* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download HPI - iupui
Survey
Document related concepts
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiac surgery wikipedia , lookup
Aortic stenosis wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Electrocardiography wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Transcript
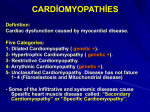
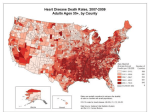
HPI 18 year old white male presents to the ED after passing out during his last basketball game as a high school senior. Patient recalls that the event occurred shortly after a steal and a fast break down the court. He remembers that after scoring he began to feel light headed and weak. The next thing he remembers is waking up on the court surrounded by all of his teammates, and the team nurse. 911 was called and he was immediately brought to you. He claims to feel fine now and appears relaxed. His mother is crying and keeps saying “this can’t be happening again.” What questions would you like to ask the patient and his family? • Pmhx: none, other then the occasional cold he reports being a healthy athletic kid • Allergies: none • Medications: none • Hospitalizations/Surgeries: Tonsillectomy at age 6. • Social: lives at home with parents and 2 sisters. Does not smoke, admits to occasional alcohol use on the weekends with 2 best friends. No illicit illegal drug use. • Family Hx: Mom with DM2, Dad with HTN controlled on HCTZ. – Mom crying because her brother at 16 died suddenly after collapsing on the football field. She said it had something to do with his heart, but no other information is known. • ROS: all negative. What is in your differential diagnosis at this time? • Syncope DDx: – Neuro: Stroke, embolus, ischemia, vasovagal – CV: arrhythmia, cardiomyopathy, ischemia, tamponade, aortic dissection, hemorrhage, valvular disease – Pulm: PE – Meds: think of those affecting conduction, long QT syndrome, anti-depressants – Misc: dehydrated, illicit drug use (something he is not telling you) • And many many more What is your next step to assess this patient? • Vitals Physical Exam – HR 68, BP 124/75 (sitting) 118/69 (standing), RR 18, T 37.3 • General: appears in no acute distress, sitting comfortably • CV: regular rate and rhythm, no rubs or gallops appreciated. Do appreciate a 2/4 systolic ejection murmur best heard over the left sternal border. When you have the patient stand up the murmur seems to worsen, when the patient is laying down though, the murmur decreases. • Pulm: CTA • Abd: wnl • Neuro: CN II-XII grossly intact, 5/5 strength bilaterally UE and LE. No numbness, tingling, loss of sensation • Psych: normal affect What to do next? Imaging? Labs? Send home? Labs/Tests • CBC: WBC 6000, Hgb 15.6, Hct 45%, Plt 200,000 • Chemistry Panel – Na 140, K 3.8, Cl 101, Bicarb 24, BUN 12, Cr 1.0, Glucose 94 • • • • • TSH: 2.7uU/mL (normal) Troponins : Negative Urine Drug Screen: Negative Head CT: Negative CXR: Normal Now ready to send home? Two things need to be done: 1) EKG 2) Echo- used if still unsure of diagnosis, or if need to visualize the heart Any thoughts now? Cardiomyopathy Three Main Types • Dilated Cardiomyopathy • Restrictive Cardiomyopathy • Hypertrophic Cardiomyopathy Hypertrophic Cardiomyopathy • Most common cause of Sudden Death in young individuals. • Sporadic and Familial forms exist • Sporadic Seen in the elderly while familial seen in young individuals • Familial noted to be autosomal dominant with nearly full penetrance. Use of ECG and Echo in HCM - Findings on 12-lead ECG are abnormal in 75-95% of HCM patients. Common abnormalities are LVH and widespread, deep, Q waves, which suggest an old MI. Many patients will have arrhythmias, both atrial and ventricular. ECG’s are useful principally for suggesting the possibility of HCM in relatives of HCM patients and in athletes undergoing pre-participation screening. (is used to screen all athletes in Italy for HCM, not yet used as a screening tool in the US) - Two-dimensional echocardiography is the usual method of diagnosis. Echocardiography can be used to confirm the size of the heart, the pattern of ventricular hypertrophy, the contractile function of the heart, and the severity of the outflow gradient. It has the advantages of high resolution and no known risk. Echocardiography has been used extensively both as an aid to diagnosis and for research into the pathophysiology of hypertrophic cardiomyopathy (HOCM). It is characterized by an abnormal arrangement of the myocardial cells, which instead of lying in parallel rows, form whorl-like patterns. It most commonly affects the interventricular septum, but may also involve the entire myocardium or occur in isolated areas undetectable except by detailed histopathologic examination. As shown in the above echo, the interventricular septum is enlarged, thus creating an outflow tract obstruction. Pathophysiology • Hypertrophy of the myocardium – Disproportionately greater hypertrophy of the interventricular septum then the LV free wall. – This may lead to an obstruction of the LV outflow tract below the aortic valve. – Leaflet of the mitral valve is drawn against the IVS which can lead to regurgitation – This hypertrophy of the LV leads to a restricted filling and therefore a DIASTOLIC dysfunction. • Syncope caused by the outflow obstruction • Sudden death due to ventricular tachycardia/fibrillation Enlarged interventricular septum leading to outflow tract obstruction This is a histological section of the conduction system in the septum which shows the aberrant myofibers Disarray and disorganization of myocardial fibers, showing abnormal branching, overlapping and hypertrophy, with interstitial plexiform fibrosis Common Clinical Findings • Harsh Systolic Ejection Murmur • Murmur intensity increases with a decreased preload (obstruction worsens). – Such as standing up, valsalva etc. • Murmur will decrease with an increased preload – The increased preload essentially opens the outflow tract – Therefore our treatment will be aimed at increasing the preload. And avoiding activities that increase the HR thereby reducing filling time. • Angina or Syncope are common due to the outflow obstruction Treatment • Avoid Strenuous Activity to avoid shortening filling time. • Avoid drugs that decrease the pre-load (diuretics) or increase the hearts force of contraction (digitalis). • Beta Blockers remain the mainstay of treatment. – By decreasing the HR you prolong diastole increase filling time and therefore increase preload – Also affective and decreasing myocardial contractility. • Defibrillator implantation – This may be a necessary procedure to prevent sudden cardiac death. What Next? • Screen All First Degree Relatives! • Stop all sports. Board Review Questions • Young teenager playing sports drops dead? Think Hypertrophic Cardiomyopathy • What part is most thickened? Interventricular Septum, this leads to an inwardly drawn mitral valve leaflet • Dysfunction? Mainly diastolic as the left ventricle is non compliant and therefore restricts filling. • Main treatment? Beta Blockers • http://www.ncbi.nlm.nih.gov/pubmedhealth/ PMH0001243/ • http://www.4hcm.org/ • http://www.heart.org/HEARTORG/Conditions/ More/Cardiomyopathy/HypertrophicCardiomyopathy_UCM_444317_Article.jsp • Goljan, Edward. Rapid Review Pathology, Elsevier 2009 Edition