this submission is for a panel test, please complete the mode of inheritance for each condition in the table in appendix 1. See appendix 1 5. Gene – approved name(s) and symbol as published on HGNC database (alternative names will be listed on the UKGTN website) If this submission is for a panel test please complete appendix 1 listing all of the genes included using approved HGNC name, symbol, number and OMIM number. See appendix 1 6a. OMIM number(s) for gene(s) If a panel test – see 5. above See appendix 1 6b. HGNC number(s) for gene(s) If a panel test – see 5. above See appendix 1 7a. Gene – description(s) If this submission is for a panel test, please provide total number of genes. 61 genes: EDS -12 Bethlem Myopathy- 3 Alport- 3 Cutis Laxa- 7 Familial Porencephaly- 2 Familial Thoracic Aortic Aneurysms- 10 Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 Osteogenesis Imperfecta All- 16 Stickler- 8 7b. Number of amplicons to provide this test (molecular) or type of test (cytogenetic) (n/a for panel tests) 7c. GenU band that this test is assigned to for index case testing. Band G 50-100 amplicons –Collagen IV - related disorders Band H over 100 amplicons – Osteogenesis Imperfecta, Cutis Laxa, Ehlers Danlos Syndrome, Alports, Collagen VI- related myopathy, Familial Thoracic Aortic Aneurysm, Stickler 8. Mutational spectrum for which you test including details of known common mutations (n/a for panel tests) If this application is for a panel test to be used for different clinical phenotypes and/or various sub panel tests – please contact the team for advice before completing a Gene Dossier 9a. Technical method(s) – please describe the test. Clonal sequencing using the Illumina MiSeq platform. SureSelect Shearing of genomic DNA using the Covaris E220 sonicator. End repair, A tailing and ligation of adaptors using SureSelectXT library system (Agilent Technologies). Enrichment by SureSelect target enrichment (Agilent Technologies) using custom in house designed probes. Samples have barcode tags added following target enrichment. Sequencing on the Illumina MiSeq using the MiSeq Reagent Kit v2 performing 2 x 150 bp end paired reads. Data Analysis Bases on the open source ‘Best Practices’ workflow by the Broad Institute (for additional information, see http://www.broadinstitute.org/gatk/guide/best-practices). BWA alignment of reads to human genome build hg19. Generation of depth of coverage reports and checked using Alamut v 2.2 (Rev1) (Interactive Biosoftware). A minimum threshold of 30-fold read depth is set for exonic sequences and intronic sequences upto and including 5 bp from exon. A minimum threshold of 18-fold read depth is set for intronic sequences from 6 bp to 25 bp from exon together with a visual check of all reads. Identification of variants using HaplotypeCaller. Annotation from dbSNP and COSMIC (currently dbSNP138 and COSMIC v67 but updated with new releases) Variants filtered against in-house polymorphism lists and Best Practice Guidelines for the evaluation of pathogenicity and the reporting of sequence variants in clinical molecular genetics (Association for Clinical Genetic Science). Post analysis Confirmation of all clinically significant sequence variants by Sanger sequencing. Filling of all gaps with low depth of coverage by Sanger sequencing. Creation of a diagnostic report combining clonal and Sanger sequence data. 9b. For panel tests, please specify the strategy for dealing with gaps in coverage. Sanger sequencing is used to complete all gaps. 9c. Does the test include MLPA? (For panel tests, please provide this information in appendix 1) See appendix 1 Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 9d. If NGS is used, does the lab adhere to the Association of Clinical Genetic Science Best Practice Guidelines for NGS? Yes 10. Is the assay to be provided by the lab or is it to be outsourced to another provider? If to be outsourced, please provide the name of the laboratory and a copy of their ISO certificate or their CPA number. Assay is provided by the laboratory. 11. Validation process Please explain how this test has been validated for use in your laboratory or submit your internal validation documentation. If this submission is for a panel test, please provide a summary of evidence of: i) instrument and pipeline validation, and ii) panel verification for the test Please submit as appendices to the Gene Dossier (these will be included in the published Gene Dossier available on the website). Please note that the preferred threshold for validation and verification is 95% sensitivity with 95% Confidence Intervals. Validation of the Miseq analysis pipeline was carried out using 31 patient samples in whom a number of genes associated with glycogen storage disorders, connective tissue disorders, Fanconi anaemia and hereditary cancer had been analysed by Sanger sequencing. All 341 variants previously detected by Sanger sequencing were detected by the Miseq analysis pipeline. In addition, the Miseq analysis pipeline did not detect any false positive variants. The Connective Tissue Disorder (CTD) panel was validated by testing 7 patient samples for whom previous Sanger sequencing analysis was available for 14 CTD genes. 164 variants previously identified by Sanger sequencing were correctly identified. No false positive variants were reported by the Miseq analysis pipeline. The data obtained from the validation is above the preferred thresholds of 95% sensitivity with 95% confidence intervals. See attached validation documents 1 & 2. 12a. Are you providing this test already? Yes 12b(i). If yes, how many reports have you produced? 34 12b(ii). Number of reports mutation positive? 14 12b(iii). Number of reports mutation negative? 20 12b(iv). Please provide the time period in which these reports have been produced and whether in a research or a full clinical diagnostic setting. The service was moved from sanger sequencing to NGS on 4th November 2013. Thirty four reports have been issued via this pipeline. Testing for OI was established in 2002 and for EDS was introduced in 2009. Further connective tissue disorders have been developed over the last 5 years. More than 1000 reports have been issued for these conditions. All reports have been issued in a clinical diagnostic setting. 13a. Is there specialised local clinical/research expertise for this disorder? Yes Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 13b. If yes, please provide details Prof ACM Ong Professor of Renal Medicine Head, Academic Unit of Nephrology University of Sheffield Dr JA Cook Consultant Clinical Genetics Renal Genetics Clinic Department of Clinical Genetics Sheffield Children's NHS Foundation Trust Dr Glenda J Sobey Consultant Dermatologist EDS Specialist Clinic Dept of Clinical Genetics Sheffield Children's NHS Foundation Trust Dr Chris Rittey Consultant Paediatric Neurologist Sheffield Children's NHS Foundation Trust Dr Diana Johnson Consultant Clinical Genetics Department of Clinical Genetics Sheffield Children's NHS Foundation Trust Dr Meena Balasubramanian Consultant Clinical Geneticist Lead Consultant, OI-Genetics Service, NCG-OI Service Honorary Senior Clinical Lecturer University of Sheffield Sheffield Clinical Genetics Service Sheffield Children's NHS Foundation Trust Prof N Bishop Professor of Paediatric Bone Disease Heads of Metabolic Bone Disease Sheffield Children's NHS Foundation Trust 14. Based on experience what will be the national (UK wide) activity, per annum, for: Index cases: 965 Family members where mutation is known: 345 15. If your laboratory does not have capacity to provide the full national need please suggest how the national requirement may be met. For example, are you aware of any other labs (UKGTN members or otherwise) offering this test to NHS patients on a local area basis only? This question has been included in order to gauge if there could be any issues in equity of access for NHS patients. If you are unable to answer this question please write “unknown”. N/A 16. If using this form as an Additional Provider application, please explain why you wish to provide this test as it is already available from another provider. N/A Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 EPIDEMIOLOGY 17a. Estimated prevalence of conditions in the general UK population Prevalence is total number of persons with the condition(s) in a defined population at a specific time. Please identify the information on which this is based. For panel tests, please provide estimates for the conditions grouped by phenotypes being tested. Alport syndrome: 1/50,000 (http://ghr.nlm.nih.gov/condition/alport-syndrome) Collagen VI related Myopathy: Prevalence is estimated at 0.77:100,000 in Bethlem myopathy and 0.13:100,000 in Ullrich CMD (http://www.ncbi.nlm.nih.gov/books/NBK1503) Cutis Laxa: Prevalence for all types of cutis laxa is approximately 1:1,000,000 (http://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=GB&Expert=209) EDS: Classical EDS: 1/20,000 (Byers PH Disorders of collagen biosynthesis and structure Scriver, Beaudet, Sly, Valle eds The metabolic and molecular basis of inherited disease. 2 ed Edinburgh, UK Churchill Livingstone; 2001: 1065-81). Vascular EDS: 1/50,000-1/200,000 (Byers PH Gene Reviews) Many families with vascular EDS are only identified after a severe complication or death, therefore the prevalence may be higher. Kyphoscoliotic EDS: 1/100,000 (Yeowell NH, Steinmann B Gene Reviews) Combined 1/5000 (Genetics Home Reference- http://ghr.nlm.nih.gov/condition/ehlers-danlos-syndrome). Collagen IV-related disorders: Unknown as there is no data available (http://ghr.nlm.nih.gov/condition/familial-porencephaly) and only 17 families have been described (http://www.ncbi.nlm.nih.gov/books/NBK7046/) FTAA: Loeys-Dietz: Not known Marfan syndrome 1/5,000 (Orphanet- Prevalence of rare diseaseshttp://www.orpha.net/orphacom/cahiers/docs/GB/Prevalence_of_rare_diseases_by_alphabetical_list.pdf) TAAD 1/5,000-10,000 (http://ukgtn.nhs.uk/fileadmin/uploads/ukgtn/Documents/Resources/Library/Reports_Guidelines/UKGTN %20Workshop%20%20Marfan%20report%20%202012.pdf) OI: 1/15-20,000 (Forlino and Marini (2000) Mol Genet Metab 71: 225-32) Stickler: No studies to determine the prevalence of Stickler syndrome have been undertaken (http://www.ncbi.nlm.nih.gov/books/NBK1302) 17b. Estimated annual incidence of conditions in the general UK population Incidence is total number of new cases in a year in a defined population. Please identify the information on which this is based. For panel tests, please provide for groups of conditions. Alport: Not known Collagen VI related myopathy: There is no data available for specific incidence in the UK Cutis Laxa: Incidence for all types of cutis laxa is approximately 1:4,000,000 (http://www.ncbi.nlm.nih.gov/books/NBK5201) EDS: Individual incidence not known but combined EDS has an incidence of 1/5000 (Whitelaw SE; Ehlers-Danlos syndrome, classical type: case management. Dermatol Nurs. 2004 Oct;16(5):433-6, 449.) Collagen IV related disorders: Unknown as there is no data available FTAA: Loeys-Dietz: Not known Marfan Syndrome - 1/3,300 (http://ukgtn.nhs.uk/fileadmin/uploads/ukgtn/Documents/Resources/Library/Reports_Guidelines/UKGTN %20Workshop%20%20Marfan%20report%20%202012.pdf) Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 TAAD- 1/10,000 (http://ukgtn.nhs.uk/fileadmin/uploads/ukgtn/Documents/Resources/Library/Reports_Guidelines/UKGTN %20Workshop%20%20Marfan%20report%20%202012.pdf) OI: Types I, III, IV - 1/15-20,000 (Forlino and Marini (2000) Mol Genet Metab 71: 225-32) Type II – 1/50,000-60,000 (Baldridge et al (2008) Hum Mut 29(12): 1435-1442) Stickler: Approximate incidence of Stickler syndrome among newborns can be estimated from data regarding the incidence of Robin sequence in newborns (1:10,000-1:14,000) and the percent of these newborns who subsequently develop signs or symptoms of Stickler syndrome (35%). These data suggest that the incidence of Stickler syndrome among neonates is approximately 1:7,500-1:9,000 [Printzlau & Andersen 2004]. (http://www.ncbi.nlm.nih.gov/books/NBK1302) 18. Estimated gene frequency (Carrier frequency or allele frequency) Please identify the information on which this is based. n/a for panel tests. 19. Estimated penetrance of the condition. Please identify the information on which this is based n/a for panel tests 20. Estimated prevalence of conditions in the population of people that will be tested. n/a for panel tests. INTENDED USE (Please use the questions in Annex A to inform your answers) 21. Please tick either yes or no for each clinical purpose listed. Panel Tests: a panel test would not be used for pre symptomatic testing, carrier testing and pre natal testing as the familial mutation would already be known in this case and the full panel would not be required. Diagnosis Yes No Treatment Yes No Prognosis & management Yes No (n/a for Panel Tests) Yes No Carrier testing for family members (n/a for Panel Tests) Yes No Prenatal testing Yes No Presymptomatic testing (n/a for Panel Tests) Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 TEST CHARACTERISTICS 22. Analytical sensitivity and specificity This should be based on your own laboratory data for the specific test being applied for or the analytical sensitivity and specificity of the method/technique to be used in the case of a test yet to be set up. Please note that the preferred threshold for validation and verification is 95% sensitivity with 95% Confidence Intervals. Validation data for the Miseq analysis pipeline shows that the test sensitivity is >99% and test specificity is >99%. 23. Clinical sensitivity and specificity of test in target population The clinical sensitivity of a test is the probability of a positive test result when condition is known to be present; the clinical specificity is the probability of a negative test result when disorder is known to be absent. The denominator in this case is the number with the disorder (for sensitivity) or the number without condition (for specificity). Please provide the best estimate. UKGTN will request actual data after two years service. Clinical Sensitivity Alport- (http://ghr.nlm.nih.gov/condition/alport-syndrome) 15% will have mutations in COL4A3 or COL4A4 80% will have mutations in COL4A5 Collagen VI related Myopathy- (http://www.ncbi.nlm.nih.gov/books/NBK1503) COL6A1 = 38% COL6A2 = 44% COL6A3 = 18% Cutis Laxa 50-92% It is difficult to estimate the clinical sensitivity in patients with ADCL, as little literature is available. In ARCL, investigation of 12 pedigrees found mutations in 11 probands giving a sensitivity of 92%. We would expect the clinical sensitivity of this panel to be lower than this. EDS Classical EDS type 50–90% (COL5A1 and COL5A2 gene),which is genetically heterogeneous with additional, still unknown gene loci (Malfait F, Wenstrup RJ, De Paepe A (2010) Genet Med; 12: 597– 605; Symoens S et al (2012) Hum Mutat 33: 1485-1493. 95% for Vascular EDS (COL3A1 gene), (Germain DP (2007): Ehlers-Danlos syndrome type IV. Orphanet J Rare Dis 19: 2–32), arthrocholasic EDS (COL1A1 and COL1A2 gene, respectively) and kyphoscoliotic EDS (PLOD1 gene) (Rohrbach M et al (2011) Orphanet J Rare Dis 23: 6–46.) Sensitivity is not known in the recessively inherited clinical entities including Brittle Cornea syndrome 1 and 2 (ZNF469 and PRDM5 gene), D4ST1-deficient EDS (CHST14 gene), FKBP14-deficient EDS, dermatosparactic type (ADAMTS2 gene), EDS progeroid form (B4GALT7 gene) and EDS spondylocheiro dysplastic form (SLC39A13 gene). (Burkitt Wright EM et al, (2011) Am J Hum Genet 88: 767–777; Malfait F et al, (2010) Hum Mutat 31: 1233–1239; Baumann M et al, (2012) Am J Hum Genet 90: 201–216; Colige A et al, (2004) J Invest Dermatol 123: 656–663). Collagen IV related disorders Porencephaly has a variable phenotype and age of onset and as such this affects the clinical sensitivity. Not all mutation carriers have infantile porencephaly and hemiparesis, but have migraine or cerebral haemorrhage in adulthood. Combining both genes will increase the sensitivity FTAA Loeys-Dietz:The clinical sensitivity has been reported as 95% Loeys at al (2006) N Eng J Med 355(8): 788-98 Marfan syndrome : The clinical sensitivity has been reported as 90% in Marfan syndrome (Loeys et al (2004) Hum Mutat 24:140-6) with mutations primarily in FBN1 but up to 21% of mutations are found in Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 TGFBR2 (Saiki et al (2006) Am J Med Genet A 140(16):1719-25.; Mizuguchi et al (2004) Nat Genet 36(8):855-60) TAAD: ACATA2- 14% (Guo et al (2007) Nat Gen 36(12):1448-93; TGFBR2- 5% (Matyas et al (2006) Hum Mutat. 27(8):760-9 ; FBN1- unkown; TGFBR1- unknown Vasucular EDS 95% (see above) OI Dominant OI is approximately 85-90% and recessive OI is approximately 10-15% (http://www.oif.org/site/PageServer?pagename=fastfacts) Stickler- (http://www.ncbi.nlm.nih.gov/books/NBK1302) COL2A1 = 80-90% mutations COL11A1 = 10-20% mutations CO11A2, COL9A1, COL9A2, COL9A3 = rare 24. Clinical validity (positive and negative predictive value in the target population) The clinical validity of a genetic test is a measure of how well the test predicts the presence or absence of the phenotype, clinical condition or predisposition. It is measured by its positive predictive value (the probability of getting the condition given a positive test) and negative predictive value (the probability of not getting the condition given a negative test). Not currently requested for panel tests 25. Testing pathway for tests where more than one gene is to be tested sequentially Please include your testing strategy if more than one gene will be tested and data on the expected proportions of positive results for each part of the process. Please illustrate this with a flow diagram. This will be added to the published Testing Criteria. n/a for panel tests Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 CLINICAL UTILITY 26. How will the test change the management of the patient and/or alter clinical outcome? Please describe associated benefits for patients and family members. If there are any cost savings AFTER the diagnosis, please detail them here. General Accurate diagnosis allowing appropriate, effective treatment and improved surveillance. Identification and counselling of at risk relatives. First trimester prenatal diagnosis made possible. The availability of a panel test will result in a significant cost saving due to the removal of the need for sequential gene testing, biochemistry and possible need for skin/kidney/muscle/bone biopsy and will lead to a much quicker diagnosis for the patient. Alport The establishment of mode of inheritance is important in assessing the potential clinical outcome and therefore informs treatment and management strategies. In addition, testing of family members becomes available where either a molecular diagnosis is required for their clinical management/reproductive decisions or they wish to act as a living kidney donor. Collagen VI - related myopathy Collagen type VI-related disorders represent a continuum of overlapping phenotypes with Bethlem myopathy at the mild end, Ullrich congenital muscular dystrophy (CMD) at the severe end, and two rare, less well-defined disorders – autosomal dominant limb-girdle muscular dystrophy and autosomal recessive myosclerosis myopathy – in between. Although Bethlem myopathy and Ullrich CMD were defined long before their molecular basis was known, they remain useful for clarification of prognosis and management. Bethlem myopathy, characterized by the combination of proximal muscle weakness and variable contractures, affects most frequently the long finger flexors, elbows, and ankles. Onset may be prenatal (characterized by decreased fetal movements), neonatal (hypotonia or torticollis), in early childhood (delayed motor milestones, muscle weakness, and contractures), or in adulthood (proximal weakness and Achilles tendon or long finger flexor contractures). Because of slow progression, more than two thirds of affected individuals over age 50 years rely on supportive means for outdoor mobility. Respiratory involvement is rare and appears to be related to more severe muscle weakness in later life. Ullrich CMD is characterized by congenital weakness and hypotonia, proximal joint contractures, and striking hyperlaxity of distal joints. Some affected children acquire the ability to walk independently; however, progression of the disease often results in later loss of ambulation. Early and severe respiratory involvement may require ventilatory support in the first or second decade of life. Genotyping clarifies the inheritance pattern, provides some prognostic information and allows prenatal testing. Provides information on whether cardiac screening is required. Cutis Laxa Cutis laxa has several different forms. The effects of this condition are not only on the skin causing loose folds of wrinkled skin at an early stage, but can also affect the heart, blood vessels, joints, intestines and lungs. The bladder can also be affected. The signs and symptoms of cutis laxa can vary from mild to life threatening. Cutis laxa can be caused by mutations in a variety of genes. By knowing which gene is affected, patients can be appropriately managed according to the organ systems affected in that type. Inheritance in the family can also be accurately determined as this varies between the different types of cutis laxa. Presymptomatic testing to identify individuals at risk for cardiovascular and pulmonary disease is made available. EDS EDS describes a group of separate conditions with different genetics. These conditions need to be differentiated so that accurate diagnosis of subtype can lead to appropriate management. Some subtypes have a risk of sudden death and these patients need appropriate monitoring. The confirmation Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 of a subtype with no life threatening features means that further investigations and particularly expensive cardiovascular monitoring are not required. COL4A1-related disorders These include: small-vessel brain disease of varying severity variably associated with porencephaly, cerebral aneurysms, eye defects (retinal arterial tortuosity, Axenfeld-Rieger anomaly, cataract) and systemic findings (kidney involvement, muscle cramps, Raynaud phenomenon, and cardiac arrhythmia) Small-vessel brain disease manifests as infantile hemiparesis, seizures, single or recurrent hemorrhagic stroke, ischemic stroke, and isolated migraine with aura. Porencephaly(fluid-filled cavities in the brain detected by CT or MRI) is typically manifest as infantile hemiparesis, seizures, and intellectual disability; however, on occasion it can be an incidental finding. Hereditary Angiopathy with Nephropathy, Aneurysms, and muscle Cramps (HANAC) syndrome usually associates asymptomatic small-vessel brain disease, cerebral large vessel involvement (i.e., aneurysms), and systemic findings involving the kidney, muscle, and small vessels of the eye. Porencephalic cysts may occur after antenatal or neonatal parenchymal hemorrhagic infarction in the context of neonatal alloimmune thrombocytopenia, or a coagulopathy like von Willebrand disease, factor V or factor X deficiency, maternal warfarin use, or thrombophilia (most often heterozygosity for factor V Leiden mutation). It is important to differentiate familial porencephaly from these alternate causes as it affects pregnancy management and information given to families with regard to recurrence risk Cesarean delivery of fetuses at risk for a COL4A1-related disorder to prevent brain vascular injury resulting from birth trauma. Avoid anticoagulant use. FTAA Diagnosis of these conditions will allow for prompt appropriate and potentially life-saving treatment. Non-invasive screening for sites of arterial aneurysm may reduce morbidity and mortality. Affected individuals should be instructed to seek immediate medical attention for sudden unexplained pain. For some patients elective surgery may be discouraged due to increased tissue fragility resulting in a high risk of surgical complications. Pregnancy in women with these conditions can be associated with increased risk of death from peripartum arterial rupture or uterine rupture and should be managed in a high risk obstetric program. Osteogenesis Imperfecta Mutation analysis will confirm diagnosis of OI, inform the mode of inheritance and allow assessment of recurrence risk. In the event that an individual with a mild/moderate dominant mutation wishes to consider PND then recurrence risk is 50%. Mutation analysis in the affected individual would be required and allow reduction in late terminations or birth of affected children. Late prenatal testing is sometimes requested for delivery management. Molecular diagnosis also allows rapid predictive analysis of the newborn (2 weeks) and reduced parental anxiety. Severe OI can result from either a de novo dominant mutation where the risk of recurrence is associated with germline or somatic mosaicism in either parent, or recessive OI where there is a 25% recurrence risk. Though gonadal mosaicism cannot be tested for directly it is likely that absence of identifiable somatic mosaicism results in a reduced risk to the couple. Without mutation analysis each subsequent pregnancy may require ultrasound scans from 14-16wks onwards and in the event of an affected fetus, a late termination by induction of labour. There is also significant parental anxiety. OI is one of the rare genetic conditions where there is treatment available in the form of bisphosphonates which has dramatically changed the clinical outcome of patients with this condition. However, not being able to determine the genotype is difficult when trying to predict treatment outcomes, especially for patients with milder form of the condition. As a Clinician, it is important to ascertain the genotype so as to predict outcome, management implications and provide prognostic and recurrence risk information to patient and/or families. Stickler Testing with provide Individuals with a definitive diagnosis and this allows appropriate follow up which should include annual examination by a vitreoretinal specialist+/- prophylactic surgery; audiologic Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 evaluations every six months through age five years, then annually thereafter. Life style advice to reduce risk of complications. It will provide information on recurrence risk in families 27. If this test was not available, what would be the consequences for patients and family members? General : Can be difficult to assess potential clinical outcome and therefore develop appropriated monitoring and/or management plans, leading to poorer outcome. Lack of accurate identification of the mode of inheritance would not allow appropriate counselling of at risk family members and carrier, presymptomatic and prenatal testing is not possible. Alports syndrome: For this condition the inability to investigate carrier status may preclude family members from being live kidney donors. Collagen VI-related disorders: Patients with myopathy would not be differentiated into subtype. Unnecessary cardiac screening might occur. Prenatal diagnosis would then not be available. It would not be possible to determine if recurrence risk was < 1/200 or ¼ for simplex cases. Cutis Laxa Cutis laxa patients need to have the genetic basis of their condition determined otherwise under or over -management would be likely. Prenatal diagnosis would then not be available which is particularly important in the life threatening types. EDS: These patients would not be differentiated into subtype meaning that under or over -management would be likely. Prenatal diagnosis would then not be available which is particularly important in the life threatening types. Collagen IV-related disorders: Pregnancies might not be managed correctly and it would not be possible to give accurate information to families about recurrence. Prenatal testing would not be possible. FTAA: Appropriate organisation of elective surgery may not be possible without accurate diagnosis. The need for referral to high risk obstetric program may not be identified. Prompt and appropriate medical management may not be available. OI: Testing in OI to determine the genetic cause is important to provide information regarding recurrence risks, option of prenatal diagnosis especially with various patterns of inheritance that have been described. It alters clinical management in particular, decisions regarding therapeutic options especially in children with milder forms of bone fragility. Stickler syndrome caused by mutations in COL2A1, COL11A1, or COL11A2 is inherited in an autosomal dominant manner; Stickler syndrome caused by mutations in COL9A1 or COL9A2 is inherited in an autosomal recessive manner. In families with autosomal dominant inheritance, affected individuals have a 50% chance of passing on the mutation to each offspring. In families with autosomal recessive inheritance, each sib of an affected individual has a 25% chance of being affected, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier. Prenatal testing is possible in pregnancies at increased risk if the disease-causing mutation(s) in the family are known. In simplex cases if no mutation is identified it is not possible to give families accurate information with regards to recurrence risk, the possibility of severe eye phenotype or offer prenatal tests. 28. Is there an alternative means of diagnosis or prediction that does not involve molecular diagnosis? If so (and in particular if there is a biochemical test), please state the added advantage of the molecular test. Alport Syndrome: Renal biopsy (minimum cost £917), immunohistochemistry (£35 per antibody) of skin biopsy, ophthalmic assessment. Collagen VI related myopathy: Clinical assessment and muscle biopsy (£292) may suggest Bethlem vs Ullrich however there is considerable overlap in phenotype and only molecular genetic testing is Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 definitive. Cutis Laxa: There is no other accurate measure. Skin biopsy only demonstrates the reduction / absence of elastin but can not confirm the exact diagnosis or the affects on other organ systems. Only molecular diagnosis will allow prenatal diagnosis. EDS: There is no other accurate measure for EDS. Collagen species analysis can be used in Vascular EDS but not accurately in other types. Electron microscopy of skin biopsy can be undertaken but findings can be non specific and are not considered to be diagnostic. These methods would not allow prenatal diagnosis Collagen IV-related disorders: It is not possible to clinically distinguish familial porencephaly from the adult onset form of this condition which is autosomal dominant is very difficult to distinguish clinically from CARASIL which is autosomal recessive. FTAA: The only other method of diagnosis is by clinical evaluation using diagnostic criteria such as Ghent and Villfranche. However these conditons can have variable and overlapping clinical OI : Bone biopsy, which is highly invasive and needs to be performed under anaesthetic, does not provide adequate information for diagnosis and gives broad information on bone turn-over. Skeletal survey and DXA scans are used to type OI but this does not provide any information on the likely genetic cause. Urine NTx is used as a biochemical marker but again not specific enough and is more useful in monitoring response to treatment rather than being useful from a diagnostic point of view. Collagen analysis from skin biopsy has reduced positive and negative predictive value compared to genetic analysis due to subjective interpretation and lower sensitivity of assay. Electron microscopy of skin biopsy can be undertaken but findings can be non specific and are not considered to be diagnostic in isolation. Stickler: A small proportion of individuals with Stickler can be diagnosed on the basis of their eye phenotype. However there are only a very limited number of Ophthalmologists able to do this. 29a. What unexpected findings could this test show? For example, lung cancer susceptibility when testing for congenital cataract because ERCC6 gene (primarily associated with lung cancer) is included in a panel test for congenital cataract. The bioinformatics pipeline has been developed to enable the specific sub-panel relevant to the phenotype being investigated to be analysed. It is not therefore anticipated that there will be any unexpected findings. 29b. Please list any genes where the main phenotype associated with that gene is unrelated to the phenotype being tested by the panel. N/A 30. If testing highlights a condition that is very different from that being tested for, please outline your strategy for dealing with this situation. N/A 31. If a panel test, is this replacing an existing panel/multi gene test and/or other tests currently carried out through UKGTN using Sanger sequencing? If so, please provide details below. Sequential Sanger sequencing of some of the genes associated with Osteogenesis Imperfecta, Ehlers Danlos Syndrome, Alport Syndrome, Collagen VI-related myopathy, collagen IV related disorders and Stickler Syndrome are available. The Familial Thoracic Aortic Aneurysm panel incorporates Marfan syndrome, Loeys Dietz, vascular Ehlers Danlos Syndrome and familial Thoracic Aortic Aneurysm with Dissection. These are listed as single disorders on UKGTN. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 32. Please describe any specific ethical, legal or social issues with this particular test. IS IT A REASONABLE COST TO THE PUBLIC? 33. In order to establish the potential costs/savings that could be realised in the diagnostic care pathway, please list the tests/procedures that would be required in the index case to make a diagnosis if this genetic test was not available. Costs and type of imaging procedures Costs and types of laboratory pathology tests (other than molecular/cyto genetic test proposed in this Gene Dossier) Costs and types of physiological tests (e.g. ECG) Cost and types of other investigations/procedures (e.g. biopsy) Total cost of tests/procedures no longer required (please write n/a if the genetic test does not replace any other tests procedures in the diagnostic care pathway) Type of test Cost (£) Electron microscopy £350 Fibroblast culture £252.50 Collagen species analysis. £420 Sequential testing £1500 Skin biopsy gene £143 £2665.50 34. Based on the expected annual activity of index cases (Q14), please calculate the estimated annual savings/investments based on information provided in Q33. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 Number of index cases expected annually Cost to provide tests for index cases if the genetic test in this Gene Dossier was not available (see Q33) Total annual costs pre genetic test Total annual costs to provide genetic test Additional savings for 100% positive rate for index cases Percentage of index cases estimated to be negative Number of index cases estimated to be negative Costs to provide additional tests for index cases testing negative Total costs for tests for index patient activity (a) 965 (b) £2665.50 (a) x (b) = (c) £2,572,207 (a) x cost of genetic testing for index case = (d) £892,625 (d) – (c) = (e) -£1,679,582 (f) 50 (f) x number of index cases = (g) 482 (g) x (b) = (h) 482X1165= £561,771 Total costs for family members (e) + (h) = (i) -£1,679,528+£561,771 =£-1,117,757 Costs for family member test x number of family members expected to test in a year 345X155=£53,475 If there is a genetic test already available and some of the family testing is already being provided, please advise the cost of the family testing already available Cost for family member testing already available x estimated number of tests for family members already provided (k) 345X155=£53,475 Total costs for family members minus any family member testing costs already provided Additional savings for all activity expected in a year HSS Complex/Atypical EDS Service: testing for ~150 probands (£138,750). HSS Complex/Atypical OI : testing for 15 probands only (£13,875) (j) – (k) = (l) 0 (i) + (j) or (i) + (l) = £1,117,757 35. REAL LIFE CASE STUDY Please provide a case study that illustrates the benefits of this test 13-year female patient, 3rd child of healthy, non-consanguineous parents with no significant family history. Antenatally, there was no concerns identified and she was born at term. Following birth, she sustained several rib fractures prompting a diagnosis of OI. Skeletal survey pointed towards a diagnosis of type 3 OI. Genetic testing failed to identify a causative mutation in COL1A1 or COL1A2. She was followed up by the Metabolic Bone team in Sheffield and subsequently in Manchester for several years and has been on treatment with Pamidronate. This patient was seen in the OI-Genetics clinic under the auspices of the Severe/Complex OI service in Sheffield. Testing through the Next generation CTD panel identified a homozygous mutation in exon 1 CRTAP, thus confirming the diagnosis of OI but also providing accurate recurrence risks for this family who have older children of a child-bearing age. It also provided prognostic information for this patient and her family. This real life case study illustrates the clinical utility and advantages of accessing the OI panel test as part of the specialised services in Sheffield. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 TESTING CRITERIA 36. Please only complete this question if there is previously approved Testing Criteria. Please contact the UKGTN office if you are unsure whether testing criteria is available. 36a. Do you agree with the previously approved Testing Criteria? No 36b. If you do not agree, please provide revise Testing Criteria on the Testing Criteria form and explain below the reasons for the changes. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 UKGTN Testing Criteria Test name: Collagen VI Related Myopathy 3 Gene Panel Approved name and symbol of disorder/condition(s): Bethlem Myopathy Ullrich Congenital Muscular Dystrophy OMIM number(s): 158810 254090 Approved name and symbol of gene(s): collagen, type VI, alpha 1; COL6A1 collagen, type VI, alpha 2; COL6A2 collagen, type VI, alpha 3; COL6A3 OMIM number(s): 120220 120240 120250 Patient name: Date of birth: Patient postcode: NHS number: Name of referrer: Title/Position: Lab ID: Referrals will only be accepted from one of the following: Referrer Tick if this refers to you. Consultant Clinical Genetics Consultant Neurologist Consultant Paediatrician Minimum criteria required for testing to be appropriate as stated in the Gene Dossier: Criteria Tick if this patient meets criteria Myopathy phenotype with typical concentric signal abnormality on muscle MRI OR Reduced/absent collagen VI in muscle, OR Abnormal COL6 in fibroblast culture Additional Information: At risk family members where familial mutation is known do not require a full panel test but should be offered analysis of the known mutation If the sample does not fulfil the clinical criteria or you are not one of the specified types of referrer and you still feel that testing should be performed please contact the laboratory to discuss testing of the sample. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 UKGTN Testing Criteria Test name: Alport Syndrome 3 Gene Panel Approved name and symbol of disorder/condition(s): Alport Syndrome, Autosomal Dominant Alport Syndrome, Autosomal Recessive Alport Syndrome, X-Linked; ATS Benign Familial Haematuria Approved name and symbol of gene(s): collagen, type IV, alpha 3 (Goodpasture antigen); COL4A3 collagen, type IV, alpha 4; COL4A4 collagen, type IV, alpha 5; COL4A5 OMIM number(s): 104200 203780 301050 141200 OMIM number(s): 120070 120131 303630 Patient name: Date of birth: Patient postcode: NHS number: Name of referrer: Title/Position: Lab ID: Referrals will only be accepted from one of the following: Referrer Tick if this refers to you. Consultant Clinical Geneticist Consultant Nephrologist Consultant Ophthalmologist Consultant Paediatrician Minimum criteria required for testing to be appropriate as stated in the Gene Dossier: CriteriaTick if this patient At least 2 of the following criteria must be met by the proband: meets criteria Positive family history of haematuria or chronic renal failure Electron microscope evidence of Alport syndrome on renal biopsy High tone sensorineural deafness Characteristic ophthalmic signs (perimacular dots and flecks or anterior lenticous) OR Immunochemical evidence of loss of COL4A3 OR COL4A4 staining on a skin biopsy Additional Information: At risk family members where familial mutation is known do not require a full panel test but should be offered analysis of the known mutation If the sample does not fulfil the clinical criteria or you are not one of the specified types of referrer and you still feel that testing should be performed please contact the laboratory to discuss testing of the sample. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 UKGTN Testing Criteria Test name: Stickler 8 Gene Panel Approved name and symbol of disorder/condition(s): OMIM number(s): See appendix 1 See appendix 1 Approved name and symbol of gene(s): OMIM number(s): See appendix 1 See appendix 1 Patient name: Date of birth: Patient postcode: NHS number: Name of referrer: Title/Position: Lab ID: Referrals will only be accepted from one of the following: Referrer Tick if this refers to you. Consultant Clinical Geneticist Consultant Ophthalmologist Consultant Orthopaedist Minimum criteria required for testing to be appropriate as stated in the Gene Dossier: Criteria Tick if this patient meets criteria Skeletal abnormalities affecting joints e.g. hypermobility, joint pain, scoliosis, hyphosis, osteoarthritis etc AND Cleft palate (or family history of cleft palate) AND Sensori-neural hearing loss AND Normal vitreous phenotype Additional Information: At risk family members where familial mutation is known do not require a full panel test but should be offered analysis of the known mutation If the sample does not fulfil the clinical criteria or you are not one of the specified types of referrer and you still feel that testing should be performed please contact the laboratory to discuss testing of the sample. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 UKGTN Testing Criteria Test name: Cutis Laxa 7 Gene Panel Approved name and symbol of disorder/condition(s): Cutis Laxa: Occipital Horn Syndrome; Supravalvular Aortic Stenosis; Approved name and symbol of gene(s): See appendix 1 OMIM number(s): 614434 304150 185500 OMIM number(s): See appendix 1 Patient name: Date of birth: Patient postcode: NHS number: Name of referrer: Title/Position: Lab ID: Referrals will only be accepted from one of the following: Referrer Tick if this refers to you. Consultant Clinical Geneticist Consultant Paediatrician Consultant Dermatologist Consultant Cardiologist Consultant in Respiratory Medicine Minimum criteria required for testing to be appropriate as stated in the Gene Dossier: Criteria Tick if this patient meets criteria Loose/sagging/inelastic skin AND Emphysema OR Supravalvular Aortic Stenosis OR Radiological features of Occipital horn syndrome Additional Information: At risk family members where familial mutation is known do not require a full panel test but should be offered analysis of the known mutation. If the sample does not fulfil the clinical criteria or you are not one of the specified types of referrer and you still feel that testing should be performed please contact the laboratory to discuss testing of the sample. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 UKGTN Testing Criteria Test name: Osteogenesis Imperfecta 16 Gene Panel Approved name and symbol of disorder/condition(s): See appendix 1 OMIM number(s): See appendix 1 Approved name and symbol of gene(s): See appendix 1 OMIM number(s): See appendix 1 Patient name: Date of birth: Patient postcode: NHS number: Name of referrer: Title/Position: Lab ID: Referrals will only be accepted from one of the following: Referrer Tick if this refers to you. Consultant Clinical Geneticist Consultant Paediatrician Consultant in Bone Metabolism/Endocrinologist Consultant Neonatologist Minimum criteria required for testing to be appropriate as stated in the Gene Dossier: Criteria Tick if this patient meets criteria Multiple fractures of long bones without significant trauma AND at least two of the following: Wormian bones Blue/grey sclera Hearing loss Ribs, broad and beaded, thin and irregular Short stature Dentinogenesis imperfecta Triangular face and narrow thorax Round facies and short barrel-shaped chest Additional Information: At risk family members where familial mutation is known do not require a full panel test but should be offered analysis of the known mutation. If the sample does not fulfil the clinical criteria or you are not one of the specified types of referrer and you still feel that testing should be performed please contact the laboratory to discuss testing of the sample. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 UKGTN Testing Criteria Test name: Thoracic Aortic Aneurysms 10 Gene Panel Approved name and symbol of disorder/condition(s): See appendix 1 OMIM number(s): See appendix 1 Approved name and symbol of gene(s): See appendix 1 OMIM number(s): See appendix 1 Patient name: Date of birth: Patient postcode: NHS number: Name of referrer: Title/Position: Lab ID: Referrals will only be accepted from one of the following: Referrer Consultant Clinical Geneticist Tick if this refers to you. Consultant Cardiologist Consultant Ophthalmologist Consultant Paediatrician Minimum criteria required for testing to be appropriate as stated in the Gene Dossier: Criteria Tick if this patient meets criteria A patient should have at least one of the three following features: Dilated aortic root OR Tortuosity or aneurysm of other arteries OR Intestinal/uterine fragility or rupture AND Ectopia lentis OR Marfanoid habitus OR Excessive bleeding OR Characteristic facial appearance for one of these conditions including a decrease in subcutaneous adipose tissue, particularly face and limbs OR Positive family history, sudden death in a close relative Additional Information: At risk family members where familial mutation is known do not require a full panel test but should be offered analysis of the known mutation If the sample does not fulfil the clinical criteria or you are not one of the specified types of referrer and you still feel that testing should be performed please contact Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 UKGTN Testing Criteria Test name: Ehlers-Danlos 12 gene panel Approved name and symbol of disorder/condition(s): See appendix 1 OMIM number(s): See appendix 1 Approved name and symbol of gene(s): See appendix 1 OMIM number(s): See appendix 1 Patient name: Date of birth: Patient postcode: NHS number: Name of referrer: Title/Position: Lab ID: Referrals will only be accepted from one of the following: Referrer Tick if this refers to you. Consultant Clinical Geneticist Consultant Paediatrician Consultant Neurologist Consultant Dermatologist Minimum criteria required for testing to be appropriate as stated in the Gene Dossier: Criteria Tick if this patient meets criteria Skin hyperextensibility AND Joint hypermobility and laxity AND one of the following: Widening atrophic scars (tissue fragility) Easy bruising Muscle hypotonia Scoliosis Scleral fragility Additional Information: At risk family members where familial mutation is known do not require a full panel test but should be offered analysis of the known mutation If the sample does not fulfil the clinical criteria or you are not one of the specified types of referrer and you still feel that testing should be performed please contact Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 UKGTN Testing Criteria Test name: Familial Porencephaly 2 Gene Panel Approved name and symbol of disorder/condition(s): Porencephaly 1; Poren1 Porencephaly 2; Poren2 Brain Small Vessel Disease with Hemorrhage OMIM number(s): 175780 614483 607595 Approved name and symbol of gene(s): collagen, type IV, alpha 1; COL4A1 collagen, type IV, alpha 2; COL4A2 OMIM number(s): 120130 120090 Patient name: Date of birth: Patient postcode: NHS number: Name of referrer: Title/Position: Lab ID: Referrals will only be accepted from one of the following: Referrer Tick if this refers to you. Consultant Clinical Geneticist Consultant Paediatric Neurologist Consultant Neonatologist Consultant Neurologist Consultant in Stroke Medicine Minimum criteria required for testing to be appropriate as stated in the Gene Dossier: Criteria Tick if this patient meets criteria Evidence of familial porencephaly ie cysts or cavities within the cerebral hemisphere AND Hemiplegia, seizures and intellectual disability OR Close family history of familial porencephaly Additional Information: At risk family members where familial mutation is known do not require a full panel test but should be offered analysis of the known mutation If the sample does not fulfil the clinical criteria or you are not one of the specified types of referrer and you still feel that testing should be performed please contact the laboratory to discuss testing of the sample. Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 Appendix 1 Genes in panel test and associated conditions. Highlighted rows indicate where the gene was currently being fully analysed in the context of a single separate UKGTN test when the Gene Dossier was submitted. ALPORT HGNC standard name and symbol of the gene collagen, type IV, alpha 3 (Goodpasture antigen); COL4A3 collagen, type IV, alpha 4; COL4A4 collagen, type IV, alpha 5; COL4A5 HGNC OMIM number number OMIM standard name of condition and symbol Mode of inherit ance OMIM number Evidence of association between gene(s) and condition % of horizontal coverage of gene MLPA Comments 2204 ALPORT SYNDROME, AUTOSOMAL DOMINANT AD 104200 van der Loop et al. (2000) Kidney Int. 58: 1870-1875 – 1 unique variant in 6 individuals; Heidet et al. (2001) J. Am. Soc. Nephrol. 12: 97-106 - 1 unique variant in 2 individuals 100 NO Alport ALPORT SYNDROME, AUTOSOMAL RECESSIVE AR 203780 BENIGN FAMILAL HAEMATURIA AD 141200 ALPORT SYNDROME, AUTOSOMAL RECESSIVE AR 203780 100 NO Alport BENIGN FAMILAL HAEMATURIA AD 141200 Mochizuki et al. (1994) Nature Genet. 8: 77-81 - ; 3 unique variant in 3 individuals Lemmink et al. (1994) Hum Mol Genet 3: 12691273 - 1 unique variant in 1 individual; Gubler et al. (1995) Kidney Int. 47: 1142-1147 – 15% of Alport cases have mutations in COL4A3 or COL4A4 Bandenas et al (2002) J AM Soc Nephrol 13:1248-1254- 6/10 unrelated Spanish families had 2 different mutations in COL4A3 Mochizuki et al. (1994) Nature Genet. 8: 77-81- 1 unique variant in 1 individual; Gubler et al. (1995) Kidney Int. 47: 1142-1147 – 15% of Alport cases have mutations in COL4A3 or COL4A4 Lemmink et al (1996) J Clin Invest 98: 1114-1118- Identified a heterozygous mutation in COL4A4 ALPORT SYNDROME, XLINKED; ATS XL 301050 100 YES Alport 2206 2207 120070 120131 303630 Approval Date: September 2014 Knebelmann et al. (1996) Am. J. Hum. Genet. 59: 1221-1232 - 74 variants in 131 individuals giving a mutation detection rate of 50%; Renieri et al. (1996) Am. J. Hum. Genet. 58: 1192-1204 found causative mutations in 45% of 201 unrelated individuals Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 COLLAGEN VI RELATED MYOPATHY HGNC standard name and symbol of the gene HGNC OMIM number number OMIM standard name of condition and symbol Mode of inherit ance OMIM number Evidence of association between gene(s) and condition % of horizontal coverage of gene MLPA Comments collagen, type VI, alpha 1; COL6A1 2211 120220 BETHLEM MYOPATHY AD/AR 158810 Lucioli et al. (2005) Neurology 64: 1931-1937 – 8 unique variants in 16 individuals; Pan et al. (1998) Hum. Molec. Genet. 7: 807-812 – 1 variant in a large American pedigree 100 NO Type VI related myopathy AD/AR 254090 120240 ULLRICH CONGENITAL MUSCULAR DYSTROPHY; UCMD BETHLEM MYOPATHY AD 158810 Giusti et al (2005) Ann. Neurol. 58: 400-410 – 3 unique variants in 3 individuals Baker et al. (2007) Ann. Neurol. 62: 390-405 – 2 unique variants in 2 individuals 100 NO Type VI related myopathy ULLRICH CONGENITAL MUSCULAR DYSTROPHY; UCMD AD/AR 254090 BETHLEM MYOPATHY AD 158810 100 NO Type VI related myopathy ULLRICH CONGENITAL MUSCULAR DYSTROPHY; UCMD AD/AR 254090 Demir et al (2002) Am. J. Hum. Genet. 70: 1446-1458 – homozygous mutations in COL6A3 cause UCMD collagen, type VI, alpha 2; COL6A2 collagen, type VI, alpha 3; COL6A3 2212 2213 120250 Venegas et al (2001) Proc. Nat. Acad. Sci. 98: 7516-7521 demonstrated recessive mutations in COL6A2 are the cause of UCMD Baker et al. (2007) Ann. Neurol. 62: 390-405 – 2 unique variants in 2 individuals CUTIS LAXA HGNC standard name and symbol of the gene HGNC OMIM number number OMIM standard name of condition and symbol Mode of inherit ance OMIM number Evidence of association between gene(s) and condition % of horizontal coverage of gene MLPA Comments fibulin 5; FBLN5 3602 CUTIS LAXA, AUTOSOMAL DOMINANT 2; ADCL2; AD 614434 Callewaert et al (2013) Hum Mutat 34: 111-121 - 2 unique variants in 2 individuals 100 NO Cutis Laxa CUTIS LAXA, AR 219100 Loeys et al. (2002) Hum. Molec. 604580 Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 Elastin; ELN 3327 130160 EGF containing fibulinlike extracellular matrix protein 2; EFEMP2 3219 604633 ATPase, H+ transporting, lysosomal V0 subunit a2; ATP6V0A2 18481 611716 pyrroline-5-carboxylate reductase 1; PYCR1 9721 179035 latent transforming growth factor beta binding protein 4; LTBP4 6717 604710 ATPase, Cu++ transporting, alpha polypeptide; ATP7A 869 300011 AUTOSOMAL RECESSIVE, TYPE IA; ARCL1A CUTIS LAXA, AUTOSOMAL DOMINANT 1; ADCL1 Genet. 11: 2113-2118 - 1 unique variant in 4 individuals AD 123700 SUPRAVALVULAR AORTIC STENOSIS; SVAS AD 185500 CUTIS LAXA, AUTOSOMAL RECESSIVE, TYPE IB; ARCL1B CUTIS LAXA, AUTOSOMAL RECESSIVE, TYPE IIA; ARCL2A CUTIS LAXA, AUTOSOMAL RECESSIVE, TYPE IIB; ARCL2B AR 614437 AR 219200 AR 612940 CUTIS LAXA, AUTOSOMAL RECESSIVE, TYPE IIIB; ARCL3B AR 614438 CUTIS LAXA, AUTOSOMAL RECESSIVE, TYPE IC; ARCL1C OCCIPITAL HORN SYNDROME; OHS AR 613177 XL 304150 Szabo et al. (2006) 2 unique variants in a 3 generation family; Tassabehji et al. (1998) Hum Mol Genet 7: 1021-1028 - 1 unique variant in 1 individual Micale et al. (2010) 7 unique variants in 31 familal and sporadic cases of SVAS Hucthagowder et al. (2006) 1 unique variant in 1 individual; Dasouki et al. (2007) 2 unique variants in 1 individual Kornak et al. (2008) 10 unique variants in 12 families; Fischer et al. (2012) 14 unique variants in 13 individuals Reversade et al. (2009) Nature Genet 41: 1016- 1023 - 16 unique variants in 22 individuals Lin et al. (2011) 2 unique variants in 1 individual; Reversade et al. (2009) 16 unique variants in 22 individuals Callewaert et al (2013) Hum Mutat 34: 111-121 - 9 unique variants in 9 individuals; Urban et al. (2009) 5 unique variants in 4 individuals Kaler et al. (1994) 1 unique variant in1 individual; Tang et al. (2006) 1 unique variant in 2 individuals 100 NO Cutis Laxa 100 NO Cutis Laxa 100 NO Cutis Laxa 100 NO Cutis Laxa 100 NO Cutis Laxa 100 YES Cutis Laxa EHLERS DANLOS SYNDROME HGNC standard name and symbol of the gene HGNC OMIM number number OMIM standard name of condition and symbol Mode of inherit ance OMIM number Evidence of association between gene(s) and condition % of horizontal coverage of gene MLPA Comments collagen, type III, alpha 1; COL3A1 2201 EHLERS-DANLOS SYNDROME, TYPE IV, AUTOSOMAL DOMINANT AD 130050 https://eds.gene.le.ac.uk/home.ph p?select_db=COL3A1 ≥ 342 unique variants in 476 individuals 100 YES EDS/FTAA 120180 Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 collagen, type V, alpha 1; COL5A1 2209 120215 EHLERS-DANLOS SYNDROME, TYPE I; EHLERS-DANLOS SYNDROME, TYPE II EHLERS-DANLOS SYNDROME, TYPE I; AD 130000; 130010 collagen, type V, alpha 2; COL5A2 2210 120190 AD 130000 carbohydrate (Nacetylgalactosamine 4-0) sulfotransferase 14; CHST14 24464 608429 EHLERS-DANLOS SYNDROME, MUSCULOCONTRACTU RAL TYPE 1; EDSMC1 AR 601776 procollagen-lysine, 2oxoglutarate 5dioxygenase 1; PLOD1 FK506 binding protein 14, 22 kDa; FKBP14 9081 153454 AR 225400 18625 614505 AR 614557 Ras and Rab interactor 2; RIN2 18750 610222 EHLERS-DANLOS SYNDROME, TYPE VI; EDS6 EHLERS-DANLOS SYNDROME WITH PROGRESSIVE KYPHOSCOLIOSIS, MYOPATHY, AND HEARING LOSS; EDSKMH MACROCEPHALY, ALOPECIA, CUTIS LAXA, AND SCOLIOSIS AR 613075 PR domain containing 5; PRDM5 9349 614161 BRITTLE CORNEA SYNDROME 2; BCS2 AR 614170 zinc finger protein 469; ZNF469 23216 612078 BRITTLE CORNEA SYNDROME 1; BCS1 AR 229200 xylosylprotein beta 1,4galactosyltransferase, polypeptide 7 ; B4GALT7 930 604327 AR 130070 solute carrier family 39 (zinc transporter), member 13; SLC39A13 20859 608735 EHLERS-DANLOS SYNDROME, PROGEROID TYPE, 1; EDSP1 SPONDYLOCHEIRODYS PLASIA, EHLERSDANLOS SYNDROME- AR 612350 Approval Date: September 2014 https://eds.gene.le.ac.uk/home.ph p?select_db=COL5A1 ≥ 165 unique variants detected in 180 individuals https://eds.gene.le.ac.uk/home.ph p?select_db=COL5A2 ≥ 46 unique variants detected in 45 individuals https://eds.gene.le.ac.uk/home.ph p?select_db=CHST14 ≥ 12 unique variants detected in 17 individuals 100 YES EDS 100 NO EDS 100 NO EDS https://eds.gene.le.ac.uk/home.ph p?select_db=PLOD1 ≥38 unique variants detected in 65 individuals Baumann et al. (2012) Am. J. Hum. Genet. 90: 201-216 - 2 unique variants detected in 6 individuals 100 YES EDS 100 NO EDS 100 NO EDS/Cutis Laxa 100 NO EDS 100 NO EDS 100 NO EDS 100 NO EDS Basel-Vanagaite et al. (2009) Am. J. Hum. Genet. 85: 254-263 - 1 unique variant in 3 individuals ; Syx et al. (2010) Hum. Genet. 128: 79-88 - 1 unique variant in 3 individuals Aldahmesh et al. (2012) Clin. Genet. 81: 198-199 - 1 unique variant in 1 individual Burkitt Wright et al. (2011) Am. J. Hum. Genet. 88: 767-777 - 2 unique variants in 14 individuals Abu et al. (2008) Am. J. Hum. Genet. 82: 1217-1222 - 2 unique variants detected in 5 individuals Christensen et al. (2010) Invest. Ophthal. Vis. Sci. 51: 47-52 - 1 unique variant detected in 2 individuals; Khan et al. (2010) Arch. Ophthal. 128: 1376-1379 - 1 unique variants detected in consanguineous family https://eds.gene.le.ac.uk/home.ph p?select_db=B4GALT7 ≥ 3 unique variants detected in 2 individuals Giunta et al. (2008) Am. J. Hum. Genet. 82: 1290-1305 - 1 unique variants detected in 6 individuals Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 LIKE ADAM metallopeptidase with thrombospondin type 1 motif, 2; ADAMTS2 218 604539 EHLERS-DANLOS SYNDROME, TYPE VII, AUTOSOMAL RECESSIVE AR 225410 Fukada et al. (2008) PLoS One 3: e3642 - 1 unique variants detected in 2 individuals https://eds.gene.le.ac.uk/home.ph p?select_db=ADAMTS2 ≥ 20 variants detected 100 NO EDS COLLAGEN 4 RELATED DISORDERS HGNC standard name and symbol of the gene HGNC OMIM number number OMIM standard name of condition and symbol Mode of inherit ance OMIM number Evidence of association between gene(s) and condition % of horizontal coverage of gene MLPA Comments collagen, type IV, alpha 1; COL4A1 2202 PORENCEPHALY 1; POREN1 AD 175780 Gould et al. (2005) Science 308: 1167-1171 - 2 unique variants detected in 2 families; Breedveld et al (2005) J Med Genet 43: 490495 - 3 unique variants in 10 individuals 100 NO Type IV related disorders BRAIN SMALL VESSEL DISEASE WITH HEMORRHAGE PORENCEPHALY 2; POREN2 AD 607595 Sibon et al. Ann. Neurol. 62: 177184, 2007 AD 614483 Yoneda et al. (2012) Am. J. Hum. Genet. 90: 86-90 - 2 unique variants detected in 2 individuals 100 NO Type IV related disorders collagen, type IV, alpha 2; COL4A2 2203 120130 120090 FAMILAL THORACIC AORTIC ANEURYSMS HGNC standard name and symbol of the gene HGNC OMIM number number OMIM standard name of condition and symbol Mode of inherit ance OMIM number Evidence of association between gene(s) and condition % of horizontal coverage of gene MLPA Comments Actin, alpha 2, smooth muscle, aorta; ACTA2 130 AORTIC ANEURYSM, FAMILIAL THORACIC 6 AD 611788 Guo Nature Genet. 39: 1488-1493, 2007 14%of inherited ascending thoracic aneurysms and dissections. 100 No FTAA 613834 Milewicz Am. J. Med. Genet. 102620 MULTISYSTEMIC Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 SMOOTH MUSCLE DYSFUNCTION SYNDROME Fibrillin 1; FBN1 3603 134797 MARFAN SYNDROME AD 154700 myosin, heavy chain 11, smooth muscle; MYH11 7569 160745 AORTIC ANEURYSM, FAMILIAL THORACIC 4 AD 132900 solute carrier family 2 (facilitated glucose transporter), member 10; SLC2A10 filamin A, alpha; FLNA SMAD family member; SMAD3 Fibrillin 2; FBN2 13444 3754 6769 3604 606145 300017 603109 612570 ARTERIAL TORTUOSITY SYNDROME HETEROTOPIA, PERIVENTRICULAR, EDS VARIANT LOEYS-DIETZ SYNDROME, TYPE 3 CONTRACTURAL Approval Date: September 2014 AR 208050 X-linked AD AD 300537 613795 121050 152A: 2437-2443, 2010 Seven unrelated patients presenting with multisystemic smooth muscle dysfunction syndrome Comeglio et al. Hum. Mutat. 28: 928 , 2007. 508 individuals: 90 (82%) of 110 patients with 'classic' Marfan; 84 (27%) of 315 with 'incomplete Marfan phenotype; 19 (50%) of 38 patients with isolated ectopia lentis. Pannu Hum. Molec. Genet. 16: 2453-2462, 2007 Two kindreds with thoracic aortic aneurysm and/or aortic dissection. Zhu Nature Genet. 38: 343-349, 2006 Three probands from 3 TAAD families Couke J. Med. Genet. 40: 747751, 2003 Mutations identified in 6 ATS families Callewaert Hum. Mutat. 29: 150158, 2008 16 patients from 12 families, 11 different mutations identified. Sheen Neurology 64: 254-262, 2005 Two families and 9 sporadic cases reported. Gomez-Garre J. Med. Genet. 43: 232-237, 2006 Three female patients from a 3generation Spanish family Van de Laar J. Med. Genet. 49: 47-57, 2012 Data from 45 patients from 8 families presented. Regalado Circ. Res. 109: 680-686, 2011 Concludes SMAD3 mutations found in 2%of FTAA Frederic Hum Mutat 30(2) 181-190 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 100 Yes FTAA 100 No FTAA 100 No FTAA 100 No FTAA 100 No FTAA 100 No FTAA ARACHNODACTYLY, CONGENITAL transforming growth factor, beta 2; TGFB2 11768 190220 LOEYS-DIETZ SYNDROME, TYPE 4 transforming growth factor, beta receptor 1; TGFBR1 11772 190180 LOEYS DIETZ SYNDROME 609192 FAMILIAL THORACIC AORTIC ANEURYSMS 608967 transforming growth factor, beta receptor 2; TGFBR2 11773 190182 AD 614816 LOEYS-DIETZ SYNDROME, TYPE 1B 610168 LOEYS-DIETZ SYNDROME, TYPE 2B 610380 2009 Locus specific database ≥115 records provided. Lindsay Nature Genet. 44: 922927, 2012 86 individuals – 6 mutations identified Loeys New Eng. J. Med. 355: 788798, 2006 13 mutations identified in cohort of 80; 40 with typical manifestations, 40 with apparent vascular EDS. Singh Hum. Mutat. 27: 770-777, 2006 41 unrelated individuals 2 mutations in TGFBR1 and 5 in TGFBR2 identified Stheneur Hum Mutat. 2008;29:E284–95 Investigations in 457 patients with Marfan syndrome type I and II, Loeys-Dietz syndrome and related disorders - 23 TGFBR2 and 6 TGFBR1 mutations identifed 100 No FTAA 100 Yes FTAA 100 Yes FTAA OSTEOGENESIS IMPERFECTA HGNC standard name and symbol of the gene HGNC OMIM number number OMIM standard name of condition and symbol Mode of inherit ance OMIM number Evidence of association between gene(s) and condition % of horizontal coverage of gene MLPA Comments collagen, type I, alpha 1; COL1A1 2197 OSTEOGENESIS IMPERFECTA, TYPE I AD 166200 https://oi.gene.le.ac.uk/home.php? select_db=COL1A1 100 Yes OI/EDS OSTEOGENESIS IMPERFECTA, TYPE II 166210 ≥1360 individuals with OI listed with variants in this gene OSTEOGENESIS IMPERFECTA, TYPE III 259420 OSTEOGENESIS IMPERFECTA, TYPE IV 166220 EHLERS-DANLOS SYNDROME, TYPE VIIA 120150 120150 Approval Date: September 2014 6 individuals with EDS VIIA Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 collagen, type I, alpha 2; COL1A2 Cartliage-associated protein; CRTAP 2198 2379 120160 605497 EHLERS-DANLOS SYNDROME, TYPE I OSTEOGENESIS IMPERFECTA, TYPE I 130000 11 individuals OI/EDS overlap 166200 https://oi.gene.le.ac.uk/home.php? select_db=COL1A2 OSTEOGENESIS IMPERFECTA, TYPE II 166210 ≥798 OI individuals with variants in this gene OSTEOGENESIS IMPERFECTA, TYPE III 259420 OSTEOGENESIS IMPERFECTA, TYPE IV 166220 EHLERS-DANLOS SYNDROME, TYPE VIIB 120160 26 individuals with EDS VIIB AR 225320 11 individuals OI/EDS overlap AR 610682 https://oi.gene.le.ac.uk/home.php? select_db=CRTAP EHLERS-DANLOS SYNDROME, CARDIAC VALVULAR FORM OSTEOGENESIS IMPERFECTA, TYPE VII AD interferon induced transmembrane protein 5; IFITM5 1664 614757 OSTEOGENESIS IMPERFECTA, TYPE V AD 610967 Leucine proline-enriched proteoglycan (leprecan) 1; LEPRE1 19316 610339 OSTEOGENESIS IMPERFECTA, TYPE VIII AR 610915 ≥25 individuals with variants in this gene https://oi.gene.le.ac.uk/home.php? select_db=IFITM5 ≥32 individuals reported https://oi.gene.le.ac.uk/home.php? select_db=LEPRE1 ≥48 individuals with variants in this gene https://oi.gene.le.ac.uk/home.php? select_db=PPIB 100 Yes OI/EDS 100 No OI Formerly known as OI type IIB N/A No OI A single point mutation is report in OI type V 100 No OI 100 No OI 100 No OI peptidylprolyl isomerase B (cyclophilin B); PPIB 9255 123841 OSTEOGENESIS IMPERFECTA, TYPE IX AR 259440 serpin peptidase inhibitor, clade F (alpha-2 antiplasmin, pigment epithelium derived factor), member 1; SERPINF1 serpin peptidase inhibitor, clade H (heat shock protein 47), member 1, (collagen binding protein 1); SERPINH1 FK506 binding protein 10, 65 kDa; FKBP10 8824 172860 OSTEOGENESIS IMPERFECTA, TYPE VI AR 613982 1546 600943 OSTEOGENESIS IMPERFECTA, TYPE X AR 613848 Christiansen et al Am J Hum Genet 2010 86(3):389-98 Single severely affected individual reported. 100 No OI 18169 607063 OSTEOGENESIS IMPERFECTA, TYPE XI AR 610968 https://oi.gene.le.ac.uk/home.php? select_db=FKBP10 100 No OI Approval Date: September 2014 ≥12 individuals reported https://oi.gene.le.ac.uk/home.php? select_db=SERPINF1 ≥21 individuals reported Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 ≥48 individuals reported BRUCK SYNDROME 1 procollagen-lysine, 2oxoglutarate 5dioxygenase 2; PLOD2 Sp7 transcription factor; SP7 9082 601865 BRUCK SYNDROME 2 AR 609220 17321 606633 OSTEOGENESIS IMPERFECTA, TYPE XII AR 613849 transmembrane protein 38B; TMEM38B 25535 611236 OSTEOGENESIS IMPERFECTA, TYPE XIV AR 615066 wingless-type MMTV integration site family, member 1; WNT1 12774 164820 OSTEOGENESIS IMPERFECTA, TYPE XV 100 No There is clinical overlap between OI and Bruck syndrome. OI 100 No OI 100 No OI 100 No OI 100 No OI 100 No OI 100 No OI 259450 AR 615220 https://oi.gene.le.ac.uk/home.php? select_db=PLOD2 ≥10 individuals described Lapimzina et al 2010 Am J Hum Genet Case report Shaheen J. Med. Genet. 49: 630635, 2012 Three consanguineous families reported. Volodarsky et al Hum. Mutat. 34: 582-586, 2013 A further three consanguineous families KeuppAm. J. Hum. Genet. 92: 565-574, 2013 Three individuals from one family. Pyott Am. J. Hum. Genet. 92: 590597, 2013 Four families Fahiminiya J. Med. Genet. 50: 345-348, 2013 Three families bone morphogenetic protein 1; BMP1 1067 112264 Plastin 3; PLS3 9091 300131 cAMP responsive element binding protein 3-like 1 CREB3L1 18856 Not assigned OSTEOPOROSIS, EARLY-ONSET, SUSCEPTIBILITY TO, AUTOSOMAL DOMINANT OSTEOGENESIS IMPERFECTA, TYPE XIII X-LINKED OSTEOPOROSIS AND FRACTURES OSTEOGENESIS IMPERFECTA, TYPE III Approval Date: September 2014 615221 AR 614856 X-linked 300910 AR 259420 Laine New Eng. J. Med. 368: 1809-1816, 2013 Case study Asharani Am. J. Hum. Genet. 90: 661-674, 2012 Two affected sibs from consanguineous family. Martinez-Glez Hum. Mutat. 33: 343-350, 2012 Two sibs in consanguineous family Van Dijk New Eng. J. Med. 369: 1529-1536, 2013 Five families segregating Symoens Orphanet J Rare Dis 8;154 Case report Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 STICKLER HGNC standard name and symbol of the gene HGNC OMIM number number OMIM standard name of condition and symbol Mode of inherit ance OMIM number Evidence of association between gene(s) and condition % of horizontal coverage of gene MLPA Comments collagen, type XI, alpha 1; COL11A1 2186 120280 STICKLER SYNDROME, TYPE II; STL2 AD 604841 100 YES Stickler/Marshall collagen, type XI, alpha 2; COL11A2 2187 120290 STICKLER SYNDROME, TYPE III; STL3 AD 184840 100 NO Stickler collagen, type II, alpha 1; COL2A1 2200 120140 STICKLER SYNDROME, TYPE I, NONSYNDROMIC OCULAR AD 609508 Annunen et al. (1999) Am. J. Hum. Genet. 65: 974-983 - 15 unique variants in 15 individuals ; Majava et al. (2007) Am J Med Genet 143A:258–264 - 10 unique variants in 10 individuals Vikkula et al. (1995) Cell 80: 431437 - 1 unigue variant in a large Dutch kindred segregating with Stickler; Vuoristo et al. (2004) Am. J. Med. Genet. 130A: 160-164 - 1 unique variant in a 3 generation family with Stickler Richards et al. (2006) Hum. Mutat. 27: 696-704 - 3 unique variants in 3 families; McAlinden et al. (2008) Hum. Mutat. 29: 83-90 - 2 unique variants in 3 individuals 100 YES Stickler/Achondrogenesis STICKLER SYNDROME, TYPE I; STL1 AD 108300 STICKLER SYNDROME, TYPE IV; STL4 AR 614134 100 NO Stickler EPIPHYSEAL DYSPLASIA, MULTIPLE, 6; EDM6 STICKLER SYNDROME, TYPE V; STL5 AD 614135 AR 614284 100 NO Stickler EPIPHYSEAL DYSPLASIA, MULTIPLE, 2; EDM2 AD 600204 EPIPHYSEAL DYSPLASIA, MULTIPLE, 3; EDM3 AD 600969 100 NO Stickler collagen, type IX, alpha 1; COL9A1 collagen, type IX, alpha 2; COL9A2 collagen, type IX, alpha 3; COL9A3 2217 2218 2219 120201 120260 121270 Approval Date: September 2014 Annunen et al. (1999) Am. J. Hum. Genet. 65: 974-983 - 8 unique variants in 8 individuals; Richards et al. (2006) Hum. Mutat. 27: 696704 - 47 variants in 50 individuals Van Camp et al. (2006) Am. J. Hum. Genet. 79: 449-457 - 1 unique variant in 1 individual Czarny-Ratajczak et al. (2001) Am. J. Hum. Genet. 69: 969-9801 unique variant in 1 individual Baker et al. (2011) Am. J. Med. Genet. 155A: 1668-1672 – 1 unique variant segregating in a 5 generation family Fiedler et al. (2002) Am. J. Med. Genet. 112: 144-153 – 1 unique variant in 12 affected members of a 5 generation family Paassilta et al. (1999) Am. J. Hum. Genet. 65: 1214 – 1 unique variant in several affected members of a Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 procollagen-lysine, 2oxoglutarate 5dioxygenase 3; PLOD3 9083 603066 solute carrier family 26 (anion exchanger), member 2; SLC26A2 10994 606718 family with EDM3 https://eds.gene.le.ac.uk/home.ph p?select_db=PLOD3 ≥ 3 unique variants in 2 individuals BONE FRAGILITY WITH CONTRACTURES, ARTERIAL RUPTURE, AND DEAFNESS EPIPHYSEAL DYSPLASIA, MULTIPLE, 4; EDM4 AR 612394 AR 226900 Czarny-Ratajczak et al. (2001) Am. J. Hum. Genet. 69: 969-980 – 1 unique variant in 2 individuals; Ballhausen et al. (2003) J. Med. Genet. 40: 65-71 – 1 unique variant in 18 individuals from 12 families ACHONDROGENESIS, TYPE IB; ACG1B AR 600972 Superti-Furga et al. (1996) Nature Genet. 12: 100-102 – 6 variants in 6 individuals Approval Date: September 2014 Submitting Laboratory: Sheffield RGC Copyright UKGTN © 2014 100 NO Stickler 100 NO Stickler/Achondrogenesis